|
Introduction
Small bowel obstruction (SBO) is a common cause of emergency surgical admissions.1,2 It is estimated that 60% of small bowel obstruction is due to postoperative adhesions.3 Traditionally, most of the patients with Adhesive (SBO) respond to conservative management. However, surgical intervention may be required in 20-30% of patients who develop serious complications such as strangulation, which can develop when surgery is delayed for more than 48 hours or do not respond to conservative treatment.4 Gastrografin (sodium diatrizoate, meglumine diatrizoate, schering, New Zealand) have been found to be helpful for predicting the outcome of obstruction.5 The aim of this study is to determine the role of gastrografin in predicting patients with adhesive small bowel obstruction who will respond to conservative treatment.
Methods
This prospective study was conducted between 1st August 2004 and 1st July 2006 at King Fahd University Hospital, Al Khobar, K.S.A. The study included 27 patients with 34 adhesive small bowel obstruction episodes who were admitted consecutively. The inclusion criteria were as follows: (a) clinical symptoms and signs compatible with small bowel obstruction including abdominal pain, distention, nausea, vomiting, abnormal bowel sounds and constipation and, (b) a plain abdominal radiograph showing dilated small bowel loops and air fluids levels. Patients were excluded if: (a) they had signs suggestive of intestinal strangulation present at admission including fever, intractable pain, leukocytosis or signs of peritonitis, (b) if the cause was something other than adhesions e.g. inflammatory bowel disease, external hernia, malignant disease or prior abdominal irradiation, (c) the obstruction developed within the first 4 weeks after abdominal surgery, (d) previously had total or subtotal colectomy, (e) allergy to iodine, and (f) pregnancy.
All patients had a thorough history and physical examination and were managed by intravenous hydration with Ringer’s lactate solution to correct dehydration and electrolyte imbalance. Nasogastric tube was inserted and after complete suction of gastric fluid, 100 ml of undiluted gastrografin was administered through the nasogastric tube after written informed consent was obtained, then the tube was clamped for 3 hours and the patient was kept in semi-sitting position. Planned abdominal radiography was taken at 6 hrs and 24 hrs. Patients with contrast reached colon were considered to have partial small bowel obstruction, thus the nasogastric tube was removed and the patients were given liquid diet followed by soft diet. Patients in whom gastrografin failed to reach the colon after 24 hours were considered to have complete small bowel obstruction and underwent laparotomy if there was no clinical or radiological improvement in the following 24 hours. The attending surgeon regularly assessed the patients’ condition during the hospital stay for any signs that would suggest the need for surgery. The patients were discharged when symptoms had resoleved and they were able to tolerate regular diet.
The data collected for each patient included: age, sex, type and time of previous operation, previous attack of intestinal obstruction, other medical illness outcome, hospital stay and surgical intervention.
Results
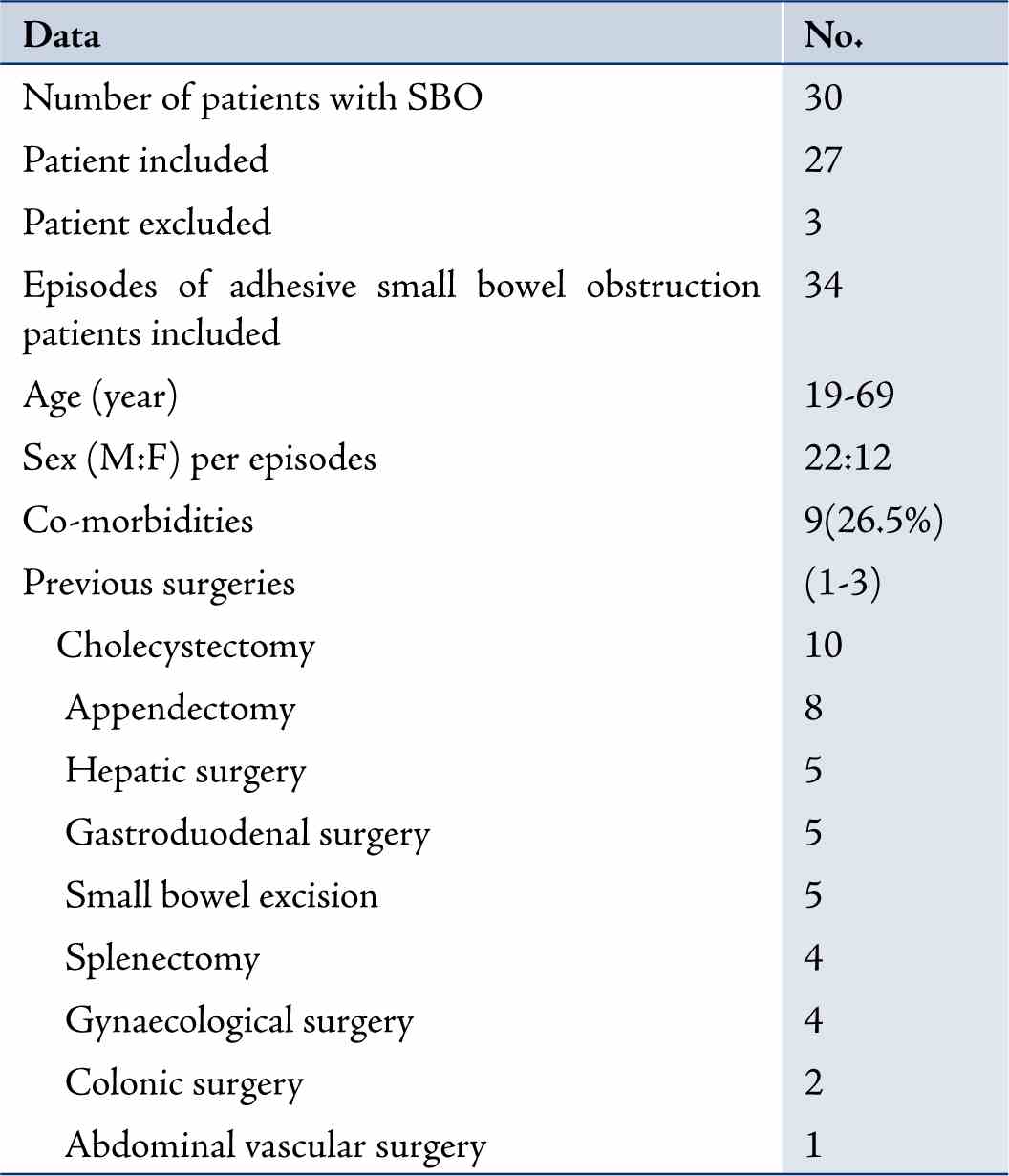
From August 2004 to July 2006, 27 patients with 34 episodes of adhesive small bowel obstruction were included in the study. Another three patients were excluded (mesenteric ischemia in 2 patients and one with colonic carcinoma presented with small bowel obstruction and had previous splenectomy). The mean age was 38.2 years (range: 19-69). Twenty-two patients were males and 12 females; and nine patients (26.5%) had associated medical illness. There were 44 previous operations, 28 patients had undergone a single previous abdominal operation. The most common operations were: Cholecystectomy and appendectomy (Table 1). Twenty-five patients were treated conservatively in 31 cases (91%). (Table 2)
Table 1: Demographic data of 27 patients adhesive small bowel obstruction.
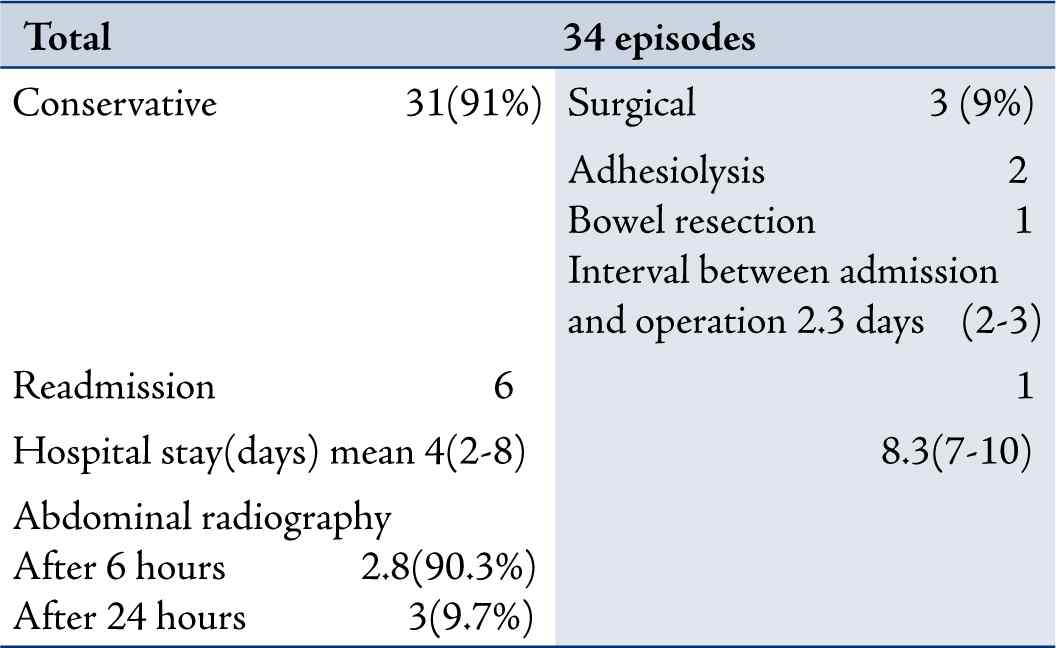
Four of them re-admitted twice and one was re-admitted three times. Repeated abdominal radiography showed gastrografin in the colon after 6 hours in 28 episodes (91.3%) and after 24 hours in (9.7%) while the mean hospital stay was 4 days (2-8). The only patient who stayed 8 days was diabetic and had hypertensive coronary artery disease and previous abdominal vascular occlusion operation. Three patients (9%) underwent laparotomy after gastrografin failed to reach the colon in the first 24 hours and no clinical improvement was observed in the next 24 hours (Table 2). Adhesiolysis was performed in two patients and small bowel resection in one patient. One patient was re-admitted with symptoms of small bowel obstruction and was managed conservatively. The time between admission and operation was planned in the protocol of the study after 48 hours, but one patient was delayed by one more day to control his blood sugar. The mean hospital stay was 8.3 days (7-10). All patients were discharged after resolution of their symptoms and once they tolerated oral feeding. No intra or postoperative complication and no mortality were reported. All the data analysis was done for the SBO cases.
Table 2: Outcome after administration of oral gastrografin.
Discussion
Adhesive small bowel obstruction is a common surgical problem but the optimal period of conservative treatment is of controversial issue before surgical intervention. Seror et al.6 reported that nonoperative management of up to 5 days duration can be used safely for the majority of patients with postoperative bowel obstruction. Hostetter suggested that small bowel obstruction should be treated surgically if obstruction is not resolved within 12 hours of conservative treatment.7 While Brolin and colleagues found that failure of conservative treatment requires prompt laparotomy usually within 24 hours.8
Sosa and Gardner found that patients with adhesive small bowel obstruction may be treated non-operatively for 24-48 hours, if no signs of strangulation are noted.9
However, Bizer et al. suggested that 48-72 hours is a sufficient period for non-operative management.10 The possibility of resolution of adhesive small bowel obstruction must be weighed against the need to decrease the complication of delayed surgery.11 The present study suggests that operation should be performed in patients in whom Gastrografin fails to reach the colon within 24 hours.
Different methods have been used to predict which patient will best benefit from non-operative treatment. Recent reports have indicated that abdominal computed tomography and ultrasonography may improve the diagnostic accuracy of bowel strangulation increasing the safety of conservative treatment. The use of gastrografin in the management of adhesive bowel obstruction has been evaluated in recent years.12
Gastrografin is a water-soluble contrast medium of high osmolarity composed of sodium diatrizoate, Meglumine amidotrizoate and wetting agent (polysorbate 80). The real value of gastrografin in this study was early detection of patients who could be confidently managed non-operatively. This study identified 91% of the patients who were treated conservatively.
Gastrografin may also have therapeutic effects in adhesive bowel obstruction because of its hyperosmolarity. Gastrografin also promotes shifting of fluid into the bowel lumen and increases the pressure gradient across the obstructing site.13 The bowel contents are diluted and in the presence of wetting agent, easier passage of the bowel content through narrowed lumen is allowed; thus gastrografin also decreases bowel wall edema, and enhances bowel motility.13-15
Furthermore, gastrografin is water soluble and relatively safe even if the obstruction is complicated by perforation. Complications from the use of gastrografin in small bowel obstruction are rare, although anaphylactoid reaction and lethal aspiration have been described.16,17 Gastrografin may also shorten postoperative ileus and relieve intestinal obstruction caused by impacted ascaris lumbricoides and bezoar.16-18 In this study, all patients with the contrast observed in the colon within 24 hrs were treated conservatively. On the other hand, surgery was performed in all the patients in whom the contrast failed to reach the colon within 24 hrs. There was no complication that could be attributed to the use of gastrografin in this study.
Conclusion
All patients with adhesive small bowel obstruction in whom the contrast reaches the colon in 6 hrs may be successfully treated conservatively as Gastrografin may have a therapeutic effect in addition to its diagnostic effect and permits early oral intake and discharge from hospital.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. McEntee G, Pender D, Mulvin D, McCullough M, Naeeder S, Farah S, et al. Current spectrum of intestinal obstruction. Br J Surg 1987 Nov;74(11):976-980.
2. Richards WO, Williams LF Jr. Obstruction of the large and small intestine. Surg Clin North Am 1988 Apr;68(2):355-376.
3. Roadley G, Cranshaw I, Young M, Hill AG. Role of Gastrografin in assigning patients to a non-operative course in adhesive small bowel obstruction. ANZ J Surg 2004 Oct;74(10):830-832.
4. Shih SC, Jeng KS, Lin SC, Kao CR, Chou SY, Wang HY, et al. Adhesive small bowel obstruction: how long can patients tolerate conservative treatment? World J Gastroenterol 2003 Mar;9(3):603-605.
5. Chung CC, Meng WC, Yu SC, Leung KL, Lau WY, Li AK. A prospective study on the use of water-soluble contrast follow-through radiology in the management of small bowel obstruction. Aust N Z J Surg 1996 Sep;66(9):598-601.
6. Seror D, Feigin E, Szold A, Allweis TM, Carmon M, Nissan S, et al. How conservatively can postoperative small bowel obstruction be treated? Am J Surg 1993 Jan;165(1):121-125, discussion 125-126.
7. Hofstetter SR. Acute adhesive obstruction of the small intestine. Surg Gynecol Obstet 1981 Feb;152(2):141-144.
8. Brolin RE, Krasna MJ, Mast BA. Use of tubes and radiographs in the management of small bowel obstruction. Ann Surg 1987 Aug;206(2):126-133.
9. Sosa J, Gardner B. Management of patients diagnosed as acute intestinal obstruction secondary to adhesions. Am Surg 1993 Feb;59(2):125-128.
10. Bizer LS, Liebling RW, Delany HM, Gliedman ML. Small bowel obstruction: the role of nonoperative treatment in simple intestinal obstruction and predictive criteria for strangulation obstruction. Surgery 1981 Apr;89(4):407-413.
11. Chen SC, Lin FY, Lee PH, Yu SC, Wang SM, Chang KJ. Water-soluble contrast study predicts the need for early surgery in adhesive small bowel obstruction. Br J Surg 1998 Dec;85(12):1692-1694.
12. Choi HK, Law WL, Ho JW, Chu KW. Value of gastrografin in adhesive small bowel obstruction after unsuccessful conservative treatment: a prospective evaluation. World J Gastroenterol 2005 Jun;11(24):3742-3745.
13. Caniano DA, Beaver BL. Meconium ileus: a fifteen-year experience with forty-two neonates. Surgery 1987 Oct;102(4):699-703.
14. Bar-Maor JA, de Carvalho JL, Chappell J. Gastrografin treatment of intestinal obstruction due to Ascaris lumbricoides. J Pediatr Surg 1984 Apr;19(2):174-176.
15. Stordahl A, Laerum F, Gjolberg T, Enge I. Water-soluble contrast media in radiography of small bowel obstruction: Comparison of ionic and non-inoic contrast. Media ACTA Radiol 1988;29:53-56.
16. Skucas J. Anaphylactoid reactions with gastrointestinal contrast media. AJR Am J Roentgenol 1997 Apr;168(4):962-964.
17. Trulzsch DV, Penmetsa A, Karim A, Evans DA. Gastrografin-induced aspiration pneumonia: a lethal complication of computed tomography. South Med J 1992 Dec;85(12):1255-1256.
18. Watkins DT, Robertson CL. Water-soluble radiocontrast material in the treatment of postoperative ileus. Am J Obstet Gynecol 1985 Jun;152(4):450-455.
|