| |
Abstract
A polytrauma patient on ventilator was admitted to ICU with open tracheostomy, GCS 8/15 and unequal pupils. After 10 days, he was weaned from the ventilator. The patient had respiratory problems i.e. expiratory stridor, shortness of breath, dysphonia and dyspnea on closing tracheostomy. It was diagnosed as a case of asthma, and the patient responded to salbutamol nebulization and intravenous steroid therapy. However, after some time, he desaturated and a plan for rapid sequence intubation was made. Endotracheal tube could not be negotiated beyond vocal cords, so an unprepared tracheostomy without proper equipment had to be immediately done by an anesthetist to save the patient’s life. CT scan revealed tracheal stenosis. This case demonstrates that patients with a short 15-days history of previous tracheostomy may have tracheal stenosis.
Keywords: Tracheostomy complication, stenosis, ICU.
|
|
| |
Introduction
Most patients who require prolonged ventilator support in ICU have to undergo tracheostomy.1 These patients can have multiple complications after the closure of tracheostomy. Iatrogenic airway injury after tracheostomy continues to be a serious complication.1 We hereby present a case of early tracheostomy done on day number one in a polytrauma patient who developed a life threatening complication after closure of tracheostomy on the tenth day. The correct diagnosis of tracheal stenosis was missed because of atypical presentation of wheezing and stridor.
Case Report
A 23 year old male patient was transferred to Khoula Hospital with polytrauma from a road traffic accident. The patient had severe head injury, multiple lower leg and facial bone fractures. There was no associated medical problem. An open tracheostomy (tube size 8.0) was done by a general surgeon at the referral hospital for facial injuries and on the same day, the patient was shifted to Khoula Hospital on a ventilator. At the time of admission, the patient had GCS of 8/15, the pupils were unequal, the right pupil was dilated (5mm) and was not reacting to light, and the left pupil was 2 mm and had only a sluggish reaction to light. He stayed in ICU for 10 days and was later shifted to the ward with tracheostomy. At that time, he was breathing on room air and his GCS was 10T.
In the ward, the tracheostomy was closed uneventfully. Later, he started having problems with respiration. To begin with, it was slight effort on inspiration which gradually increased to shortness of breath, dysphonia and dyspnea. Auscultatory findings were; bilateral scattered ronchi, few crepts and expiratory stridor. The patient’s respiratory condition improved after steroid therapy and salbutamol nebulization. Second day after shifting from ICU, the patient again had respiratory problems. He could not lie down on the bed, due to dyspnea and respiratory stridor. Therefore, he was shifted back to ICU for further management. In the ICU, he was kept in a propped up position, meanwhile intravenous steroid and salbutamol nebulization were continued. After 4 hours of ICU stay, the patient had a sudden severe respiratory crisis. The patient’s respiratory rate was 40/min, saturation dropped to 80% and ABG showed a PaO2 of 45 mm of Hg. Immediate decision was taken to intubate the patient and crash trolley was kept ready. The patient was induced with Thiopentone (4 mg/Kg, IV) and relaxed with suxamethonium (2 mg/Kg, IV). Intermittent positive pressure ventilation was tried with AMBU bag but failed. The saturation started dropping further, therefore intubation was attempted immediately. After laryngoscopy, the vocal cords were visualized but the patient could not be intubated. Even the endotracheal tubes of smaller number (No 5.0 uncuffed) could not be negotiated; hence immediate decision to do an open tracheostomy was taken. As it was an emergency situation, the surgeon was called for, but because of lack of time the anesthetist had to start an open tracheostomy. It was a repeat tracheostomy with a lot of fibrosis and anatomy was not clear, but still the passage could be created and the tracheostomy tube was inserted and patient ventilated through it. Saturation started improving. By this time, the surgical team also arrived and the patient was stabilized. CT scan was done later on, which showed the tracheal stenosis of about 12 mm in length (Fig. 1). The CT scan report mentioned, "The patient is having tracheal stenosis of 12mm, which is extending in thoracic part of trachea. It is almost completely occluding the lumen of the trachea." ENT consultation was done and the patient was shifted to cardiothoracic surgery for the sleeve resection of the trachea.
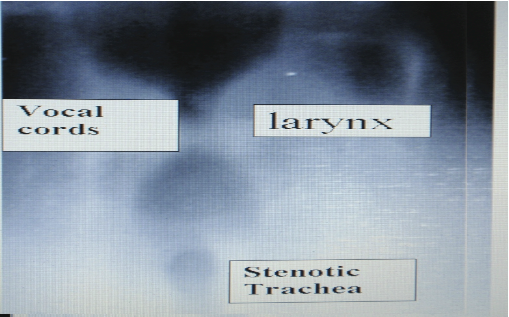
Figure 1: CT scan showing tracheal stenosis
Discussion
Although lower airway obstruction may result from a wide variety of pathologic conditions, most cases are secondary to endotracheal tube or tracheostomy injury. This airway trauma causes pressure necrosis and induces inflammation, characterized by granulation tissue and perichondritis.2 Major causes leading to stenosis at stoma site include; large tracheostomy stoma or large tube inserted in small stoma by force, damage to the first tracheal ring or cricoid cartilage, wound sepsis and abnormal wound healing with excess granulation tissue formation around the tracheal stoma.2 Increased cuff pressure of the tracheostomy tube can also be one of the causes for tracheal stenosis.3 The inflammation, in turn leads to collagen deposition, fibrosis and in severe cases, chondritis and cartilage collapse with loss of tracheal cartilage. Subsequent scar contracture results in luminal narrowing and obstruction.3 Early stages are characterized by granulation tissue, late stages by mature fibrous strictures and tracheomalacia.4, 5
There was no chance of having high cuff pressure in this patient because according to our ICU protocol, all the patients who are having tracheostomy tube or cuffed endotracheal tube are monitored for the cuff pressure by a manometer regularly, which is kept between 20-30cm of H2O. The inflammation in turn, leads to collagen deposition, fibrosis and in severe cases, chondritis and cartilage collapse with loss of tracheal cartilage. Subsequent scar contracture results in luminal narrowing and obstruction.3 Early stages are characterized by granulation tissue, late stages by mature fibrous strictures and tracheomalacia.4,5 In a review of tracheal stenosis in a patient following tracheostomy, Zias et al. reported that tracheal stenosis could develop after 14 to 151 days of the procedure.6 The length of stenosis varies from 0.5 cm to 2.5 cm. 6The reported incidence of tracheal stenosis following tracheostomy ranges from 0.6- 21%. But only 1-2% of patients are symptomatic and have severe stenosis.2 The clinical manifestation of such obstruction may include expiratory stridor, dysphonia, shortness of breath and dyspnea on exertion. Difficulty in bringing up secretions may be an early symptom. These signs and symptoms may mimic other more common cardiopulmonary disorders such as asthma, bronchitis and congestive heart failure and thus delay diagnosis.7 This is exactly what happened in the present case.
We suspected it to be a case of asthma with bronchitis because the patient’s chest was having typical findings of wheeze, bilateral scattered bronchi and expiratory crept and responded to the initial treatment given. Physician’s findings were stridor, sinus tachycardia, no chest pain, diagnosis of obstructive airway disease; which also added to the misdiagnosis. The prescribed treatment was oxygen, salbutamol nebulization, hydrocortisone 100mg stat, and repeat nebulization after 30 min. History of tracheostomy was very short; less than 15 days, therefore, our choice of therapy was guided by specific signs, symptoms and the patient’s condition. An important rule of thumb is the patient who presents the signs and symptoms of airway obstruction must be considered to have an organic lesion until proven otherwise and should not be diagnosed as a case of asthma.8
Conclusion
We should be aware that patients with these kinds of findings may have tracheal stenosis. If a patient has undergone prior tracheostomy, then a surgeon along with the tracheostomy kit should be available before intubation is attempted.
Acknowledgements
The authors reported no conflict of interest and funding has been received on this work.
|
|
| |
- Ahmed R, Rady SR, Mohammad Siddique JI, Iqbal M. Percutaneous tracheostomy in critically ill patients: 24 months experience at a tertiary care hospital in United Arab Emirates. Ann Thorac Med 2010 Jan;5(1):26-29.
- Tsitouridis I, Michaelides M, Dimarelos V, Arvaniti M. Endotracheal and tracheostomy tube-related complications: imaging with three-dimensional spiral computed tomography. Hippokratia 2009 Apr;13(2):97-100.
- Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol 2004 Nov;4(1):8. . http://www.biomedcentral.com/1471-2253/4/8.
- Duncavage JA, Ossoff RH. Laser application in the tracheobronchial tree. Otolaryngol Clin North Am 1990 Feb;23(1):67-75.
- Har-El G, Shaha A, Chaudry R, Lucente FE. Resection of tracheal stenosis with end-to-end anastomosis. Ann Otol Rhinol Laryngol 1993 Sep;102(9):670-674.
- Zias N, Chroneou A, Tabba MK, Gonzalez AV, Gray AW, Lamb CR, et al. Post tracheostomy and post intubation tracheal stenosis: report of 31 cases and review of the literature. BMC Pulm Med 2008;8:18. . http://www.biomedcentral.com/1471-2466/8/18.
- Cooper JD. Complication of tracheostomy: pathogenesis, treatment, and prevention. In International Trends in General Thoracic Surgery: Major Challenges, eds Grillo HC, Eschapasse H. vol 2: Philadelphia, WB Saunders, 1987; p 21-53.
- Grillo HC. Reconstructive techniques for extensive post-intubation tracheal stenosis. Int Surg 1982 Jul-Sep;67(3):215-220.
|
|