| Introduction
Chronic rhinitis presents a tremendous and common problem for the healthcare industry. Cases can be classified into specific syndromes recognized mainly by a pattern of symptoms and to a lesser extent by physical signs. In patients complaining of nasal obstruction, rhinorrhea, and sneezing after allergy has been ruled out; these patients may be diagnosed with vasomotor rhinitis - a blanket term, further investigations and workup are generally abandoned by most clinicians, while treatment is indiscriminate and with a varied, unknown response rate. The Oto-Rhino- Laryngology Head and Neck Surgery (ORLHNS) literature is lacking with regards to management outcomes in patients with non-allergic rhinitis (NAR).1 Otolaryngology texts indicate the need for further epidemiological studies and research with reference to NAR.2
The term NAR is commonly applied to a diagnosis of any nasal condition in which the symptoms are identical to those seen in allergic rhinitis but an allergic etiology has been excluded.3 Recent literature defines NAR as a syndrome in which some combination of sneezing, rhinorrhea, nasal congestion, and post nasal drainage is present over time, in the absence of a specific etiology. Other terms for this condition include vasomotor rhinitis, idiopathic rhinitis, non-allergic, non-infectious rhinitis and intrinsic rhinitis.4
The present study describes the prevalence and clinical profile of NAR in a tertiary care hospital in Oman. The knowledge gaps in literature were also identified to direct future research.
Methods
A Cross sectional descriptive study was conducted of all 610 consecutive patients presenting to the ENT Clinic at Sultan Qaboos University Hospital - a tertiary care center in Oman. The study was approved by the University Medical Ethics and Research Committee. The study participants consisted of 113 patients diagnosed with chronic rhinitis. The diagnosis of NAR was based on a thorough clinical history. The diagnosis was mainly achieved by a process of exclusion in a stepwise fashion as previously described in otolaryngology texts.1-4 All males and females aged >18 years with a minimum duration of one year symptoms were included in the study.
Step 1- A complete history of symptomatology with regards to the onset of clinical conditions, timing of symptoms, exacerbating factors, environmental factors, systemic diseases, and use of drugs were obtained. The indicators for diagnosing NAR were; nasal symptoms like nasal obstruction, rhinorrhea, sneezing and the absence of positive allergy skin tests, or other forms of infective, allergic rhinitis.1-4 Specific history of the following was also obtained: the absence of identifiable aeroallergen triggers, the presence of concurrent allergic conditions, family history of allergic rhinitis, respiratory irritants such as smoking sheesha, and inducers of exacerbation, (Fig. 1). Laryngopharangeal reflux was also excluded.4
The distinguishing clinical features included nasal symptoms such as; nasal obstruction, rhinorrhea, sneezing postnasal drip, nasal irritation, anosmia, sleep disturbance, and fatigue. The subjective severity was recorded and each symptom was evaluated on the following scale: 0 = absent; 1 = Mild, (symptom was present but not annoying or troublesome); 2 = Moderate (symptom was frequently troublesome but did not interfere with normal activity or sleep; and 3 = Severe (symptom interfered with activities and sleep).
Step 2- A through physical examination was performed including a nasal endoscopy to exclude mechanical causes such as deviated nasal septum. A complete head and neck examination was also done, including: fogging test (by placing a steel spatula and observing the fogging produced by expired air and comparing right and left side, and the test was considered positive if no fogging was present in one side); Cottles test; and nasal endoscopies were performed to observe the following; nasal septum, degree of deviation, mucus membrane (mucosal edema, congestion), the presence of nasal discharge, endoscopic observation of inferior turbinate (hypertrophy), and shrinking of the turbinate after application of ephedrine 1% solution, as well as the external and internal nasal valve and middle meatus. An allergy skin test and CT of the Sinuses were done on all patients as part of the diagnostic protocol.
Step 3- Exclusion of allergic rhinitis by allergy skin testing of all patients.
Step 4- Computed Tomography to exclude sinusitis. Step 5- Clinical trial of antihistamines; Lack of response to antihistamines (patients reporting no clinical improvement in symptoms) was the final indicator of diagnosis.
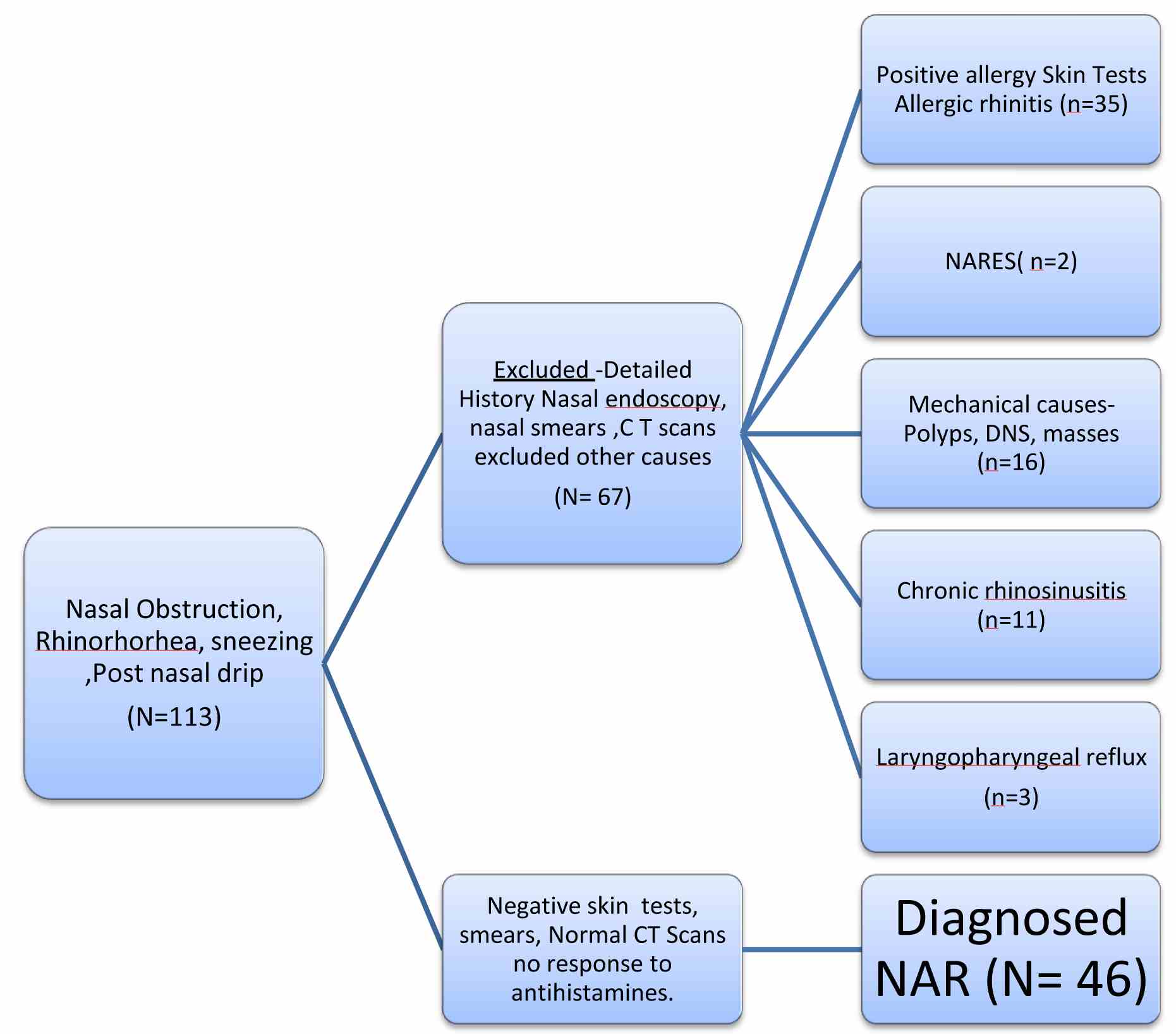
Figure 1: Shows the diagnosis algorithm and the patients excluded and included in the study.
In the knowledge gap study, primary research articles and meta-analysis evaluated for this study were identified through MEDLINE search of English language literature published between 2000 and 2011. The search targeted systematic reviews, meta-analysis, and diagnostic studies, as well as prevalence studies. The search also included hand search of the literature in the most recent otolaryngology text books, and the knowledge gaps were thus identified.
Statistical analysis was done using the SPSS package (version 13.0). The demographic data, clinical profile data were expressed as percentages.
Results
A total of 610 consecutive patients studied. The overall prevalence of rhinitis was 18.5% (n=113). The prevalence of NAR was 7.5% (n=46); while in the excluded cases, allergic rhinitis was 5.7% (n=35), Chronic rhinosinusitis was 1.8% (n=11), and miscellaneous causes were 3.4% (n=21). Among the rhinitis population (n=113), the prevalence of NAR was 57% (n=46). The major presenting symptoms included nasal obstruction 93% (n=43), postnasal drainage 78% (n=36), and rhinorrhea 62% (n=29). The exclusion and the prevalence of NAR are presented in Fig. 2.
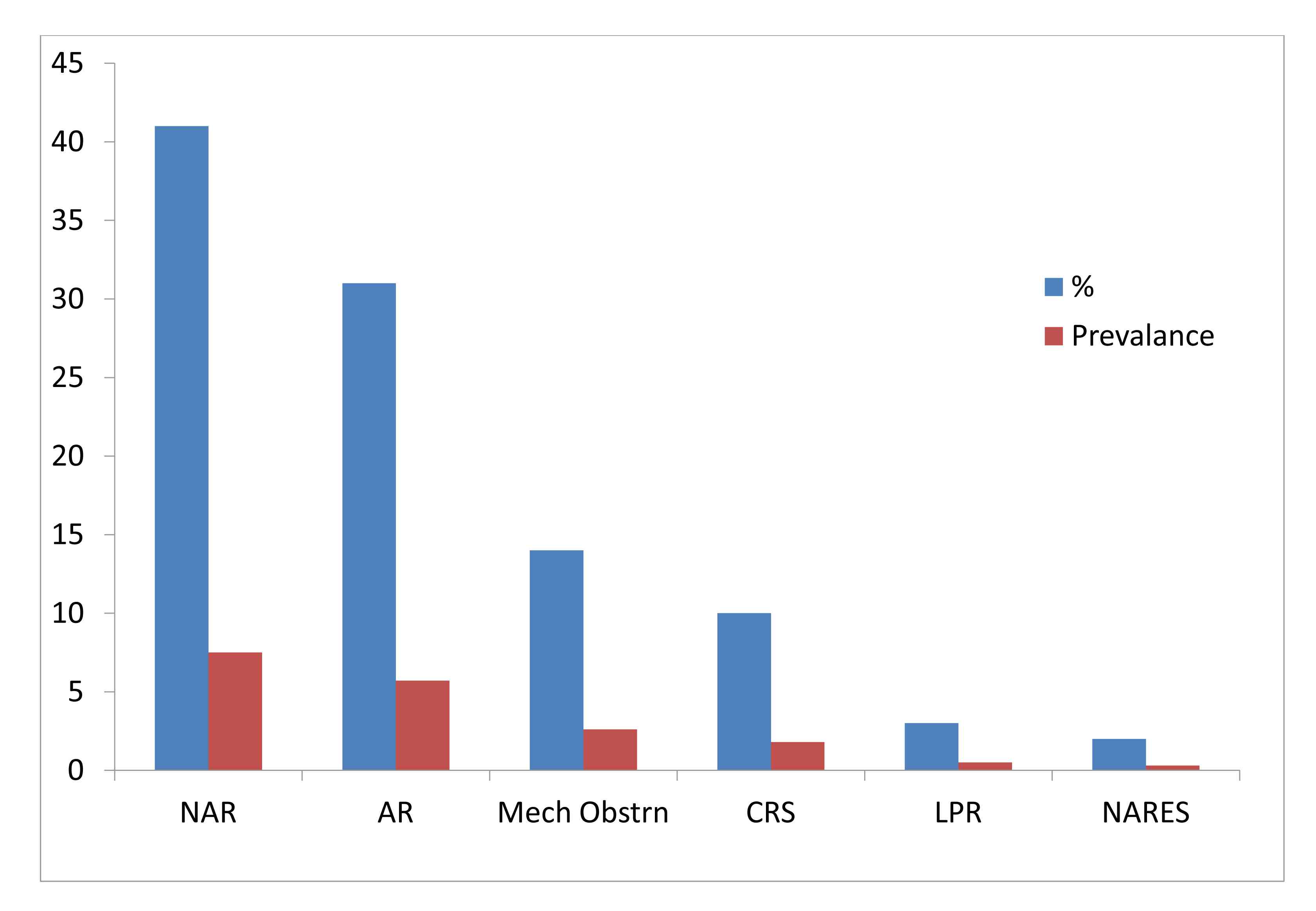
Figure 2: Demonstrates the prevalence’s of NAR.
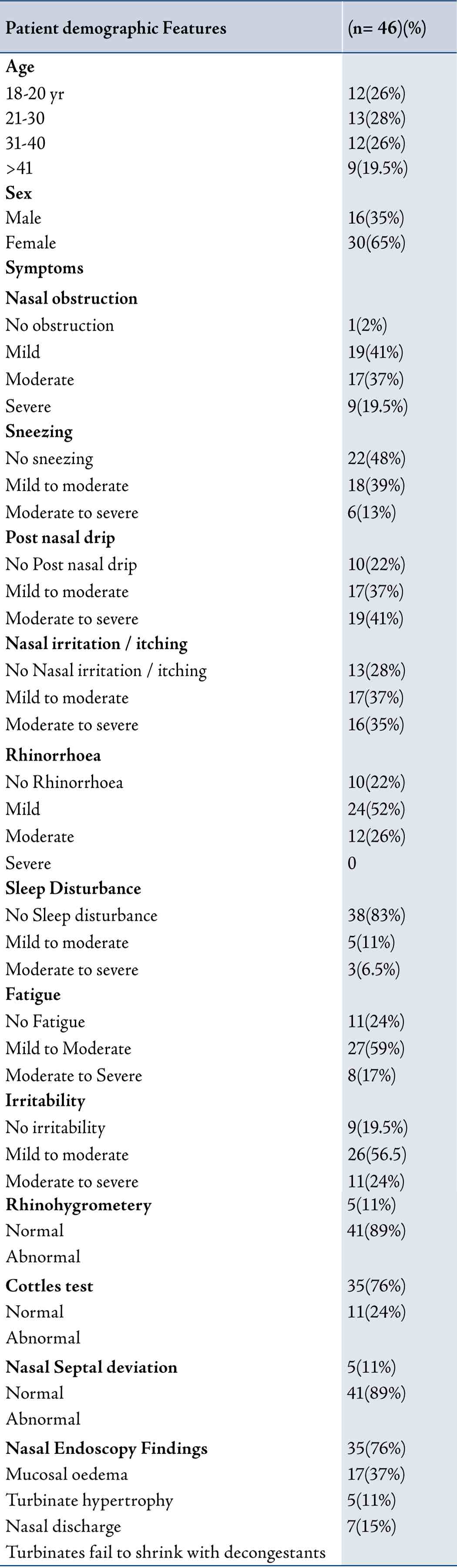
The reported age of onset was 18-20 years in seven patients, while 27 patients reported aggravation of symptoms in the hot summer months and nasal obstruction was the most common symptom, followed by postnasal drip. The details of the clinical profile of patients diagnosed with Non Allergic Rhinitis are presented in Table 1.
Table 1: illustrates clinical profile and nasal examination findings of NAR.
The knowledge gap study which consisted of the assessment and review of 115 Medline titles including 4 systematic reviews, and 34 research papers, as well as 2 recent otolaryngology text books revealed that no study on the prevalence of NAR from Oman. Although the recent text now clearly defines NAR, there is scant literature on the prevalence, diagnosis and management outcomes of NAR in the literature.
Discussion
The diagnosis of rhinitis is generally made on the basis of two or more nasal symptoms, which include nasal congestion, rhinorrhea, sneezing/ itching and impairment of smell for more than one hour on most days for over one year. There are no specific tests for NAR; a thorough case history is the best diagnostic tool to subdivide the condition into subgroups after differential diagnoses have been excluded.2 The classification of subtypes is present in recent texts.1-3
The prevalence of pure chronic NAR represents 17-52% amongst the rhinitis population.4-6 Of the patients that present to the otolaryngologists office, 50% are diagnosed with a form of NAR, and the rest are diagnosed with allergic rhinitis.1 Prevalence of NAR in Oman was found to be 57% of the rhinitis population, these figures are very similar to the ones mentioned in literature.
The knowledge gaps in pathogenesis include; no single unifying theory of the pathogenesis for chronic NAR, and it may represent a group of incompletely-defined disorders.1-3,7
NAR, AR and infectious rhinitis have nasal hyper-reactivity to various stimuli. Unlike patients with AR for whom the etiology is well defined, the etiology and pathophysiology for the majority of patients with NAR are largely unknown. Although the term ‘vasomotor’ implies increased neuronal efferent traffic to the blood vessels supplying the nasal mucosa, this has never been proven.2
In all forms of chronic NAR, there is a variable component of autonomic deregulation including adrenergic, cholinergic and or non-adrenergic, non-cholinergic innervations of the nose.8-11 Patients with NAR may display abnormal neurological findings; abnormal response to various neurogenic stimulation, heightened response to histamine, and cold stimulation of the nasal mucosa,12 as well as diminished response to vasoconstrictive stimuli.13
Twenty seven patients reported exacerbation in hot summer months. The patho-physiology and mechanism of this temperature induced environmental rhinitis can be explained as thus; in Oman the atmospheric temperature varies from 35-48 degree centigrade in the summer months (May - August). When the nasal mucosa is exposed to high temperatures, there is a possibility of the mucosa drying up with a subsequent drying up of the cilia, this can lead to impairment of mucosal clearance and subsequent drying of the mucus, crusts formation which can lead to nasal irritation, trauma to the epithelial cells and neuron trauma while cleaning the nose.2
The nasal mucosa is subjected to frequent changes in temperature and humidity as the subject's environments keeps changing while they travel in cars and keep moving from indoors to outdoors. In the present study, the prominent symptoms found were nasal obstruction and the prominent sign was mucosal edema with inferior turbinate hypertrophy.
The nose has evolved in different racial groups to suit local environments.12,13 The Arab nose is a large nose that could be evolved to increase the function of thermoregulation as the countries have a harsh hot climate. The pathological mechanisms of irritants such as temperature changes causing rhinitis are unclear. It has been postulated that these conditions result from an autonomic nervous system imbalance, including the adrenergic, cholinergic and or non-adrenergic, as well as non-cholinergic innervations of the nose. The symptoms caused by these factors can be explained on the basis of; non-IgE activated vasoactive mediators and changes in the composition of ground substances with interstitial edema. The ground substances changes may be a direct result of the insulting agent or may be mediated via histamines or kinins.14,15
Persistent irritation of the nasal mucosa may cause rhinitis. The most common irritants are dust fumes and chemicals, but pollution may play a role.14 The enhanced susceptibility of the nasal mucosa leads to symptoms of rhinitis such as sneezing, watery rhinorrhea and nasal obstruction. As for the physiologic stimuli to the nose, temperature and moisture change, exercise, types of respiratory ventilation or body posture are well known.
Management outcomes for non allergic rhinitis are lacking from literature. A combination of local intranasal glucocorticosteroids and topical antihistamine azelastine has been recommended. Oral decongestants like pseudoephedrine 30-60 mg on symptomatic days can be given. However, there are no specific studies examining the clinical efficacy.4
Exercise is an important and frequently overlooked adjunct to therapy in patients with non-allergic rhinitis; vigorous exercise decreases nasal congestion by stimulating adrenergic receptors in the nasal mucosa.1 Saline nasal douches have been proved to improve the nasal functions.15 Surgery has been recommended in recalcitrant cases to reduce the specific symptoms.1,2 Several surgical approaches have been used in patients with severe chronic NAR.16-19 These have been reported as uncontrolled case series. While it should be acknowledged that the strength of this study is its prospective collection of clinical data, it is also essential to highlight some of its most obvious limitations. Firstly, the number of patients was low and this should be expected for a condition diagnosed by exclusion, especially since the inclusion criteria were quite rigid; moreover, 35 patients with mixed etiology were excluded. Secondly, this condition belongs to a group of idiopathic rhinitis with not much evidence in literature, possible reason for this could be; difficult to prove, they are therefore underreported and under recognized. Failure to recognize NAR due to unawareness can lead to unnecessary medications and possibly unnecessary surgery exposing patient to adverse sequelae.
Conclusion
This study demonstrated that the overall prevalence of NAR in Oman is 7% in Otolaryngology clinic and 57% of rhinitis patients may suffer from it. There are no specific diagnostic tests for NAR; a thorough case history is the best diagnostic tool to date. Many knowledge gaps exist in the literature with relations to pathogenesis, clinical and laboratory diagnosis and there is a large knowledge gap with reference to medical as well as surgical outcomes. Finally prognosis of NAR, surgical and medical management outcomes need to be further studied in larger study groups.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work. |