A five-year-old previously healthy male child presented to a tertiary center in Oman with a one-day history of high-grade fever reaching up to 39 oC, left knee pain, swelling, and restricted movements. There was no history of preceding infectious symptoms, trauma, animal exposure, or travel. His immunization was up-to-date. He was born at 33 weeks of gestation, and at two weeks of life, he was managed for culture-negative septic arthritis complicated by osteomyelitis of the proximal tibia. He underwent a left knee arthrotomy and was managed with six weeks of intravenous antibiotics. He made a full recovery. The physical examination revealed a temperature of 39 oC, associated with tachycardia of 149 beats/minute and tachypnea of 32 breaths/minute. His left leg was fixed and flexed, and his left knee was swollen, erythematous, hot, tender, and externally rotated with a healed scar from the previous surgery. The other systemic examinations were unremarkable. Initial investigations revealed leukocytosis (white blood cells) of 18.2 × 109/L (4.5 – 14.5 × 109/L) and a C-reactive protein of 309 mg/L (0–5 mg/L). Magnetic resonance imaging of the left knee showed a moderate left knee joint effusion with complex internal contents, septa, and thickened and enhanced synovium with extensive periarticular soft tissue edema [Figure 1]. Gram-positive cocci in chains grew from the joint fluid. Informed consent was obtained from the patient’s family.
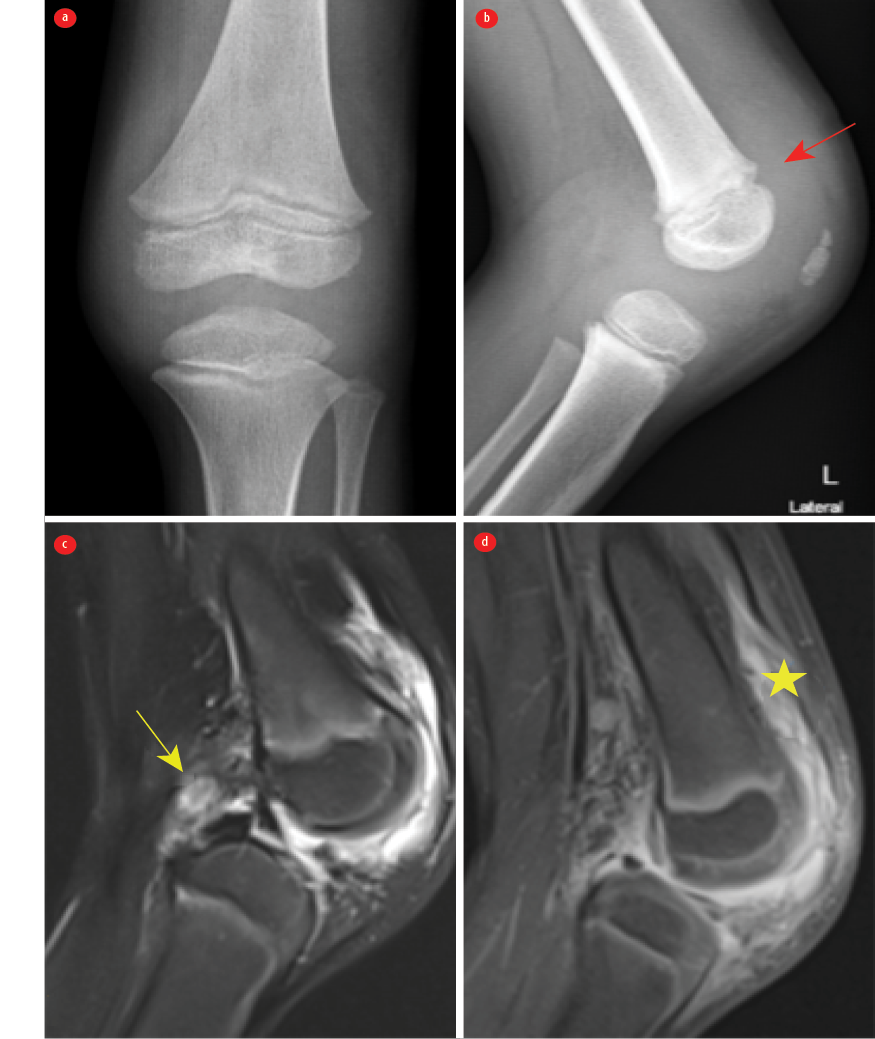 Figure 1: Radiographs of the left knee (a) anteroposterior and (b) lateral views revealed periarticular soft tissue swelling, which is better seen on the lateral radiograph. We observed suprapatellar pouch effusion (red arrow). No fractures or destructive bony lesions were observed, and the joint space was preserved. (c) Sagittal T2 FS MRI of the knee showing enlarged lymph nodes in the popliteal fossa were also noted (yellow arrow). (d) Post-contrast T1 FS MRI of the knee revealed a small knee joint effusion with synovial thickening and periarticular soft tissue edema. There was thick enhancing synovium on the post-contrast images (star).
Figure 1: Radiographs of the left knee (a) anteroposterior and (b) lateral views revealed periarticular soft tissue swelling, which is better seen on the lateral radiograph. We observed suprapatellar pouch effusion (red arrow). No fractures or destructive bony lesions were observed, and the joint space was preserved. (c) Sagittal T2 FS MRI of the knee showing enlarged lymph nodes in the popliteal fossa were also noted (yellow arrow). (d) Post-contrast T1 FS MRI of the knee revealed a small knee joint effusion with synovial thickening and periarticular soft tissue edema. There was thick enhancing synovium on the post-contrast images (star).
Questions
- What is the diagnosis?
- What is the gold standard test to make the diagnosis?
- What is the most common organism causing this infection in healthy children?
- How would you manage the patient?
Answers
- Left knee septic arthritis.
- Joint fluid aspiration for bacterial culture.
- Staphylococcus aureus.
- Anti-staphylococcus penicillin or first-generation cephalosporin, like cefazolin, as empiric antibiotics and then targeted antibiotic therapy according to the culture results.
Discussion
The enhancement suggests features of septic arthritis and synovitis, with no evidence osteomyelitis or a sizable collection [Figure 1]. He was started on intravenous cefazoline and underwent a left knee open arthrotomy. Streptococcus agalactiae, susceptible to ampicillin, grew from his synovial fluid. He was slow to improve after the first arthrotomy, but improved significantly after the second, which was done 12 days after the first procedure. He was managed with three weeks of antibiotics post the second washout. He had a full recovery at the two-month follow-up.
Group B streptococci (GBS) are a major cause of perinatal infections in pregnant women and can cause invasive infections in neonates.1 GBS invasive infections are rare beyond infancy.1 People with underlying medical conditions are reported to be the most vulnerable group to GBS infection, especially obese patients, patients with poor glycemic control, and immunocompromised patients.2 Phares et al,1 reported 233 (1.6%) cases of invasive GBS infection in children aged 90 days through 14 years in a population-based surveillance of GBS infection across 10 American states between 1999 and 2005 from a total of 14 573 cases with GBS disease. Only 5% of childhood invasive GBS disease in this cohort manifested as septic arthritis, while 58% presented as bacteremia without focus. Nearly half (44%) of infected patients, aged 1–14 years, with invasive GBS disease had at least one underlying medical conditions.2 The most common comorbidities in this study were neurological disorders (25%), followed by immunosuppressive conditions (23%), asthma (23%), malignancy (15%), and renal disease (13%). Besides having early septic arthritis during the neonatal period, our patient has been previously healthy with no known underlying medical conditions.
There is limited data regarding GBS septic arthritis beyond infancy.2 Most GBS septic arthritis cases are monoarticular, with the knee being the most affected joint in an extensive adult study, followed by the shoulder and ankle joints.3 A study from Singapore, comparing adult patients with and without GBS septic arthritis reported that patients with GBS septic arthritis tend to have significantly higher CRP, a higher rate of bacteremia, a longer hospital stay, and a longer duration of treatment, while the rates of mortality and limb loss were lower, which may not be the same in children.4 Our patient required arthrotomy twice during his illness and was slow to improve. He stayed at the hospital for three weeks for intravenous antibiotics before discharge, but achieved full recovery. Pediatricians should be aware that GBS can cause osteoarticular infections beyond infancy, particularly in children with underlying medical conditions, but not exclusively.
Disclosure
The authors declare no conflicts of interest.
references
- 1. Phares CR, Lynfield R, Farley MM, Mohle-Boetani J, Harrison LH, Petit S, et al; Active Bacterial Core surveillance/Emerging Infections Program Network. Epidemiology of invasive group B streptococcal disease in the United States, 1999-2005. J AMA 2008 May;299(17):2056-2065.
- 2. Trehan I, Fritz SA, Group B, Group B. Group B Streptococcus vertebral osteomyelitis-discitis in an immunocompetent adolescent. Pediatr Infect Dis J 2009 Jun;28(6):552-553.
- 3. Ruksasakul R, Narongroeknawin P, Assavatanabodee P, Chaiamnuay S. Group B streptococcus is the most common pathogen for septic arthritis with unique clinical characteristics: data from 12 years retrospective cohort study. BMC Rheumatol 2019 Sep;3(1):38.
- 4. Wang VT, Tan JH, Pay LH, Wu T, Shen L, O’Neill GK, et al. A comparison of Streptococcus agalactiae septic arthritis and non-Streptococcus agalactiae septic arthritis. Singapore Med J 2018 Oct;59(10):528-533.