A 21-year-old man, who was a heavy smoker, presented to his local health center with a history of pain, numbness, tingling, and swelling in his fingers and both palms, along with cold sensitivity. His symptoms started suddenly one hour after his daily outdoor walk. He had similar attacks previously, which occurred without a specific reason and lasted for variable amounts of time. He had no history of trauma, joint pain, rash, shortness of breath, or visual problems. On examination, the patient was comfortable in room air. His vital signs were within normal ranges. Color changes, including white, red, and blue discoloration, are shown in Figure 1. His complete blood count, inflammatory markers, anti-nuclear antibody, and rheumatoid factor test were unremarkable. Informed consent was obtained from the patient.
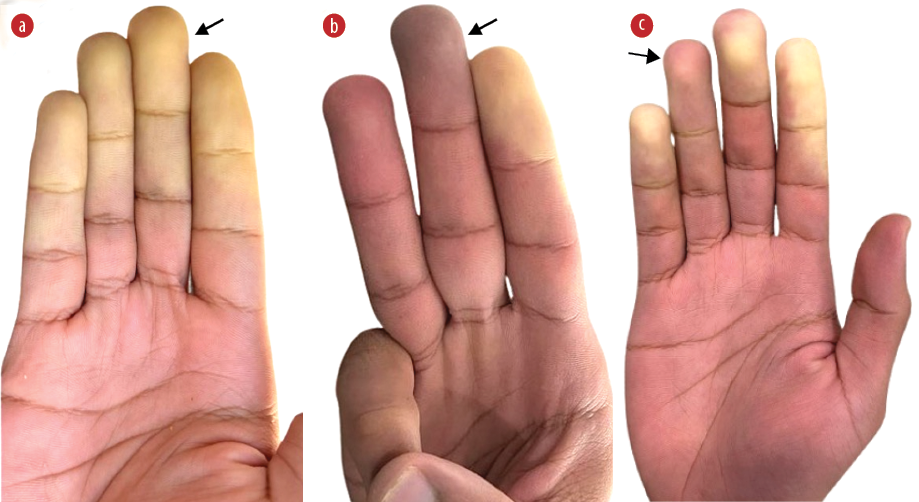 Figure 1: The hand of a young male after exposure to cold showing (a) white, (b) blue, and (c) red color changes (arrows).
Figure 1: The hand of a young male after exposure to cold showing (a) white, (b) blue, and (c) red color changes (arrows).
Question
1. What is the diagnosis?
a. Multiple sclerosis.
b. Scleroderma.
c. Raynaud’s phenomenon.
d. Rheumatoid arthritis.
Answer
c. Raynaud’s phenomenon (RP).
A primary RP diagnosis was made. The patient was advised to avoid exposure to cold weather, stop smoking, and do regular exercise, as this improves circulation. He was started on nifedipine 30 mg daily for one month.
Discussion
RP is an abnormal response to cold or emotional stress.1 It has a characteristic clinical presentation of episodic vasoconstriction in the fingers associated with skin color changes, including white (blanching secondary to vasoconstriction) [Figure 1a], blue (cyanosis secondary to deoxygenation) [Figure 1b], and red (post-ischemic hyperemia) [Figure 1c].2,3 However, the presence of all three color changes is not mandatory for diagnosis.4
Many factors can trigger RP, such as smoking, cold weather, sympathomimetic agents, and the use of vibratory tools.2 Moreover, the severity of RP can be affected by subclinical atherosclerosis and a low body mass index, which can affect the physiological thermoregulatory response.2
Based on the underlying etiology, the disease can be classified as either primary or secondary RP.1,2 Primary RP is the most common form, which is caused by functional vasospastic disorder.1,2 This form is reversible and benign. It may be associated with pain and numbness, which affect the hand’s functions.1,2 The secondary RP has a wide range of pathological causes, including rheumatological, hematological, endocrine, and vascular diseases.1,2 Specifically, conditions such as hand-arm vibration syndrome, carpal tunnel syndrome, hypothyroidism, connective tissue diseases such as systemic lupus erythematosus, systemic sclerosis, and vasculitis, and drug-related conditions such as the use of beta-blockers, amphetamines, and cyclosporine, and other reported conditions can result in the secondary type of RP.1,2 Thus, it can result in a variety of clinical presentations and have different effects on each patient.2 The secondary RP might progress to ulceration, scarring, or gangrene.1
Laboratory testing for RP depends on the clinical presentation of each patient.2 However, it should include the main investigations, such as a complete blood count, inflammatory markers, anti-nuclear antibody test, and thyroid function tests, to exclude any secondary cause.2 The laboratory results of our patient excluded any secondary cause for his RP, suggesting the primary type of disease.
Treatment of RP focuses on encouraging vasodilatation and/or suppressing vasoconstriction.1 Supportive treatment is the primary line of treatment in mild cases, which includes avoiding cold exposure, smoking cessation, and lifestyle modifications.3 In addition, vasoconstriction stimulation substances, such as caffeine, ergot alkaloids, beta-blockers, amphetamines, and cocaine should be avoided.3
Pharmacological treatment is necessary in cases where conservative treatment alone is insufficient.3 Commencing medical treatment for RP is based on its efficacy in each patient’s condition and the severity of their symptoms.2 In general, calcium channel blockers (CCBs) are the primary pharmacological treatment for RP.3 However, the long-term effects of CCBs are still unknown.5 It might reduce the frequency and severity of RP attacks, particularly in primary RP.5 Although critical side effects are rare, discontinuation of CCBs is required if side effects develop, such as hypotension, peripheral edema, and flushing.5 It is worth noting that our patient refused the use of nifedipine after knowing its possible side effects.
Disclosure
This report was conducted in accordance with the principles of the Helsinki Declaration, and it was ethically waved by the Research and Research Ethics Committee, Salmaniya Medical Complex, Government Hospitals, Bahrain.
references
- 1. Herrick AL. The pathogenesis, diagnosis and treatment of Raynaud phenomenon. Nat Rev Rheumatol 2012 Aug;8(8):469-479.
- 2. Pauling JD, Hughes M, Pope JE. Raynaud’s phenomenon-an update on diagnosis, classification and management. Clin Rheumatol 2019 Dec;38(12):3317-3330.
- 3. Block JA, Sequeira W. Raynaud’s phenomenon. Lancet 2001 Jun;357(9273):2042-2048.
- 4. Maverakis E, Patel F, Kronenberg DG, Chung L, Fiorentino D, Allanore Y, et al. International consensus criteria for the diagnosis of Raynaud’s phenomenon. J Autoimmun 2014;48-49:60-65.
- 5. Rirash F, Tingey PC, Harding SE, Maxwell LJ, Tanjong Ghogomu E, Wells GA, et al. Calcium channel blockers for primary and secondary Raynaud’s phenomenon. Cochrane Database Syst Rev 2017 Dec;12(12):CD000467.