A 35-year-old male presented with complaints of a progressive increase in the size of his right thumb. There was a significant increase in subcutaneous tissue, which was most prominent on the palmar aspect. He was experiencing difficulty in his day-to-day work due to restricted movement. There was no history of trauma, infection, or a family history suggestive of neurofibromatosis or any similar disease. He had undergone surgery two years prior for similar complaints in the index finger. Plain radiograph of the hand [Figure 1] was advised following this magnetic resonance imaging (MRI) of the right hand was preformed to confirm the diagnosis and assess the disease status [Figure 2].
A plain X-ray of the hand of another patient with similar complaints in the middle finger showed increased lengths of metacarpals and phalanges of the middle finger with prominent soft tissue and is shown in Figure 3.
Questions
- What is the diagnosis?
- Name the commonly associated nerve pathology with this condition?
Answers
- Macrodystrophia Lipomatosa
- Fibrolipomatous hamartoma of the median nerve.
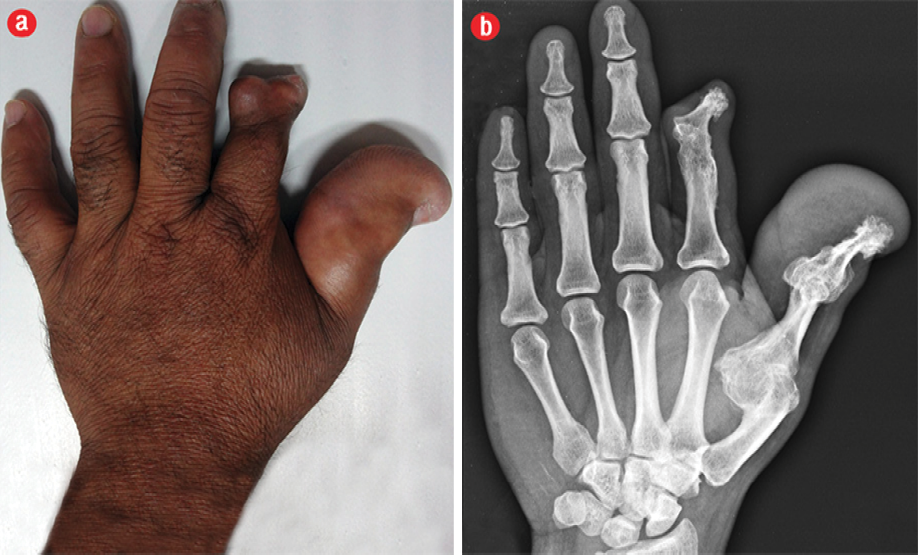
Figure 1: (a) Clinical photograph showing localised enlargement of thumb with postoperative changes in index finger. (b) X-ray imaging of the hand shows hypertrophy of soft tissue and bone with mushroom shaped terminal phalanx. Secondary degenerative changes are seen early in the involved digit.
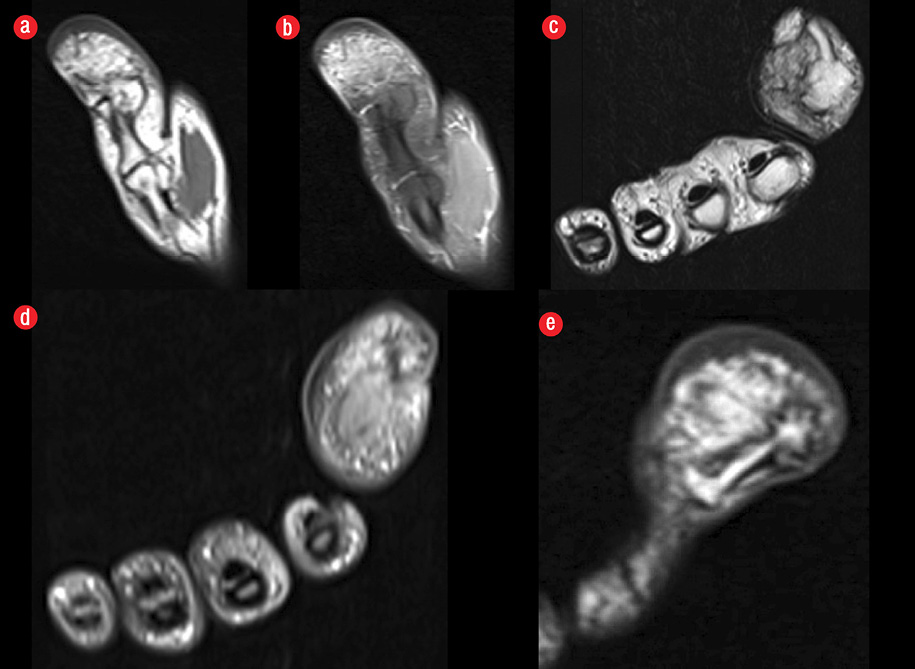
Figure 2: Magnetic resonance imaging of the fingers. (a) T1-weighted imaging shows proliferation of the fibro-fatty tissue of the thumb. (b) PD fat saturated confirms the fatty nature. (a-d)The associated bony changes are seen. (e) Mushrooming of the terminal phalanx is also seen.
Discussion

Figure 3: X-ray imaging of the hand of another patient shows hypertrophy of soft tissue and bone of middle finger with advanced degenerative changes in the involved digits.
Macrodystrophia lipomatosa is a rare, congenital, but non-hereditary disease. It is characterized by disproportionate overgrowth of the mesenchymal elements. It can be associated with syndactyly, polydactyly, or clinodactyly. The exact etiology is not understood, but the various hypotheses proposed include abnormality in fetal circulation, alteration of somatic cells in limb bud development, and hypertrophy of the concerned nerve.1
The lesion follows a sclerotome distribution.2 Involvement of the lower limbs is more common than the upper limbs. The second and third digits of the feet and hand are most frequently involved corresponding to the nerve supply of the medial plantar nerve and median nerve, respectively. Most commonly, a single limb with involvement of the distal part of the extremity is seen. Rarely, it can extend to involve the proximal part of an extremity or the abdominal wall.2,3 There is no definite sex predilection, but the macrodystrophia lipomatosa encountered by patients can be categorized under two headings; cosmetic and mechanical.1 Enlargement of body parts itself can lead to interference in normal day-to-day activities as was noted in our patients. However, true mechanical problems arise secondary to osteoarthritis and/or compression of neurovascular structures.
Plain radiograph revealed hypertrophy of bone and soft tissue. The phalanges appeared to be mushroom shaped due to broadening and elongation of the ends.2 Secondary degenerative changes were seen early in the involved digits. These findings were noted in both cases in the current report. Computed tomography can demonstrate excess fat deposition and associated bony changes,4 but MRI is the preferred investigation of choice because it is safe from radiation. More importantly, MRI can characterize fatty tissue and help in excluding other differential diagnosis. On MRI, the fibro-fatty tissue follows signal intensity of fat (hyper intense on T1-weighted imaging, and intermediate on T2-weighted imaging with suppression on fat-saturated sequences), and fibrous septae are seen as low signal intensity strands traversing the fatty tissue. The associated bony changes are well appreciated on proton density sequences. The histopathological examination in macrodystrophia lipomatosa shows abundance of mature adipocytes scattered within the fibrous tissue involving the periosteum, nerve sheaths, and subcutaneous tissues.1 However, in the present cases the clinical evaluation and plain radiograph were classic of macrodystrophia lipomatosa.
Differential diagnosis for these cases include neurofibromatosis type 1 (plexiform neurofibroma), Klippel-Trenaunay-Weber syndrome, lymphangiomatosis, hemangiomatosis, and proteus syndrome.1,2,4 In neurofibromatosis, there is family history along with characteristic skin lesions and subcutaneous nodules, which are helpful towards reaching a diagnosis. In Klippel-Trenaunay-Weber syndrome, besides localized gigantism, associated capillary malformations with varicose veins are also observed. No bony changes are seen in hemangiomatosis and lymphangiomatosis, whereas proteus syndrome presents with associated skull and dermatological changes, lung cysts, and intra-abdominal lipomas.
Fibrolipomatous hamartoma (FLH) most commonly occurs in the median nerve and is characterized by deposition of fat within the nerve sheath separating axonal bundles sheathed in the perineurium.5 However, macrodystrophia lipomatosa is associated with FLH in 30–66% of cases.6 On MRI, FLH presents as a speckled appearance correlating with fat deposition within the nerve. Peripheral nerve sheath tumors can rarely be differential and are confirmed by histopathology.7
Management depends on the age of the patient, symptoms, and severity of the disease. Improving cosmetic appearance is the most frequent reason for operation but preserving the neurological function is equally important. Debulking procedures, osteotomies, and epiphysiodesis are indicated in severe disease.1 Nerve injury and recurrence are the limiting factors of surgery.8
Disclosure
The authors declared no conflict of interest. No funding was received on this work.
references
- Khan RA, Wahab S, Ahmad I, Chana RS. Macrodystrophia lipomatosa: four case reports. Ital J Pediatr 2010;36:69.
- Fritz TR, Swischuk LE. Macrodystrophia lipomatosa extending into the upper abdomen. Pediatr Radiol 2007 Dec;37(12):1275-1277.
- Balakrishna BV, Prasad SRH. Macrodystrophia Lipomatosa. Ind J Radiol Imag 2005 15; 3:349-52.
- Koplay M, Kantarci M, Kilinc G. Medical image. Macrodystrophia lipomatosa: multidetector CT and MRI findings. N Z Med J 2012 Mar;125(1352):104-105.
- Singla V, Virmani V, Tuli P, Singh P, Khandelwal N. Case Report: Macrodystrophia lipomatosa - Illustration of two cases. Indian J Radiol Imaging 2008 Nov;18(4):298-301.
- Cavallaro MC, Taylor JA, Gorman JD, Haghighi P, Resnick D. Imaging findings in a patient with fibrolipomatous hamartoma of the median nerve. AJR Am J Roentgenol 1993 Oct;161(4):837-838.
- Fathaddin A, Fatani R. Palmar Nerve Sheath Myxoma: A Case Report. Oman Med J 2012 May;27(3) .
- Tuzuner T, Parlak AH, Kavak A, Alper M. A neglected case of macrodystrophia lipomatosa of the foot in an elderly man. J Am Podiatr Med Assoc 2005 Sep-Oct;95(5):486-490.