A 39-year-old unmarried woman was referred for evaluation following an incidental ultrasound finding of a 5 × 4 cm pelvic cyst with a thick hyperechoic wall. Otherwise, her gynecological, medical, and surgical history was unremarkable. Her clinical examination was unremarkable. She was mildly obese with a body mass index of 32. There was no abdominal tenderness or palpable masses. Bimanual vaginal examination was not performed (as is the custom in Muslim countries for unmarried women). Tumor markers cancer antigen (CA)-125, human chorionic gonadotropin, lactate dehydrogenase, and alpha-feto-protein were all negative. Magnetic resonance imaging (MRI) of the pelvis showed a normal uterus and endometrium [Figure 1]. Both ovaries were normal. There was a well-defined, irregular pelvic mass lesion, measuring 4.5 × 3.8 × 3.5 cm compressing the bladder dome, but not arising from it. It was of mixed signal intensity on T2-weighted images and was of relatively thick hypointense wall, could represent hemosiderin or calcification. There was a small amount of fluid in the solid mass that was not enhancing on postcontrast examination. There was no ascites or pelvic lymph node enlargement. The MRI concluded that it was a pelvic mass, with no clear attachment to any of the pelvic organs. The most likely possible differential diagnoses were: urachal cyst, degenerated pedunculated subserous fibroid, peritoneal inclusion cyst, and ovarian dermoid cyst.
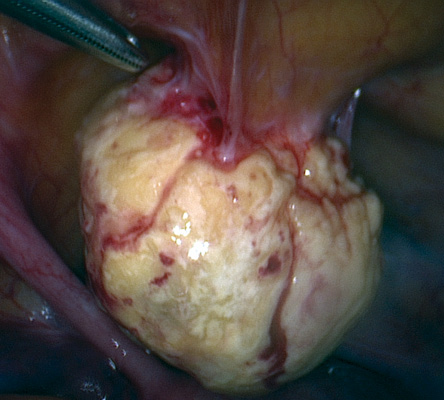
Figure 2: Laparoscopic image of the cyst intraoperatively.
She underwent laparoscopic exploration [Figure 2], which revealed a normal uterus, ovaries, and bladder. The lesion had a bony-hard shell and was rounded in shape and yellowish in color, arising at the midline of the anterior abdominal wall about 8 cm caudal to the level of the umbilicus. It was avascular, attached to the peritoneum and the preperitoneal fat. The lesion was excised completely. On laparoscopic retrieval, the shell had to be semi-crushed revealing an empty core. The patient had an uneventful recovery. Macroscopic pathology examination showed that the outer surface was rough and calcified. The cavity contained brown, cheese-like material. Microscopically, the cyst wall had dense calcification and focal ossification. The outer parts of the wall showed small foci of chronic inflammatory cells. No viable epithelial cell lining was detected. The lumen contained eosinophilic homogenous hyalinized material with many cholesterol clefts and red blood cells. There was no evidence of malignancy, and we concluded that it was a benign cystic lesion with extensive calcification, consistent with a densely calcified organized hematoma or calcified
fibrous cyst.
Pelvic cystic lesions are common in women mainly due to adnexal, ovarian, and fallopian tube cysts.1,2 Usually these pathologies are detected by ultrasound; however, in many instances, ultrasound is not able to clearly identify the origin of the cyst and MRI is used.3
When imaging can exclude adnexal origin, the differential diagnosis becomes wide and challenging. Although the medical literature is rich in clinical, radiological, and histological descriptions of those lesions it is still difficult at times to confirm the histological type of the lesion, and give a specific diagnosis.4–7 Preoperatively, face-to-face discussion between the surgeon and the reporting radiologist could help improve diagnostic accuracy and surgical planning.8 In our case, the list included the most likely differential diagnosis, but the histological description did not fit any of them. With those diagnostic limitations, the surgeon has to provide sufficient information to the patient preoperatively to obtain informed consent. The surgeon, general or gynecologic, also has to be prepared intraoperatively to manage all the likely possibilities. Postoperatively, especially when the histological study is unspecific, the surgeon has to provide the closest possible explanation of the findings to reassure the patient for future follow-up and prognosis.7
Disclosure
The authors declared no conflicts of interest.
Acknowledgements
The authors thank the patient and her family for cooperation in the matter of this publication.
references
- 1. Moyle PL, Kataoka MY, Nakai A, Takahata A, Reinhold C, Sala E. Nonovarian cystic lesions of the pelvis. Radiographics 2010 Jul-Aug;30(4):921-938.
- 2. Gowri V, Al Shukri M, Al Khaduri M, Machado L. Clinical and Histological Profile of Surgically Managed Benign Adnexal Masses. Oman Med J 2014;29(3):239-241.
- 3. Shetty MK. Adnexal Masses: Role of Supplemental Imaging with Magnetic Resonance Imaging. Seminars in Ultrasound, CT and MRI. 2016; 36(4): 369-384.
- 4. Arraiza Sarasa M, Ghai S, Metser U, Kennedy E, Vajpeyi R. A practical approach to cystic peritoneal masses and neoplasms: pearls and tips. Educational Exhibit. Congress ECR 2013:C-2522.
- 5. Levy AD, Arnáiz J, Shaw JC, Sobin LH. From the archives of the AFIP: primary peritoneal tumors: imaging features with pathologic correlation. Radiographics 2008 Mar-Apr;28(2):583-607, quiz 621-622.
- 6. Ashish P. Wasnik, Katherine E. Maturen, Ravi K. Kaza, Mahmoud M. Al-Hawary, Isaac R. Francis. Primary and secondary disease of the peritoneum and mesentery: review of anatomy and imaging features. Abdominal Imaging 2015; 40(3): 626-642.
- 7. Balaguera JC, Tórres SO, Almenta MM, Carneros VJ, Segovia JC, Gamarra LP, et al. Cystic Pathology Of The Abdominal Wall After Laparotomy: A Three-Case Report. The Internet Journal of Surgery 2005; 8(1).
- 8. Dickerson EC, Alam HB, Brown RK, Stojanovska J, Collaborative MR, Davenport MS. In-Person Communication Between Radiologists and Acute Care Surgeons Leads to Significant Alterations in Surgical Decision Making. J Am Coll Radiol 2016; 13(8):943-949.