The female reproductive tract develops from a pair of Müllerian ducts that form the fallopian tube, uterus, cervix, and the upper two-thirds of the vagina. The ovaries and lower third of the vagina have different embryological origins derived from germ cells that migrate from the primitive yolk sac and the sinovaginal bulb, respectively. Normal development of the Müllerian ducts depends on the completion of three phases: organogenesis, fusion, and septal resorption. Herlyn-Werner-Wunderlich (HWW) syndrome is part of a spectrum of Müllerian duct anomalies that occur during embryonic development.1
The syndrome is characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis.2 Only around 270 cases of this disease were reported worldwide. Imaging tests are relevant for adequate diagnosis, classification, and treatment.1 This case differs from the other reported cases due to pelvic pain secondary to infection and abscess in ureteric remnant. A search in the literature did not find any case with this clinical presentation.
Case report
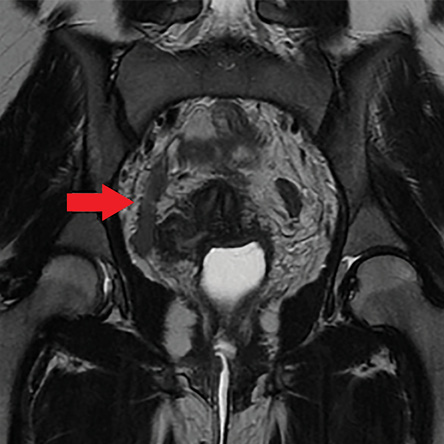
Figure 1: Computed tomography showing right renal agenesis (red arrow).
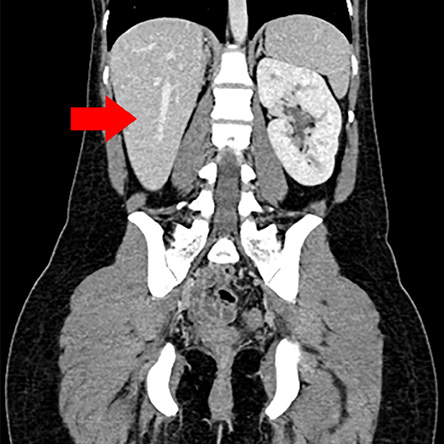
Figure 2: Coronal view showing tube-shaped formations (red arrow) extending from the right retrovesical region to the mesogastrium, without any conveyance with the vesical lumen.
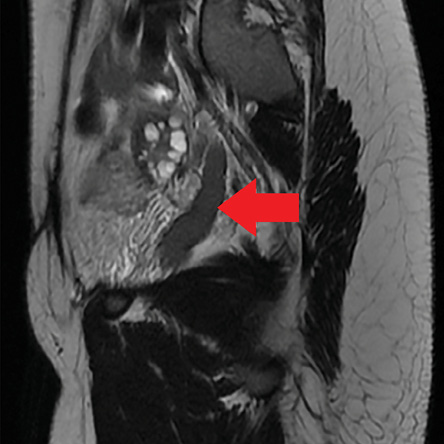
Figure 3: Sagittal view showing tube-shaped formations (red arrow) extending from the right retrovesical region to the mesogastrium, without any conveyance with the vesical lumen.
A 23-year-old female patient was presented at São Marcos Hospital with chronic pelvic pain for years, which worsened significantly in January 2013. The pain was intermittent and became more severe after sexual intercourse. The patient was diagnosed with HWW syndrome with a history of hematocolpos and vaginoplasty at the age of 12, and had undergone cesarean section at th age of 16. In June 2013, she sought urgent medical care due to intense pain, and a clinical picture suggestive of peritoneal irritation. Acute inflammatory pelvic disease was suspected and magnetic resonance imaging (MRI) showed a collection in the right adnexal region, consistent with hydrosalpinx. Clinical condition deteriorated and the patient underwent an exploratory laparotomy, which failed to identify anything to justify the abdominal pain. Retroperitoneal exploration was not performed. She remained hospitalized for seven days and received broad-spectrum antibiotics without any improvement. Urine culture and blood culture were negative. The patient continued to suffer intermittent pain until she experienced an acute episode of intense abdominal pain that was not resolved with common analgesics. The patient was referred to the urology service for further investigation. Cystoscopy was performed but did not identify the right ureteral ostium. Computed tomography (CT) showed right renal agenesis, left kidney with enlarged dimensions, and uterus didelphys [Figure 1]. MRI showed the same findings of CT and a 1.9 cm elongated cyst with hyperintense content on all pulse sequences, inferring protein content, and extending from the right retrovesical region to the mesogastric region, perhaps corresponding to the persistence of the mesonephric duct, related to ipsilateral renal
agenesis [Figures 2, 3, and 4].
The patient underwent laparoscopic procedure, identifying a right ureteric remnant blind ending, with distal and proximal obliteration, filled with purulent secretion, which was totally resected [Figure 5]. The patient was discharged from the hospital a day after the surgery. Histopathology revealed a hydroureter without signs of malignancy and culture positive for Escherichia coli. A urethral catheter was used during surgery, which was removed prior to hospital discharge. The patient was clinically free of symptoms at 14 months after surgery.
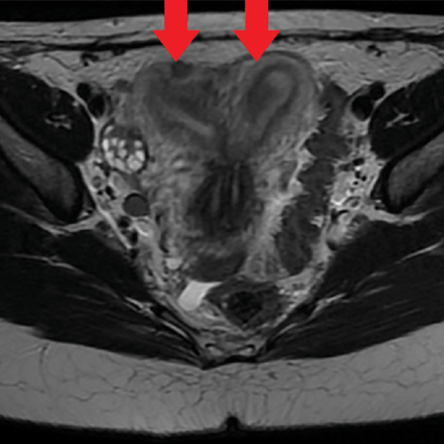
Figure 4: T2-weighted axial view showing uterus didelphys (red arrows).
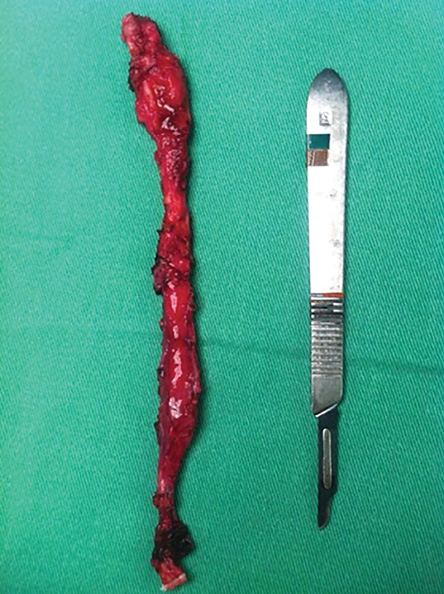
Figure 5: Surgical specimen.
Discussion
The incidence of anomalies related to the Müllerian ducts is 2−3% in the general population. Around 0.16−10% of these anomalies are responsible for the HWW syndrome, characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis.2−3
The case is normally diagnosed following an episode of postmenarche pelvic pain secondary to hematocolpos.2 Early diagnosis is imperative to prevent further complications related to urogenital anomalies that may lead to infertility. For detection of the condition, CT, ultrasonography, and MRI are the imaging tests used. However, laparoscopy may be useful when imaging tests are inconclusive.4,5 Of these tests, CT and ultrasonography are the most widely used diagnostic tools, although MRI is considered as the most sensitive imaging method for the evaluation of soft tissue anatomy and characterization of findings associated with anomalies. MRI is recommended before any surgical intervention.6
This syndrome may be accompanied by secondary complications such as endometriosis, infections, and pelvic adhesions. Furthermore, multiple alterations in the urinary tract may occur such as renal agenesis (more common and predominant on the right side), horseshoe kidney, pelvic kidney, cystic renal dysplasia, duplicated collecting system, and ectopic ureter. Thus, due to the intimate relationship between genital and urinary anomalies in females, urinary tract investigation is fundamental when there are genital anomalies and vice-versa.6
In this case report, the patient had already undergone surgery for correction of genital alterations related to the syndrome. Contrast-enhanced abdominal CT performed months ago have failed to identify any significant changes indicating the cause of the pain. Retrospectively, CT images were re-evaluated. An image of the right hydroureter was found, which was erroneously interpreted as hydrosalpinx in the first evaluation.
Since clinical conditions characterized by acute or chronic pelvic pain associated with the syndrome were generally determined by complications related to the genital tract, the main diagnostic hypothesis was endometriosis at a later date, due to persistent pelvic pain. MRI was ordered for further evaluation. Alterations identified in the illustrated case alerted to the possibility of changes in the urinary system that may be pain triggers in this clinical scenario. Therefore, imaging studies of the urinary tract are fundamental in paramesonephric duct anomalies, particularly in the HWW syndrome.
Conclusion
Up to the present, we failed to find any article in the literature reporting a case of HWW syndrome complicated by abscess in a ureteric remnant, which produced chronic pelvic pain. In this case, the ureter was removed and showed no signs of malignancy. The proximal third of the ureter was blind ending and the distal portion was atretic, preventing its drainage to the bladder and recognition by cystoscopy. Thus, appropriate diagnosis was critical for therapeutic planning and chronic pain resolution.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Chandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. Mullerian duct anomalies: from diagnosis to intervention. Br J Radiol 2009 Dec;82(984):1034-1042.
- 2. Cox D, Ching BH. Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolpos. J Radiol Case Rep 2012 Mar;6(3):9-15.
- 3. Bajaj SK, Misra R, Thukral BB, Gupta R. OHVIRA: Uterus didelphys, blind hemivagina and ipsilateral renal agenesis: Advantage MRI. J Hum Reprod Sci 2012 Jan;5(1):67-70.
- 4. Troiano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology 2004 Oct;233(1):19-34.
- 5. Madureira AJ, Mariz CM, Bernardes JC, Ramos IM. Case 94: Uterus didelphys with obstructing hemivaginal septum and ipsilateral renal agenesis. Radiology 2006 May;239(2):602-606.
- 6. Aveiro AC, Miranda V, Cabral AJ, Nunes S, Paulo F, Freitas C. Herlyn–Werner–Wunderlich syndrome: a rare cause of pelvic pain in adolescent girls. BMJ Case Rep 2011; 2011: bcr0420114147.