|
Introduction
The term "Metabolic Syndrome" was coined more than four decades back (1977) by Haller1 while reporting associations of obesity, diabetes mellitus, hyperlipoproteinemia, hyperuricemia and steatosis hepatis.2 The same year, Singer used the term for associations of obesity, gout, diabetes mellitus, and hypertension with hyperlipoprotenemia.3 Then another concept was given by Gerald B. Phillips which states that risk factors for myocardial infarction concur to form a "constellation of abnormalities" (i.e., glucose intolerance, hyperinsulinemia, hyperlipidemia (hypercholesterolemia and hypertriglyceridemia) and hypertension) that is associated not only with heart disease, but also with aging, obesity and other clinical states. It was suggested that there must be some underlying linking factor. At that time it was speculated that if the missing link is found, it can affect strategies regarding prevention of cardiovascular disease; Gerald B. Phillips hypothesized that this factor was sex hormones.4,5 In 1988, in his Banting lecture, Reaven proposed insulin resistance as the underlying factor and named the constellation of abnormalities as "Syndrome X." Reaven did not include abdominal obesity, which has also been hypothesized as the underlying factor.6
The prevalence of Metabolic Syndrome (MetS) in Pakistan is alarmingly high, and is reported to range from 18% to 46%.7 But the knowledge about this rampant clinical entity is meager, not only among the general population but also among healthcare providers. Thus we are currently going through a silently damaging epidemic. It is the need of hour that all health professionals should educate the general public about this moster. To meet this end, the health professionals must be well aware about the disease. We have conducted this study to see the awareness and prevalence of Metabolic Syndrome amongst the medical community of Bahawalpur.
Methods
Study Design and Duration: It was a cross-sectional study. It was carried out in a period of about one year (June 2008 to May 2009). The following institutions took part in the study: Bahawal Victoria Hospital, Quaid-e-Azam Medical College, Paramedical and Nursing Schools and Female Jubilee Hospital.
Sample: A total of one hundred and ninety four (194) Doctors and Paramedics (Nurses and Dispensors) out of about 1800 healthcare professionals working in the institutions included in study were selected by simple random sampling technique. The sample size was calculated with the help of Power Analysis and Sample Size (PASS) software using 90% power of study. As most of the staff is above 20 years of age and the age of retirement as per rules is 60 years, so we included the above said age group among both sexes after written consent. The subject suffering from chronic diseases and females having pregnancy were excluded. The students, temporary trainees and those not willing for the study were excluded.
Data Collection and Analysis: The data about the awareness of MetS was collected on a specially designed proforma having a total of 24 questions. Nine questions were about the identification of the responder, name, age, sex, designation, department, height, weight, hip circumference and blood pressure receptively. Next 3 questions were to note fasting levels of glucose, triglycerides and HDL-Cholesterol. Last 12 questions were about the awareness of MetS and multiple answers were given for each question. Responders had to tick one best answer. These proformas were validated by institutional review and ethical committees. The proformas were given to the individual health professionals who returned them after filling the required columns. The anthropometric measurements i.e., height, weight, waist and hip circumference were taken with the help of measuring tape and weight machine available at the department of medicine, Bahawal Victoria Hospital. Fasting venous blood was collected in 5ml sterile syringes (BDTM) for the estimation of followings; serum glucose, serum triglycerides and serum HDL. All samples were sent to Pathology Lab, QAMC Bahawalpur. All tests were done with standard laboratory techniques and negative controls were run to assure quality. After getting the reports of the above mentioned investigations and entering them into the respective columns of the proforma, data was subjected to manual analysis.
Results
Metabolic syndrome was diagnosed according to the NCEP ATP III guidelines which requires any three of the following to meet with; central obesity: waist circumference ≥102 cm or 40 inches (male), ≥88 cm or 36 inches(female), dyslipidemia: TG ≥1.7 mmol/L (150 mg/dl), dyslipidemia: HDL-C <40 mg/dL (male), <50 mg/dL (female), blood pressure ≥130/85 mmHg, fasting plasma glucose ≥6.1 mmol/L (110 mg/dl). Obesity was defined by a BMI ≥30.
The age distribution of the sample population is given in fig. 1 which shows health workers of all ages were included in the sample.
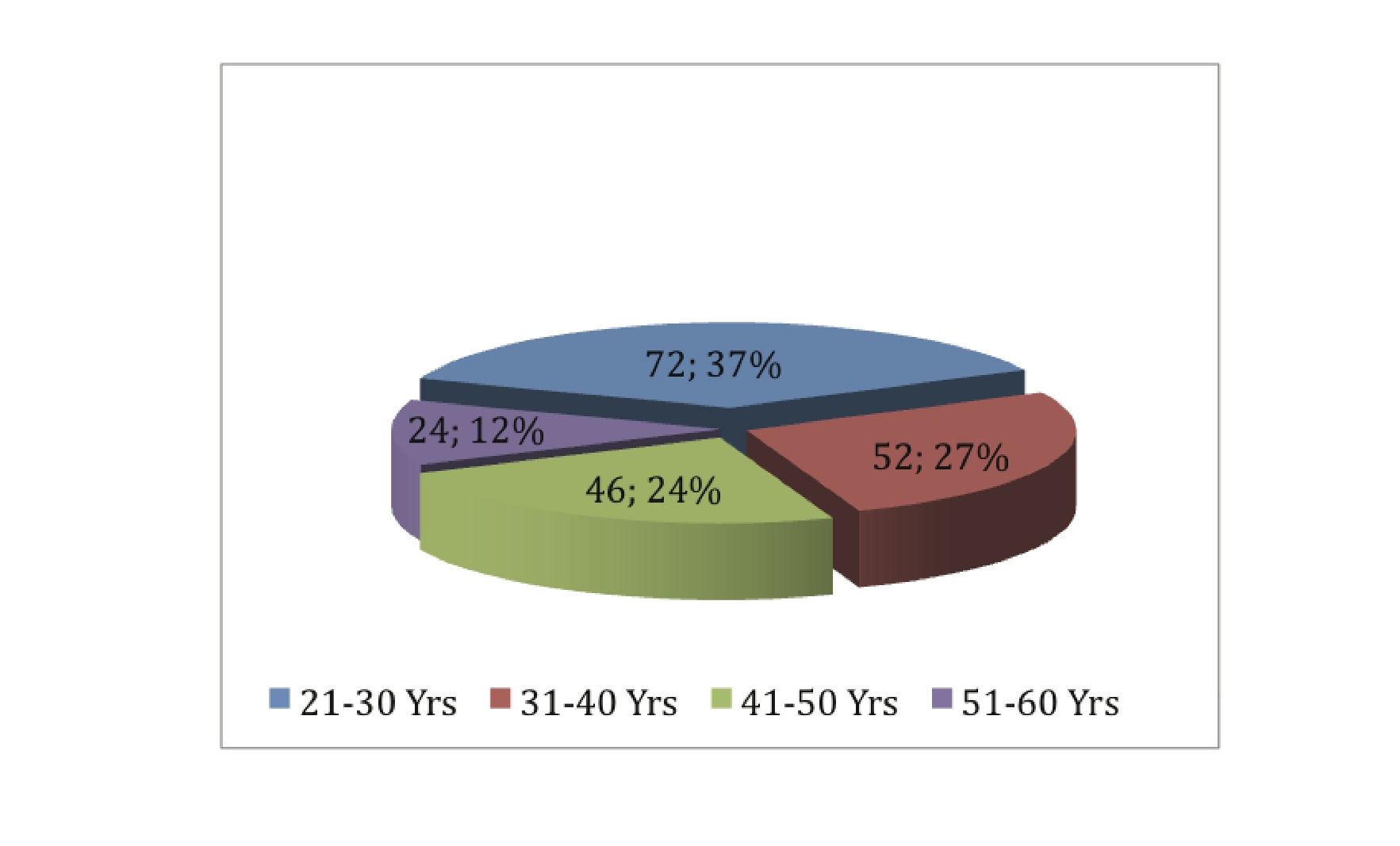
Figure 1: Age Distribution of Study Population
The gender distribution of the sample population is given in fig. 2 which shows a peculiar pattern of gender distribution among local health workers where there is all nurses are females and almost all paramedics are males.
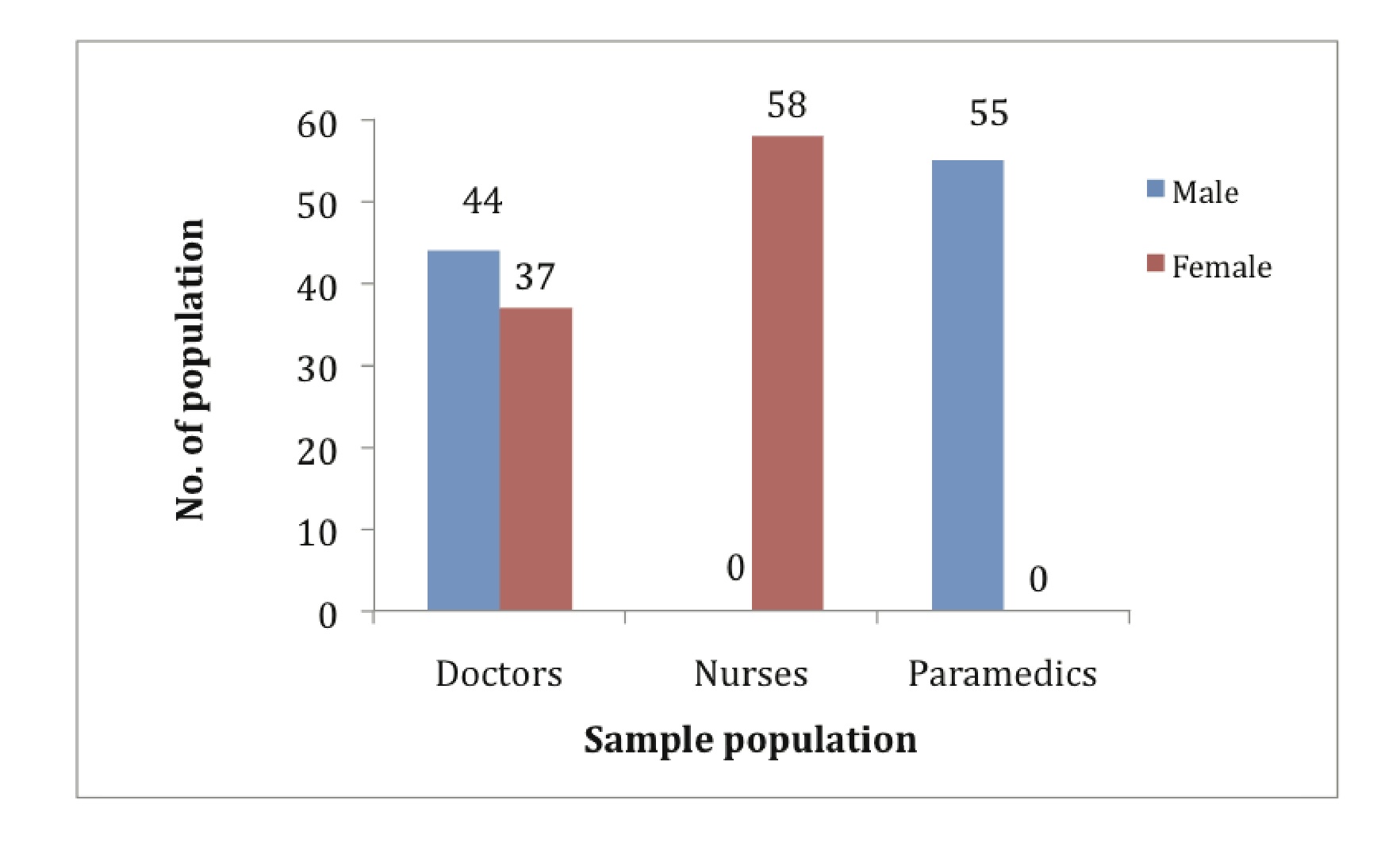
Figure 2: Gender Distribution of Study Population
At least three criteria of MetS were correctly listed by 36 participants (18.56%), with physicians showing significantly higher awareness levels (p<0.001).
Metabolic syndrome was diagnosed in 29 out of 194 participants (14.95%), and there was no significant difference between men and women in this respect (p>0.05) as shown in fig. 3.
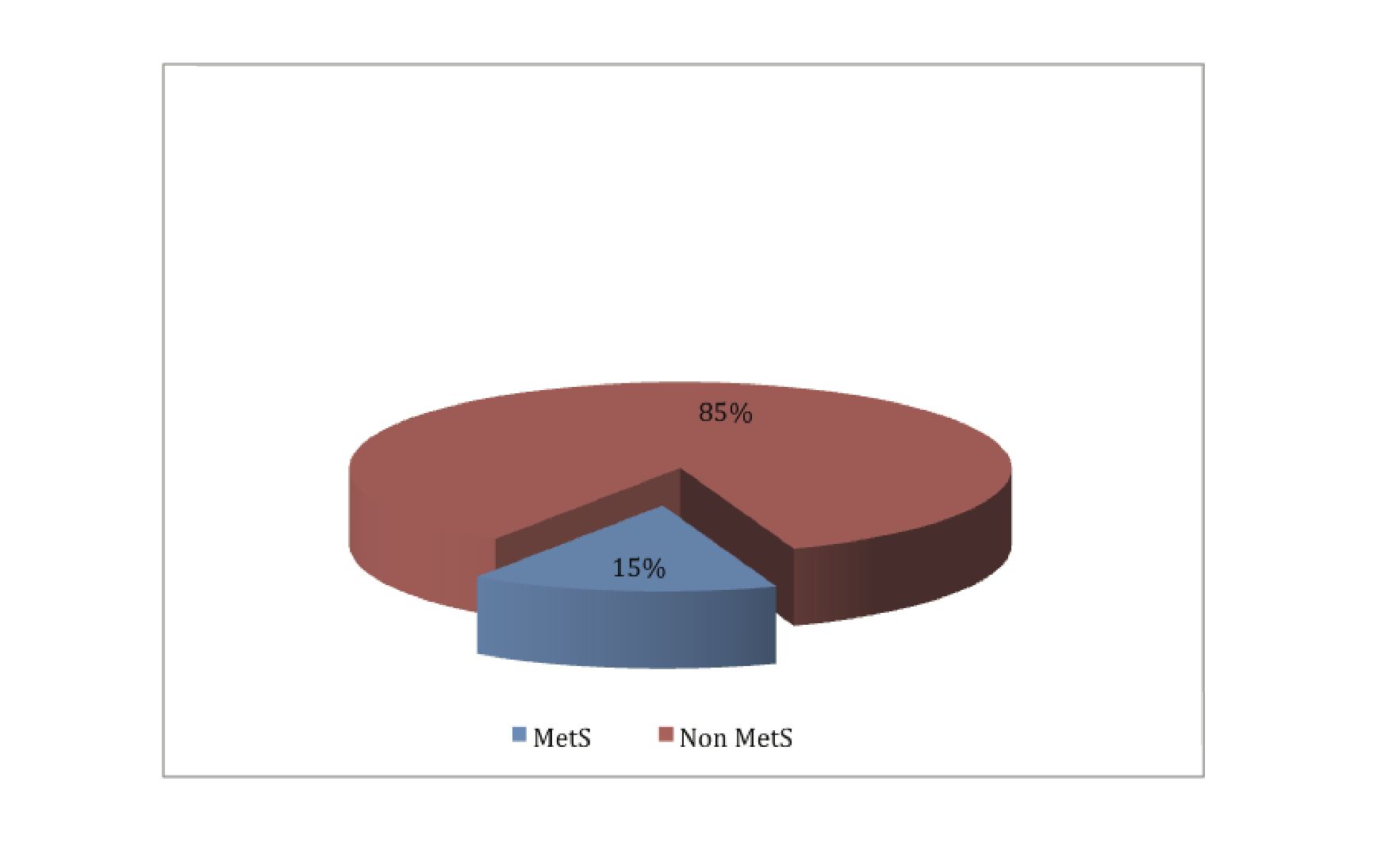
Figure 3: Prevalence of Metabolic Syndrome
The frequency of abdominal obesity was 22.68% and it was significantly higher in males than in females (29.29% vs. 14.74%; p<0.001) as shown in fig. 4.
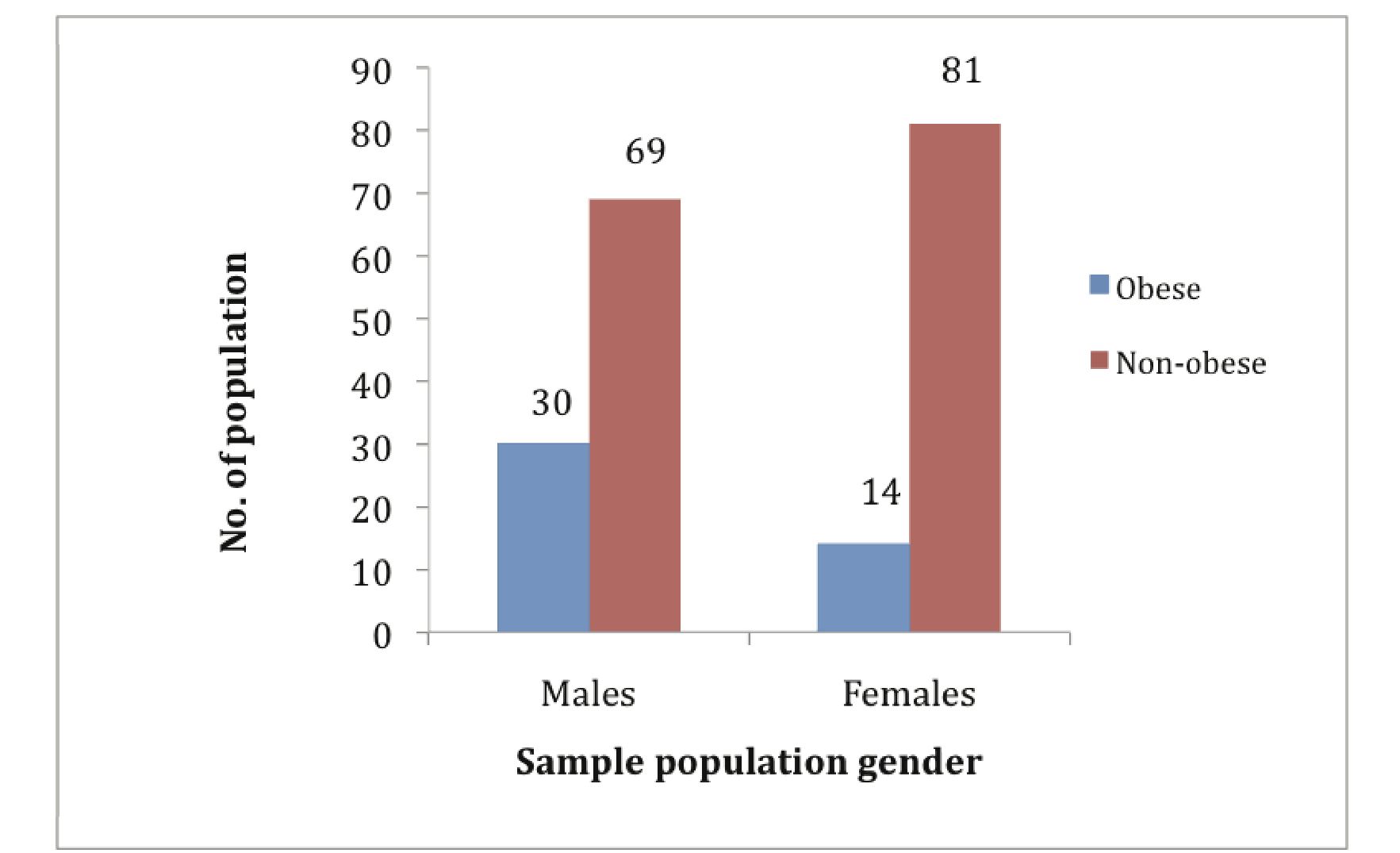
Figure 4: Prevalence of Central Obesity
Discussion
The terms "metabolic syndrome," "insulin resistance syndrome," and "syndrome X" are now used specifically to define a constellation of abnormalities that is associated with increased risk for the development of type 2 diabetes and atherosclerotic vascular disease (e.g. heart disease and stroke). The exact pathophysiology of metabolic syndrome is not yet completely known. Most patients are older, obese, sedentary, and have a degree of insulin resistance. The most important identified factors in order are: weight, aging, genetics, and lifestyle, i.e., low physical activity and excess caloric intake.
There has been an endless debate regarding whether obesity or insulin resistance is the cause of the metabolic syndrome or if they are the consequences. Many attempts have been made but the issue is still partially solved. A number of markers of systemic inflammation, including C-reactive protein, fibrinogen, interleukin 6 (IL–6), Tumor necrosis factor-alpha (TNFα) and others are often increased. Some investigators have pointed to oxidative stress due to a variety of causes including increased uric acid levels caused by dietary fructose.7-9 Commonly there is development of visceral fat after which the adipocytes increase plasma levels of TNFα and alter levels of a number of other substances (e.g., adiponectin, resistin, PAI-1). TNFα has been shown not only to cause the production of various inflammatory cytokines, but possibly to trigger cell signaling by interaction with a TNFα receptor that may actually lead to insulin resistance.10 An experimental attempt with rats that were fed a sucrose-based diet has been proposed as a model for the development of the metabolic syndrome. The sucrose first elevated triglycerides levels in plasma, leading to visceral fat and ultimately ending up in insulin resistance.11 The progression from dietary habits to visceral fat and then through TNFα pathway and resulting into insulin resistance has some parallels to the development of MetS in human.
Today, many definitions of metabolic syndrome exist among key health organizations around the globe. However, the World Health Organization (WHO) the International Diabetes Federation (IDF) and the Adult Treatment Panel III (ATPIII) share core components in their definitions as follows: obesity, dyslipidemia, high blood pressure and insulin resistance or diabetes. WHO criteria also address microalbuminuria as a component of MetS because it is a possible risk factor for atherosclerotic vascular disease, as it indicates endothelial dysfunction and subclinical atherosclerotic damage.12 The definition that has high sensitivity and specificity, most user-friendly and least confusing for clinicians should be used.
We used NCEP ATP III definition for the diagnosis of MetS. We found that only 36 (18.56%) of the participants (mostly physicians) knew ≥3 (of 5) diagnostic criteria for MetS. While almost all of the nurses and paramedics were unaware of MetS. The prevalence of MetS was 14.95% with no significant difference among the two sexes. The prevalence of the central obesity in the current study was 22.68%, with significant male preponderance.
Metabolic syndrome has been studied a lot. But its awareness among healthcare professionals have been widely neglected. We could only find a few studies evaluating awareness and prevalence of MetS in medical communities. In a recent study involving 723 healthcare workers from 4 major hospitals in Turkey,13 the prevalence of MetS was found to be 7.9% with no gender difference. In the same study,13 the central obesity was seen in 13.8% of the healthcare workers with significantly higher prevalence among males. Our findings show that MetS is more common among our healthcare population as compared to Turkish counterpart. On the other hand the awareness about MetS in our healthcare workers (18.56%) is profoundly low if we keep in consideration the awareness level of 33.2% among the participants of aforementioned study.13
Being medical professionals, we must keep ourselves abreast with upcoming medical problems and entities. It is inevitable exercise and is a prerequisite for health education.
Conclusion
Current study shows that only a minority of medical community are aware of MetS as a clinical entity. Nurses and other paramedics are unaware of the problem. The prevalence of metabolic syndrome and central obesity was as high in healthcare workers as in general population.
Acknowledgements
We acknowledge Ms. Sehar Nigar (4th year MBBS) for helping the authors in data collection, taking anthropometric measurements and drawing blood samples. We are also thankful to health workers of Bahawalpur who cooperated despite their busy schedule.
|