|
Abstract
Objective: To report the patterns and causes of neonatal death from a tertiary care neonatal intensive care unit over a period of four years.
Methods: This is a retrospective cohort study where four years data (January 2006 - December 2009) of all inborn neonatal admissions and deaths were collected from the neonatal intensive care unit at Sultan Qaboos University hospital on predesigned forms. All out born admissions and deaths were excluded. The causes of neonatal death were classified using Wigglesworth's classification.
Results: The number of inborn live births during the study period was 10064 and the total number of inborn neonatal admissions was 1475. The total deaths (neonatal and post neonatal) at the neonatal intensive care unit was 73 (63 inborn and 10 out born). Among the inborn, five deaths were post neonatal deaths and hence, excluded from analysis. Among the remaining inborn neonatal deaths (n=58), 34 (59%) were males and 24 (41%) were females. The number of neonatal admissions increased over the years during the study period from 248 to 356, while the number of deaths also increased from 10 deaths in 2006, to 20 deaths in 2009. The primary causes of neonatal deaths were prematurity and its complications 52% (n=30). Lethal congenital malformations lead to 17 (29%) newborn deaths, specific diagnosis in 7 newborns (12%), and birth asphyxia in four (7%) of cases.
Conclusion: There was an increasing trend of neonatal admissions and deaths among inborn babies. Prematurity, with sepsis as its major complication and congenital malformations were the leading cause of neonatal mortality.
Keywords: Neonatal mortality; Prematurity; Oman.
Introduction
The Sultanate of Oman has experienced economic growth which was accompanied with improvement in many health indicators, including infant mortality rate. There are few studies that have described the neonatal mortality rates in Oman. The country has achieved a significant reduction in under-five mortality and infant mortality figures over the past two decades, which may be attributed to high standards of preventive and curative maternal and child health.1 According to the UNICEF registry on the level and trends in child mortality, neonatal mortality rates have tremendously dropped from a value of 22/1000 in 1990, to a minimum value of 6/1000 in 2010 in Oman.2 Similar reports from other gulf countries including Saudi Arabia and Qatar revealed neonatal mortality rate of 12/1000 and 5.1/1000, respectively.3,4
Earlier assessments by the World Health Organization have highlighted that about 25% of countries are on track towards reaching the Millennium Development Goal 4 (MDG 4), which calls for a two-thirds reduction in mortality of children under the age of 5 years between 1990 and 2015.5 Since the adoption of the MDG 4 policies by all United Nations member states in the year 2000, it is essential to determine whether there are any indications towards those goals. Since the etiological pattern of neonatal deaths in Oman has not been previously reported, this study was conducted specifically for that purpose.
The aim of this study, therefore, is to define the neonatal mortality rate and the relative importance of various causes of death among neonates who were admitted at the neonatal intensive care unit (NICU) and to compare the findings with other neighboring countries.
Methods
This was a retrospective, analytic and descriptive study of all inborn births and neonatal deaths at Sultan Qaboos University hospital (SQUH) over a four-year period (January 2006-December 2009). The hospital has an obstetric unit, but also accepts high risk deliveries from other health institutes in the region. The newborn service operates as a referral neonatal intensive care unit for other areas in the county. Data was collected on predesigned and approved data collection forms from the admissions and discharge registers at the NICU. The total number of live births was obtained from the Department of Obstetrics and Gynecology. Neonatal deaths were thoroughly discussed at the level of the unit, department and hospital mortality committee meetings as part of the morbidity and mortality studies carried out weekly by the hospital.
Wigglesworth classification was used to classify causes of neonatal deaths into the following five groups: still birth, congenital malformations, prematurity and its complications, asphyxia, and specific diagnosis.6 Data are expressed as rates (per 1000) and proportion of cases (%). Early neonatal death (END) is defined as death that occurs in up to six completed days following birth. Late neonatal death (LND) was defined as deaths between 7 and 27 days, while post-neonatal death (PND) was defined as death after 27 days of life until the age of 1 year.7 All out born and PND deaths were excluded from the study, thus only neonates born at SQUH obstetrics unit were included. Mortality among inborn neonates was paid particular attention because the mortality rate is a calculation of the rate of deaths among live births within the tertiary centre.
Data was analyzed using the SPSS program. The chi-square test, t-test, and one way ANOVA were used to determine the trend. The level of p<0.05 was considered as the cutoff value for significance.
Results
The number of inborn live births during the study period was 10064, out of which 1235 were admitted to the NICU. During the same period, there had been 240 out born NICU admissions that were excluded from the study. Inborn babies were only been included to calculate the neonatal mortality rate. The total number of deaths during the study period was 73, out of which 10 were out born neonates who were excluded. Of the remaining 63 deaths, five cases of PND (9%) were excluded from the study, giving the remaining total of 58 inborn neonatal deaths. END occurred in 42 (72%) neonates and LND occurred in 16 (28%). The neonatal death rates per 1000 live births per year are shown in Fig. 1, in relation to the number of neonatal admissions per year.
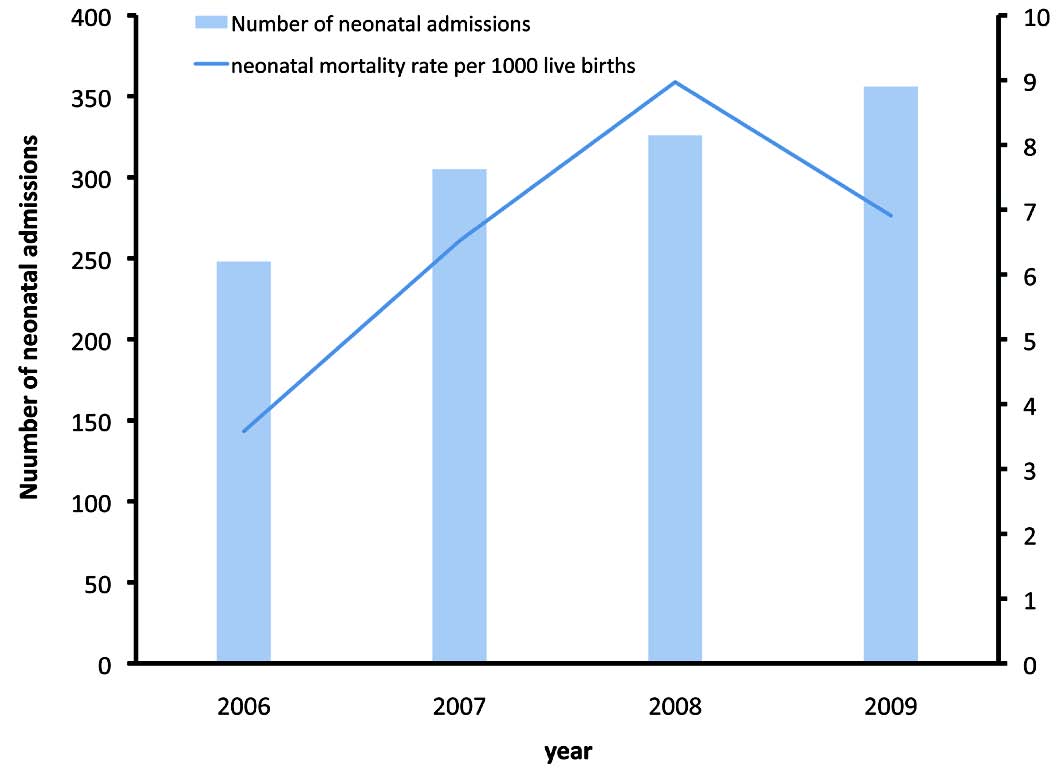
Figure 1: The number of neonates admitted per year, and the neonatal mortality rate at the NICU, SQUH, from 2006 to 2009.
There was an increasing trend in the number of neonatal admissions gradually over the four-year period (p=0.091). The neonatal mortality rate per 1000 live births was 5/1000 in 2006, 7/1000 in 2007, 9/1000 in 2008, and 8/1000 in 2009 (p=0.110). There was also a decreasing trend in the mortality rate in the last year, despite the increase in admissions to the unit. The overall neonatal mortality rate over the four years was 6/1000 (n=58), early neonatal mortality rate 4/1000 (n=42), and late neonatal mortality rate was 2/1000 (n=16).
Prematurity with its complications was the major cause of neonatal mortality. Of the 30 premature babies that died, 13 (43%) neonates were born at less than 26 weeks of gestation. The majority of deaths in this group were noted in babies less than one kilogram, which constituted 23 (77%) out of the total number of premature neonatal deaths. The major cause of death in this group was neonatal sepsis accounting for 12 (40%) cases of deaths. (Table 1)
Table 1: The distribution and causes of death according to the modified Wigglesworth classification among neonatal admissions in the neonatal intensive care unit at Sultan Qaboos University Hospital (2006-2009).
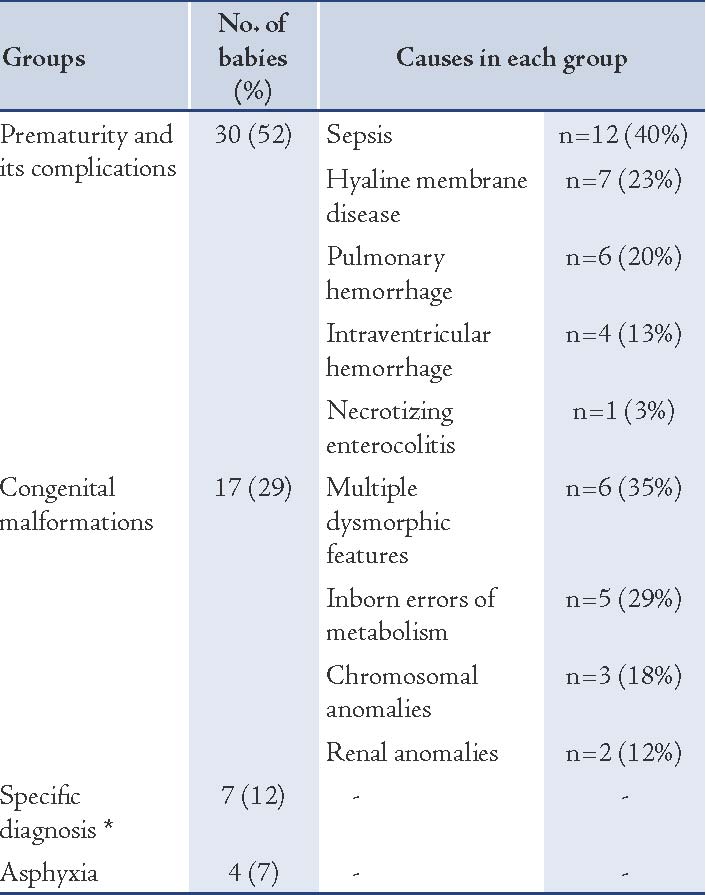
Furthermore, the number of deaths was found to be higher at lower gestational ages (p<0.001), as shown in Fig. 2. The difference between the groups of premature neonates, in terms of complications of prematurity was not particularly significant (using one-way ANOVA; p=0.137). The sex distribution showed that 34 (59%) were males and 24 (41%) were females, and of the total number of the male neonatal deaths, 16 (47%) neonates died due to prematurity and its complications, 11 (32%) of died as a result of multiple congenital anomalies, 3 (9%) died due to birth asphyxia, and 5 (15%) died due to a specific diagnosis. On the other hand, of the 24 female neonates, 12 (50%) died due to prematurity and its complications, 6 (25%) died due to lethal congenital malformations, 3 (13%) died due to a specific diagnosis, and 1 (4%) died due to birth asphyxia.
Among the five cases of PND, three infants died due to lethal congenital malformations (including trisomy 18), one died due to grade IV intraventricular hemorrhage, and one due to sepsis. Out of the ten out-born babies, 50% died due to lethal congenital malformations. This reflects the high risk referrals from other hospitals due to prenatal diagnosis by way of ultrasound.
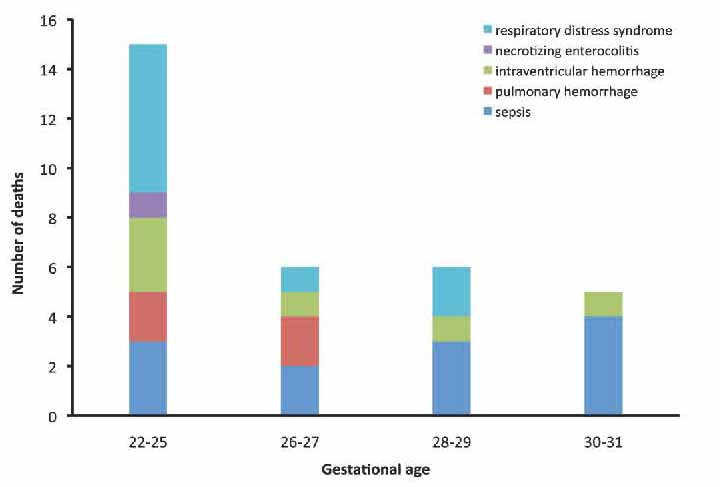
Figure 2: The causes of death in the group who died due to prematurity, according to gestational age at Sultan Qaboos University Hospital, (2006 - 2009).
Discussion
Neonatal mortality is a reliable index for evaluating the overall progress of neonatal and perinatal care in a community, which is a valuable indicator of the standard of a country’s educational, social and community health system, the nutritional status of the population and the national medical programs in obstetrics and neonatal care.8 The countries of the Gulf Cooperation Council (GCC), which include Oman have made an outstanding success in improving the neonatal mortality rate in the last two decades.9
In this study, the distribution and causes of death during the neonatal period from admission to the NICU at SQUH was grouped according to the Wigglesworth’s classification. According to this study, the two leading causes of neonatal deaths were prematurity (52%) and congenital anomalies (29%), which is similar to reports from other neighboring countries in the Middle East,10-13 and Western countries where a study from the United Kingdom confirmed that the commonest causes of neonatal death were prematurity (39%), followed by congenital anomalies (28%) and intrapartum hypoxia (13%).14
Among the premature neonates, 63% of the deaths occurred in babies of less than 28 weeks gestational age. Sepsis was the leading cause of death among the premature neonates, all of whom died due to gram negative sepsis. In fact sepsis has been reported to be one of the major causes of neonatal death in some of the gulf countries but not in developed countries,15,16 with gram-negative organisms attributed to be the leading causative agents in neonatal sepsis in developing countries.17,18 Gram-positive organisms, particularly group B streptococcus (GBS), have been reported to be the predominant organism in North America.18 This might be due to the fact that 25% of pregnant women in the West are colonized with GBS.18 There are no established reports about the nature of the inhabitants of the genitourinary and gastrointestinal tracts of pregnant women in Oman. Death due to neonatal sepsis alone occurred in 12 (38%) cases, a figure which may be considered to be comparatively higher than those for other causes of neonatal mortality in the category of premature babies. This indicates the need for strict infection control guidelines. Data from the National Institute of Child Health and Human Development-sponsored "Neonatal Network" indicated that neonatal sepsis can be responsible for almost 50% of late neonatal death.19
Furthermore, as shown in Fig. 2, respiratory distress syndrome/hyaline membrane disease (HMD), was evident to be the commonest cause of death among the neonates who were born at 22 to 25 weeks of gestation. HMD resulted in the deaths of 7 (23%) of the premature neonates. HMD was a major cause of mortality and morbidity in pre-term neonates during the pre-surfactant era (before mid 1990s). However, with the liberal use of antenatal steroids and postnatal surfactant therapy, this has now become a rarity. Also, pulmonary hemorrhage resulted in 6 (20%) deaths, making necrotizing enterocolitis the least common cause of death in premature babies, resulting in 1 (3%) death only. Never to underestimate, necrotizing enterocolitis is a serious complication of prematurity which is difficult to manage, placing the patient’s life in great jeopardy.
In this study, 17 inborn babies died due to lethal congenital malformations, the commonest cause was found to be multiple dysmorphic features, which did not have a definite diagnosis in spite of extensive investigations. The second most common cause in the same group was inborn errors of metabolism (5 neonates), of which four cases died due to organic acidemia. The most common chromosomal anomalies were trisomy 18 in three patients, and trisomy 21 in one neonate. The rest were due to renal anomalies resulting in Potter’s syndrome.
The fact that lethal congenital malformation was the second commonest cause of death could be explained partially by the high degree of consanguineous marriages in Oman. Consanguineous marriage is significantly associated with congenital malformation.20 Published data from the Sultanate of Oman revealed that congenital malformations compose a major cause of mortality, morbidity and chronic handicap.21,22 The outline and prevalence of congenital anomalies may differ over time or geographical location, thereby reflecting a complex interaction of known and unknown genetic and environmental factors including sociocultural, racial and ethnic variables.23 Accurate quantification of congenital anomalies within a given population is essential for estimating their burden and documenting the need for prevention.24 Thereby a thorough critical investigation is essential to establish the likely hereditary, socio-demographic and socioenvironmental factors underlying the different types of congenital malformations encountered. Though the importance of timely, accurate and specific diagnosis of congenital malformations in the newborn period to optimize outcome has been emphasized, it has also been stressed that a specific diagnosis may not be reached for 30% to 60% of infants with malformations and that diagnosis is not always apparent in the newborn period.23
Birth asphyxia has been attributed to be the cause of death in 4 (7%) neonates, of whom all were inborn neonates. Even though birth asphyxia was not a major problem in Oman, it has been reported to be the primary cause of death in other developed countries.3,25 This indicates a good progress in the quality of the perinatal care services, and the significance of intrapartum fetal monitoring, as well as the modes of delivery and the availability of trained personnel in Oman. In addition, 7 (12%) deaths were due to specific diagnoses, which included the following conditions: Dandy Walker, primary microcephaly and Intestinal obstruction/perforation, term baby with necrotizing enterocolitis, arthrogryposis multiplex, skeletal dysplasia, and congenital lymphangiectasia.
The overall morality was higher among male infants during the study period. It is well acknowledged that mortality rates for boys in the early neonatal period are higher than those for girls.26 Prematurity and its complications was the leading cause of deaths among neonates admitted to the NICU at SQUH with neonatal sepsis being the primary cause of death in premature infants, thus indicating that strict infection guidelines need to be implemented.
A good statistical background concerning neonatal mortality is required for mounting a reliable plan for the rapid identification and management of neonatal morbidities. The data should preferably be based on entire population surveillance. However, whatever statistics available are only hospital-based. In spite of such a restriction, the hospital-based statistics can still be valuable in indicating the pattern of neonatal morbidity and mortality in a given population. The evaluation of the outcome of the newborns at a given institution gives very helpful information on the performance of their perinatal and neonatal services.
This study has shown that there is an annual increment in the total number of neonatal admissions to the NICU, from 2006 to 2009, which indicates the increase in demand for perinatal and neonatal services at SQUH (Fig. 1). This has also been reflected by the increase in neonatal mortality rates. This can be attributed to the increasing rate of high risk obstetric case referrals from other hospitals and the presence of qualified perinatologists who joined lately. The fetomaternal unit and assisted reproduction were started around 2005, which resulted in a steady increase in the number of preterm and multiple births, and high risk obstetric referrals to NICU. The obstetric unit at SQUH is considered to be one of the two main high-risk referral centers for deliveries in Oman, the other is in Royal Hospital. There are other facilities that operate at Levels 2 and 3 in Oman. Therefore, the neonatal mortality data from SQUH does not represent the overall national neonatal data for the whole country.
A further addition to the study is to include the stillbirths at SQUH. Neonatal mortality data from other tertiary centres in Oman can be gathered to determine its pattern in the whole of Oman. Consistent published data on the pattern of neonatal mortality and the definite causes of death are sparse in Oman, which makes it difficult to calculate the precise mortality rates. Furthermore, civil registration data are incomplete to some degrees, and there are inconsistencies in defining reported standards.
Conclusion
The study aimed to stress the need to establish a database system in all central institutions in Oman. This will therefore help to oversee the healthcare development within the institutions and in the country as a whole.
Acknowledgements
The authors reported no conflicts of interest and no funding was received for this work.
References
1. Bhutta ZA, Chopra M, Axelson H, Berman P, Boerma T, Bryce J, et al. Countdown to 2015 decade report (2000-10): taking stock of maternal, newborn, and child survival. Lancet 2010 Jun;375(9730):2032-2044.
2. Level & Trends in Child Mortality. Report 2011. Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation (UNICEF, WHO, World Bank, UN DESA, UNPD.
3. World Health Organization. World Health Rep 2005;•••:1-243.
4. World health organization. Neonatal and Perinatal Mortality. Country, Regional and Global Estimates. 2006; 1-75.
5. World Health Organization. The Millennium Development Goals Report 2007; 1-21.
6. Wigglesworth JS. Monitoring perinatal mortality. A pathophysiological approach. Lancet 1980 Sep;2(8196):684-686.
7. World Health Organization. 2006 Neonatal and Perinatal Mortality Country, Regional and Global Estimates. (http://www.who.int/making_pregnancy_safer/publications/neonatal.pdf
8. Yu YH. Victor Global, regional and national perinatal and neonatal mortality. J Perinal med 2003; 31:376-379.
9. Boutayeb A, Serghini M. Health indicators and human development in the Arab region. Int J Health Geogr 2006;5:61.
10. Mansouri H. Perinatal mortality at King Abdulaziz University Hospital, Jeddah, Saudi Arabia. Saudi Med J 1996;17:176-179.
11. English JD. Perinatal mortality at the North West Armed Forces Hospital, Tabuk, Saudi Arabia and the potential benefits of the biophysical profile score. Ann Saudi Med 1995 Mar;15(2):133-136.
12. Majeed-Saidan MA, Kashlan FT, Al-Zahrani AA, Ezzedeen FY, Ammari AN. Pattern of neonatal and postneonatal deaths over a decade (1995–2004) at a Military Hospital in Saudi Arabia. Saudi Med J 2008 Jun;29(6):879-883.
13. Salameh K, Rahman S, Al-Rifai H, Masoud A, Lutfi S, Abdouh G, et al. An analytic study of the trends in perinatal and neonatal mortality rates in the State of Qatar over a 30-year period (1977 to 2007): a comparative study with regional and developed countries. J Perinatol 2009 Nov;29(11):765-770.
14. Bell R, Glinianaia SV, Rankin J, Wright C, Pearce MS, Parker L. Changing patterns of perinatal death, 1982-2000: a retrospective cohort study. Arch Dis Child Fetal Neonatal Ed 2004 Nov;89(6):F531-F536.
15. UNICEF. State of the World’s Children. 2007; 102-105.
16. World Health Organization. World Health Rep 2005;•••:1-243.
17. Aletayeb S, Khosravi A, Dehdashtian M. Identification of bacterial agents and antimicrobial susceptibility of neonatal sepsis: A 54-month study in a tertiary hospital, African Journal of Microbiology Research; 201; 5(5):528-531.
18. Falciglia G, Hageman JR, Schreiber M, Alexander K. Antibiotic Therapy and Early Onset Sepsis. Neoreviews 2012;13:e86 .
19. Hristeva L, Booy R, Bowler I, Wilkinson AR. Prospective surveillance of neonatal meningitis. Arch Dis Child 1993 Jul;69(1 Spec No):14-18.
20. Baird PA, Sadovnick AD, Yee IM. Maternal age and birth defects: a population study. Lancet 1991 Mar;337(8740):527-530.
21. Sawardekar KP. Genetic analysis of lethal congenital malformations causing perinatal mortality at Nizwa Hospital, Oman. Clin Genet 2004 Sep;66(3):239-243.
22. Rajab A, Vaishnav A, Freeman NV, Patton MA. Neural tube defects and congenital hydrocephalus in the Sultanate of Oman. J Trop Pediatr 1998 Oct;44(5):300-303.
23. AIHW NPSU. BirchM-R, Grayson N, Sullivan EA. Recommendations for development of a new Australian birth anomalies system: A review of the congenital malformations and birth defects data collection. AIHW Cat. No. PER 23. Sydney: AIHW National Perinatal Statistics Unit (Birth Anomalies Series no. 1), 2004.
24. Rajeev A, Jayalekshemi BR, Rekha S. Correlation of Early Neonatal Mortality and Technical Efficiency of Regional Maternal and Child Health Services in Oman. Oman Med J 2010 Jan;25(1).
25. Bell R, Glinianaia SV, Rankin J, Wright C, Pearce MS, Parker L. Changing patterns of perinatal death, 1982-2000: a retrospective cohort study. Arch Dis Child Fetal Neonatal Ed 2004 Nov;89(6):F531-F536.
26. de la Garza Quintanilla C, González Salinas MV. [Perinatal mortality]. Ginecol Obstet Mex 1995 May;63:186-189.
|