Pressure ulcers are a multifactorial, prevalent, and preventable morbidity. Trauma victims are often at risk of developing pressure ulcers more so than patients of neurotrauma. At our level one trauma center, we receive patients with major injuries who are often rendered immobile and bedridden for months. Pressure ulcers often afflict these patients thus prolonging their morbidity and hospital stay.
Pressure ulcers cause a huge burden, financially and emotionally, to the patient, caregivers, and society as a whole. The health care provider is forced to see his good work undone by a pressure ulcer. Trauma is perceived as an acute condition and, ironically, a pressure ulcer is one of the factors associated with chronicity in neurotrauma patients. In our setup, we face challenges exemplified by the poor socioeconomic status of patients along with the ignorance of the caregivers who are usually relatives.
We believe that pressure ulcers are preventable and even if they do occur, we try to suppress their progression to higher grades. Pressure ulcers are classified into four stages according to the depth of tissue involvement as per the National Pressure Ulcer Advisory Panel (NPUAP).1 The staging is a significant tool since the management of a pressure ulcer depends on its stage. A lower stage pressure ulcer is more likely to heal without surgical intervention. In any case pressure sores have poor healing rates and only 75% of stage two ulcers heal in two months. Of stage four ulcers, 62% heal and only 52% in a year.2
The problem is even if we can treat the patient while in the hospital; he may again develop the ulcer once he is discharged. The solution, therefore, lies in preventing or at least detecting ulcers at an early stage so that healing can be quick.
Methods
With this background in mind, we started a Wound Care Surveillance Program in 2012 for patients admitted to the neurosurgery ward. It involved nurses, physiotherapists, and doctors, thus ensuring a multidisciplinary approach so that the patients benefit from all quarters.
The study was a prospective observational study and was carried out in the level one trauma center of our hospital. All patients (n=2,974) admitted in the neurosurgery ward during the study period were included and were observed for development of pressure ulcer. Braden scoring of each admitted patient was performed at first contact3,4 and patients were classified into one of five groups (very high risk to no risk) depending on their score [Box 1].
Box 1: Braden score classification groups.
As a part of the program, serial photography of pressure ulcer was carried out. Presence of granulation tissue or slough was noted to look for worsening of the ulcer. Serial measurement of the pressure ulcer was carried out so that progress could be monitored. The largest two dimensions were measured at detection, weekly after admission, and during out-patient follow-up visits. This was documented in Computerized Patient Record System (CPRS).5 This software is used routinely in our hospital to maintain the database of all our patients. Patients were provided health education regarding home management of the ulcer. A cadre of wound care nurses ensured the compliance of both health care providers and patients with the above interventions. However, their duties were not limited to pressure ulcers but also to other wounds that were being treated at our center.
Since our aim was to detect these ulcers at an earlier stage and to ensure early healing, we looked at the stage at which the pressure ulcer was detected and healing at one, two, and 12 months.
The follow-up schedule was not every three months as most of our patients hailed from distant provinces of the country, and this it difficult for them to follow up made frequently. Our aim was to ensure that they learned the basics of self-care of their pressure ulcers in the first two months.
Variables included severity of head and spinal injury, which was assessed using Glasgow Coma Scale (GCS), and the presence of quadriplegia or paraplegia, respectively. We analyzed these outcome variables and looked for any significant association with any other variables including age, sex, body mass index (BMI), duration of intensive care unit (ICU) and hospital stay, absence of caregivers, site of pressure ulcer, whether the ulcer developed in a hospital or in the community, and the presence of tracheostomy, pelvic fractures, or any other major organ injury.
All 2,974 patients admitted to our neurosurgery ward during the study period were included in the study and were observed for development of pressure ulcers. Those who developed the pressure ulcer were evaluated further for the variables mentioned. For continuous variables, Analysis of Variance (ANOVA) and Kruskal-Wallis equality of populations rank tests were the statistical tests used. For non-continuous variables, Pearson’s chi-square test and Fisher’s exact test were used. A p-value less than 0.050 was considered significant. Statistical analysis was carried out using SPSS Statistics (SPSS Inc., Chicago, US) version 22.0 and Stata (StataCorp LP, Texas, US) version 13.
The ethical guidelines laid out by the ethics committee at our institute were strictly adhered to.
Results
Among the 2,974 patients admitted to the neurosurgery ward of the trauma center in 2012, 92 developed a pressure sore, and we calculated a prevalence of 3.1%. Younger and middle-aged patients were the most commonly affected; 27% of these patients did not survive but in none of them was mortality attributed to the pressure ulcer directly. BMI was available for 62 patients and showed a normal distribution [Figure 1]. The most common modes of injury were road traffic accidents, which accounted for 50% of cases, followed by fall from a height, which accounted for 43% of cases. Most of our patients had just a single pressure area affected, most commonly the sacrum [Figure 2 and Table 1]. The majority were managed with debridement and dressings while 12% received surgical treatment. Special dressings used for grade I and II pressure ulcers include hydrocolloid dressings, collagen dressings, and negative pressure dressings. Five patients were treated with a split-thickness skin graft. Four patients had a flap cover given.
Table 2 gives the factors affecting late detection of pressure ulcers. A patient whose ulcer was detected at a higher stage was likely to have more pressure ulcers (p= 0.005). At one month, only two of the 92 pressure ulcers had healed completely.
Table 1: Distribution of the pressure ulcer based upon their anatomic location.
|
Sacrum |
66 |
|
Greater trochanters |
27 |
|
Occiput |
11 |
|
Heel |
11 |
|
Gluteal region |
7 |
|
Ankle |
3 |
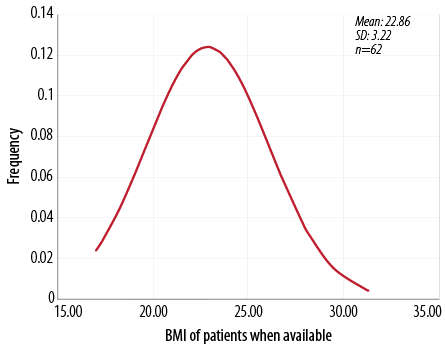
Figure 1: Frequency distribution of body mass index among patients with pressure ulcers. The curve is not skewed suggesting that obesity is not a major factor in the development of pressure ulcers.
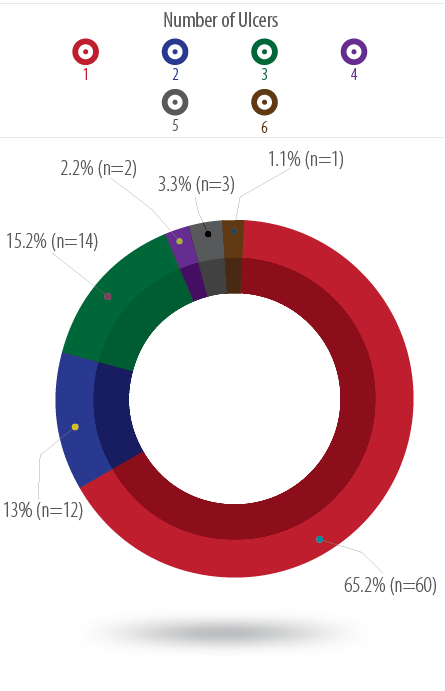
Figure 2: Distribution of the number of pressure ulcers developed. Most patients developed only one pressure ulcer but some developed up to six.
At two months, only 52 patients were followed-up. The remaining patients had either expired or were discharged and did not report for follow-up. Of the patients with stage one ulcers, 29% had healed completely at two months. This number was 17% in stage two and 6% in stage three patients. No patients with stage four ulcers had healed at two months. The Braden score continued to be associated significantly with healing at two months and after discharge at 12 months (p=0.036 and p=0.019, respectively). At discharge, 28% of all patients had healed and the same number improved or healed after discharge, but 44% worsened after discharge and needed dressing and debridement in follow-up. The other factors, associated with healing of pressure ulcers at one month are given in Table 3.
Table 2: Analysis of association of variables affecting the stage of ulcer.
|
Age |
0.881 |
|
Sex |
0.880 |
|
BMI |
0.504 |
|
Braden scores |
0.170 |
|
Duration of ICU stay |
0.088 |
|
Total hospital stay |
0.500 |
|
Unattended patients |
0.711 |
|
Components of Baden Score |
0.170 |
|
Moisture |
0.016 |
|
Activity |
1.000 |
|
Mobility |
0.366 |
|
Nutrition |
0.220 |
|
Friction and shear |
0.091 |
|
Mode of injury |
0.615 |
BMI: body mass index; ICU: intensive care unit.
Patients who had higher moisture score and those with community-acquired ulcers had higher stage of ulcer at presentation.
Table 3: Significance of association between factors with healing or improvement at one month.
|
Age |
0.731 |
|
BMI |
0.375 |
|
Total ICU stay |
0.849 |
|
Total hospital stay |
0.573 |
|
Braden score |
0.001 |
|
Low stage at detection |
0.008 |
|
Severity of head injury |
0.08 |
|
Severity of spinal injury |
0.038 |
|
Associated pelvic and extremity fractures |
0.117 |
|
Associated major solid organ injury |
0.019 |
BMI: body mass index; ICU: intensive care unit.
Discussion
Pressure ulcers, also known as pressure sores, decubitus ulcers, and bedsores, are areas of localized damage to the skin and underlying tissue. They are believed to be caused by a combination of constant pressure, shear, and friction. Pressure ulcers can cause difficulty for caregivers if not prevented, especially in the neurotrauma setting. Numerous studies have evaluated their prevalence, but very few in the Indian context. We calculated a prevalence rate of 3.1%, which is among the lowest reported prevalence rate in the literature. We credit this low prevalence rate to our systematic, multidisciplinary wound care program. Varying prevalence rates have been reported in the literature. A cross-sectional study in India by Agrawal et al,6 put it at 5%, but reports suggest they may prevail at a much higher rate. Rates of 40% and even 85% among neurotrauma patients have been reported.6,7 The International Pressure Ulcer Prevalence (IPUP) Survey established a prevalence of 8–10%.8,9
Patients without help at home did not fare worse compared to those who had family to look after them, whether it was in regard to grade at which the ulcer was detected or healing at one, two, and 12 months or even healing after discharge. This interesting finding was contrary to common perceptions regarding care of unattended patients. This affirms that with a dedicated program like ours, such factors can be negated and it is possible to achieve a low prevalence rate even in such patients. Most of our patients were young and middle-aged males. This indicates the loss of disability-adjusted life year (DALY) in the most productive age group. However, the IPUP Survey reported an increasing prevalence with age8,9 as did a study by Allman et al.10 In our study, age did not have a significant association with any of the outcome variables. BMI showed a normal distribution and did not show any statistically significant association with any of the outcome variables. Most studies document stage one pressure sores as being most prevalent,8,9 but we found stage two to be most prevalent. This could be explained by the skin color of our population, which makes it difficult to detect stage one bedsores. Most of our patients had pressure ulcers at dependent regions (e.g., sacrum) but they can develop at unusual sites too.11
Studies have evaluated the cost of treatment of pressure ulcers. The annual direct cost of treating facility-acquired pressure ulcers ranges from $400,000 to $700,000 per year for hospitals according to the IPUP Survey 2010.9 Another study by Brem et al,12 put the cost of treating stage IV ulcers at over $129,000. A unique characteristic of the health care system in India is that patients in public hospitals make only nominal payments, and the cost of health care is borne by the government. Due to this, we find it impractical to calculate the increased cost due to pressure ulcers. It is our endeavor to reduce the occurrence of pressure ulcers and reduced cost of health care is just one of the benefits of this.
The IPUP Survey 2010 showed an increase in ulcer prevalence with age.8 Various studies have been carried out to review factors associated with the development of pressure ulcers. Factors shown to have a positive association with the development of pressure ulcers are being aged 75 years or more, dry skin, nonblanchable erythema (a stage I pressure ulcer), pressure ulcer history, immobility, fecal incontinence, depleted triceps skinfold, lymphopenia (lymphocyte count <1.50 × 109/L), decreased body weight (<58 kg),10 a low American Society of Anesthesiologists or New York Heart Association score, and low food intake.12,13
The risk a patient is in of developing a pressure ulcer can be predicted using the Braden score, and this helps reduce their prevalence.14 Developed in 1987, it assesses the risk of developing pressure ulcers using six criteria, which are sensory perception, moisture, activity, mobility, nutrition, and friction and shear.3,15 In our study, Braden scoring did not show any significant association with the stage at which the ulcer was detected. The score was associated significantly with all the other outcome variables; healing at one, two, and 12 months and healing after discharge. This suggests that Braden score may be used as a prognostic tool in addition to screening. Among the components of Braden score, moisture was significantly associated with stage at which the ulcer was detected, suggesting that it may be the most important component; however, further studies are required to prove this point. As per our knowledge no study mentioned that Braden system could be used as a scoring and prognostic tool. Moreover, no studies have evaluated each component separately. Other scoring tools exist, such as the water low scale, but we preferred the Braden scale for ease of use and better general acceptance.16 Once a patient is identified to be at risk, preventive measures can be put in place. Various groups such as the Royal College of Nursing and NPUAP have established prevention guidelines.17,18
Our findings highlight the need to improve the home care of pressure ulcers. Community-acquired ulcers are more common in our set-up, and those who acquired ulcers outside the hospital had a much higher stage at detection thereby minimizing the chances of healing if any. In most international studies, including IPUP,8,9 facility-acquired ulcers were more common. Additionally, 44% of our patient’s ulcers worsened after discharge.
Healing was adversely affected by the severity of the spinal injury, associated organ injuries, and the presence of a tracheostomy. None of the studies we found had analyzed the association of healing with the latter two. One would expect that the duration of hospital or ICU stay and increasing age would prevent healing in pressure ulcers, but this was not evident in our study. This may be attributed to our Wound Care Surveillance Program, in which we have been able to negate some of the patient related factors such as duration of hospital and ICU stay and age of the patient.
Conclusions
The Wound Care Surveillance Program has been an effective strategy in the management of pressure ulcers. Braden scoring can be used as a prognostic tool to predict healing of pressure ulcers. Poor healing can be expected in high-grade ulcers and patients with spinal injury (paraplegia or quadriplegia), high-grade solid organ injury, and those who need a tracheostomy. Home based care of pressure ulcers is not up to mark in our set-up and needs to be taken up in the coming phases of our program.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- National Pressure Ulcer Advisory Panel. Available at http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-ulcer-stagescategories/. Accessed September 20, 2015.
- Thomas DR, Diebold MR, Eggemeyer LM. A controlled, randomized, comparative study of a radiant heat bandage on the healing of stage 3-4 pressure ulcers: a pilot study. J Am Med Dir Assoc 2005 Jan-Feb;6(1):46-49.
- Cassell, Charisse. Pressure Ulcer Risk Assessment: The Braden Scale for Prediction Pressure Sore Risk. Health Services Advisory Group of California Inc. Available at http://www.hsag.com/App_Resources/Documents/CA_HSAG_LS3_Risk_Cassell.pdf. Accessed November 18, 2013.
- Braden scale information available at http://www.bradenscale.com/. Accessed September 20, 2015.
- CPRS software. Available at http://en.wikipedia.org/wiki/VistA and http://www.ehealth.va.gov/EHEALTH/CPRS_Demo.asp. Accessed November 18, 2013.
- Agrawal K, Chauhan N. Pressure ulcers: Back to the basics. Indian J Plast Surg 2012 May;45(2):244-254.
- Chauhan VS, Goel S, Kumar P, Srivastava S, Shukla VK. The prevalence of pressure ulcers in hospitalised patients in a university hospital in India. J Wound Care 2005 Jan;14(1):36-37.
- International Pressure ulcer prevalence survey, 2010. Available at https://library.hill-rom.com/Pressure-Ulcer-Management/IPUP/2010-International-Pressure-Ulcer-Prevalence-Survey-Canadian-Results//. Accessed November 18, 2013.
- International Pressure ulcer prevalence survey, 2011. Available at https://library.hill-rom.com/Pressure-Ulcer-Management/IPUP/Overall-Results-from-the-2011-International-Pressure-Ulcer-PrevalenceTM-Survey/. Accessed November 18, 2013.
- Allman RM, Goode PS, Patrick MM, Burst N, Bartolucci AA. Pressure ulcer risk factors among hospitalized patients with activity limitation. JAMA 1995 Mar;273(11):865-870.
- Kataria K, Sagar S, Singhal M, Yadav R. Pressure sore at an unusual site-the bilateral popliteal fossa: a case report. Oman Med J 2012 May;27(3).
- Brem H, Maggi J, Nierman D, Rolnitzky L, Bell D, Rennert R, et al. High cost of stage IV pressure ulcers. Am J Surg 2010 Oct;200(4):473-477.
- Lindgren M, Unosson M, Krantz AM, Ek AC. Pressure ulcer risk factors in patients undergoing surgery. J Adv Nurs 2005 Jun;50(6):605-612.
- Comfort EH. Reducing pressure ulcer incidence through Braden Scale risk assessment and support surface use. Adv Skin Wound Care 2008 Jul;21(7):330-334.
- Berma A, Kozier B. Kozier & Erb’s fundamentals of nursing: concepts, process, and practice. 8th ed. Upper Saddle Riveer, NJ: Pearson Education, 2008. p. 905-907.
- Waterlow Score - Tool Evaluation. Melbourne Health. Available at http://www.health.vic.gov.au/__data/assets/file/0009/233667/Waterlow-scale.pdf. Accessed September 20, 2015.
- Royal College of Nursing. Clinical practice guidelines. Pressure ulcer risk assessment and prevention recommendations 2001. Available at http://www.rcn.org.uk/__data/assets/pdf_file/0003/78501/001252.pdf. Accessed November 18, 2013.
- NPUAP guidelines. Available at http://www.npuap.org. Accessed November 18, 2013.