Acute lymphoblastic leukemia (ALL) is the most common malignancy in childhood, accounting for approximately one-third of all pediatric cancers.1 Typical clinical presentations include symptoms such as pallor, fatigue, fever, easy bruising and bleeding, and bone pain,2 which are further supported by clinical findings of cytopenia, organomegaly, and lymphadenopathy. Although bone pain has been reported to occur in around 30–40% of ALL patients, clinical arthritis as the sole presenting feature of pediatric ALL is rare.3–5
Case Report
A five-year-old boy was referred to the rheumatology clinic with a five-month history of migratory joint pain. His symptoms began as nonspecific pain in the knees, ankles, shoulders, and back with no visible swelling. He had no history of fever, morning stiffness, or preceding illness. The joint pain was worse at night, which, with time, rendered him immobile. He was still able to use his upper limbs freely. He had occasional vomiting and loss of appetite, but no weight loss.
Upon assessment, the child was in a wheelchair. His biometric and developmental indicators were age-appropriate. He showed no signs of pallor, rashes, or lymphadenopathy. Cardiovascular, chest, and abdominal examinations were all unremarkable. His left knee was significantly swollen and tender, and the right ankle had limited flexion. There was significant bilateral leg muscle atrophy but power and reflexes were normal. As the child could not walk, his gait and Gower’s sign could not be assessed.
The patient was admitted for pain control and further investigations. His laboratory findings are listed in Table 1.
Table 1: Laboratory investigation results of
the patient.
|
Hemoglobin, g/dL
|
11.8 (11.5–15.5)
|
|
Platelets, × 109/L
|
433 (150–450)
|
|
WBC, × 109/L
|
5.6 (4.5–14.5)
|
|
ANC, × 109/L
|
2.1 (1.4–9.0)
|
|
Lymphocyte, × 109/L
|
3.0 (1.9–9.8 )
|
|
Urea and electrolytes
|
Normal
|
|
CRP
|
21 (< 1)
|
|
ESR
|
60 (< 10)
|
|
TB, Brucellosis, Q fever, syphilis, toxoplasmosis, hepatitis, ASOT, HIV, Mycoplasma pneumonia
|
All negative
|
|
LFT
|
Normal
|
|
TFT
|
Normal
|
|
Mg
|
Normal
|
|
Uric acid
|
Normal
|
|
LDH
|
Normal
|
|
CK
|
Normal
|
|
Urine PCR
|
Normal
|
|
ANA
|
+ve 1:80 (low titer)
|
WBC: white blood cell; ANC: absolute neutrophil count; CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; TB: tuberculosis; ASOT: antistreptolysin O titer; LFT: liver function test; TFT: thyroid function test; Mg: magnesium; LDH: lactate dehydrogenase; CK: creatine kinase; PCR: polymerase chain reaction; ANA: antinuclear antibody; ENA: extractable nuclear antigen.
The chest X-ray and abdominal ultrasound images were normal. However, the X-ray of the left knee showed heterogeneous lucencies with diffuse erosions [Figure 1].
 Figure 1: X-ray image of the left knee showing heterogeneous lucencies of the distal femoral metaphysis, proximal tibial metaphysis, and proximal fibular metaphysis with diffuse erosions.
Figure 1: X-ray image of the left knee showing heterogeneous lucencies of the distal femoral metaphysis, proximal tibial metaphysis, and proximal fibular metaphysis with diffuse erosions.
The patient’s whole-body magnetic resonance imaging (MRI) revealed multifocal heterogeneous areas of T2 hyperintensity affecting almost all bones, including the sternum, pelvis, and phalanges of the hands and feet. The left knee joint had a small effusion. Similar radiographic changes were observed in the humerus, radius, ulna, carpals, metacarpals, femurs, tibias, fibulas, tarsal, sternum, scapulae, clavicles, multiple spinal processes, posterior-superior iliac spines, iliac crests, and phalanges. Features were in keeping with those of chronic recurrent multifocal osteomyelitis (CRMO) [Figure 2].
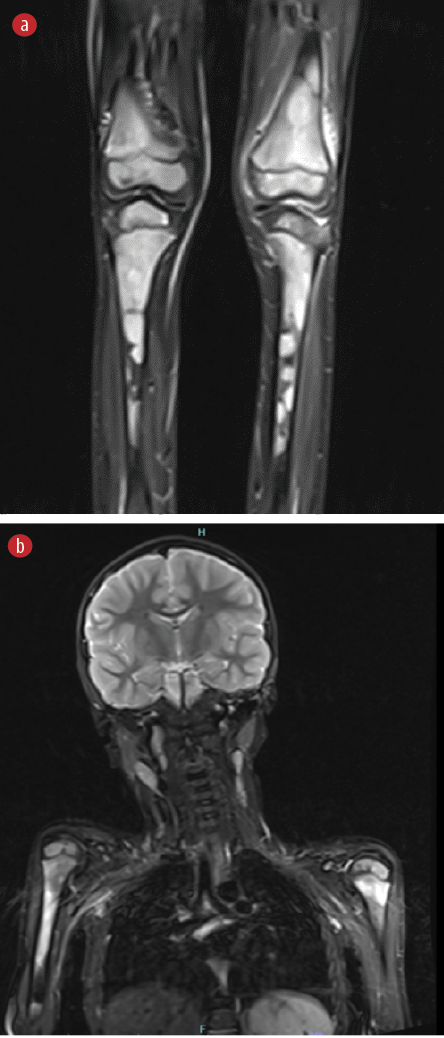 Figure 2: Details from the whole-body MRI. Multifocal heterogeneous areas of T2 hyperintensity affecting mainly the long bones (epiphysis, metaphysis, and diaphysis, with affinity to metaphysis). Also, periosteal elevation and surrounding soft tissue edema at the distal left femur and proximal left tibia, with focal thinning of the cortex of the tibia. Small joint effusion of the left knee. The brain parenchyma is unremarkable.
Figure 2: Details from the whole-body MRI. Multifocal heterogeneous areas of T2 hyperintensity affecting mainly the long bones (epiphysis, metaphysis, and diaphysis, with affinity to metaphysis). Also, periosteal elevation and surrounding soft tissue edema at the distal left femur and proximal left tibia, with focal thinning of the cortex of the tibia. Small joint effusion of the left knee. The brain parenchyma is unremarkable.
A bone biopsy taken from the left femur revealed replacement of the marrow by sheets of immature blasts. Blood film, bone marrow aspirate, and flow cytometry showed that 66% of the blasts exhibited features consistent with precursor B-cell acute lymphoblastic leukemia , characterized by a common B-immunophenotype (WHO 2017).
The patient was started on UKALL 2011-Regimen A, and he continues to show favorable response at the time of writing this report. Informed consent was obtained from the patient's mother for the publication of this case.
Discussion
While the pathogenesis of arthritis in ALL remains poorly understood, it has been proposed that leukemic cells infiltrate the synovium, causing joint inflammation and subsequent arthritis-like symptoms.6,7
Juvenile idiopathic arthritis (JIA) is the most common chronic autoimmune disorder in children under the age of 16.8 Arthritis-like symptoms in ALL can be misinterpreted as JIA if they present with multiple joint involvement for more than six weeks, antinuclear antibody (ANA) positivity, and no cell line abnormalities.3
Our patient presented with a significantly tender knee, an inability to bear weight, disturbed sleep, and repeated vomiting, which, when put together, did not favor a diagnosis of JIA, triggering the search for other differential diagnoses. He had a low positive ANA titer of 1:80 with negative dsDNA and extranuclear antibodies, rendering connective tissue disorders less likely. Due to its non-specificity and the possibility that it may also be present in non-rheumatic disorders such as infections and malignancies, ANA should not be used to distinguish between these conditions.9
The uniqueness of this case lay in its MRI findings, which suggested a diagnosis of CRMO, a rare autoinflammatory bone disorder characterized by recurrent episodes of bone inflammation that predominantly affects the clavicle, sternum, vertebrae, and metaphyses of long bones.10 CRMO of small bones appears to be less common.11 Despite the typical radiological appearance characterized by osteolysis, sclerosis, and hyperostosis, we did not find them distinctive enough for a definitive diagnosis of CRMO.12,13 In such junctures, misinterpretation of MRI and biopsy results is known to occur.14,15
Our patient’s long-standing, typical clinical findings; symmetrical, multifocal radiological involvement; normal blood cell counts; and elevated inflammatory markers in the absence of fever collectively appear to fulfill the two commonly used pediatric diagnostic criteria for CRMO: the Bristol and Jansson criteria.16,17 However, his extreme pain and widespread bone marrow enhancement necessitated a bone biopsy, which confirmed a different diagnosis—that of pre-B-cell leukemia, the most prevalent form of ALL. Indeed, several studies have reported the absence of blasts in ALL patients who presented with musculoskeletal complaints.18,19
Conclusion
A high level of clinical suspicion and a comprehensive diagnostic approach are crucial when encountering a patient with atypical joint symptoms such as intense pain, nocturnal symptoms, and the absence of morning stiffness. This case highlights the importance of considering that clinical arthritis in a child can be a presenting feature of pediatric malignancy, even in the absence of cytopenia, fever, lymphadenopathy, or hepatosplenomegaly.
Disclosure
The authors declare no conflicts of interest.
Acknowledgments
We are grateful to our patient and his parents for their participation.
references
- 1. Zahnreich S, Schmidberger H. Childhood cancer: occurrence, treatment and risk of second primary malignancies. Cancers (Basel) 2021 May;13(11):2607.
- 2. Clarke RT, Van den Bruel A, Bankhead C, Mitchell CD, Phillips B, Thompson MJ. Clinical presentation of childhood leukaemia: a systematic review and meta-analysis. Arch Dis Child 2016 Oct;101(10):894-901.
- 3. Demir F, Eroglu N, BAHADIR A, Kalyoncu M. A case of acute lymphoblastic leukemia mimicking juvenile idiopathic arthritis. North Clin Istanb 2019;6(2):184-188.
- 4. Hann IM, Gupta S, Palmer MK, Morris-Jones PH. The prognostic significance of radiological and symptomatic bone involvement in childhood acute lymphoblastic leukaemia. Med Pediatr Oncol 1979;6(1):51-55.
- 5. Sadawaite S, Jijina F, Nair CK, Seth S, Ghosh K. An unusual presentation of pediatric acute lymphoblastic leukemia. Indian J Hematol Blood Transfus 2008 Jun;24(2):59-62.
- 6. Trapani S, Grisolia F, Simonini G, Calabri GB, Falcini F. Incidence of occult cancer in children presenting with musculoskeletal symptoms: a 10-year survey in a pediatric rheumatology unit. Semin Arthritis Rheum 2000 Jun;29(6):348-359.
- 7. Zombori L, Kovacs G, Csoka M, Derfalvi B. Rheumatic symptoms in childhood leukaemia and lymphoma-a ten-year retrospective study. Pediatr Rheumatol Online J 2013 May;11(1):20.
- 8. Martini A, Ravelli A, Avcin T, Beresford MW, Burgos-Vargas R, Cuttica R, et al; Pediatric Rheumatology International Trials Organization (PRINTO). Toward new classification criteria for juvenile idiopathic arthritis: first steps, pediatric rheumatology international trials organization international consensus. J Rheumatol 2019 Feb;46(2):190-197.
- 9. Vermeersch P, Bossuyt X. Prevalence and clinical significance of rare antinuclear antibody patterns. Autoimmun Rev 2013 Aug;12(10):998-1003.
- 10. Girschick HJ, Huppertz HI, Harmsen D, Krauspe R, Müller-Hermelink HK, Papadopoulos T. Chronic recurrent multifocal osteomyelitis in children: diagnostic value of histopathology and microbial testing. Hum Pathol 1999 Jan;30(1):59-65.
- 11. Acikgoz G, Averill LW. Chronic recurrent multifocal osteomyelitis: typical patterns of bone involvement in whole-body bone scintigraphy. Nucl Med Commun 2014 Aug;35(8):797-807.
- 12. Shah A, Rosenkranz M, Thapa M. Review of spinal involvement in chronic recurrent multifocal osteomyelitis (CRMO): what radiologists need to know about CRMO and its imitators. Clin Imaging 2022 Jan;81:122-135.
- 13. Aydıngöz Ü, Yıldız AE. MRI in the diagnosis and treatment response assessment of chronic nonbacterial osteomyelitis in children and adolescents. Curr Rheumatol Rep 2022 Feb;24(2):27-39.
- 14. Koryllou A, Mejbri M, Theodoropoulou K, Hofer M, Carlomagno R. Chronic nonbacterial osteomyelitis in children. Children (Basel) 2021 Jun;8(7):551.
- 15. Alshammari A, Usmani S, Elgazzar AH, Ashkanani RA. Chronic recurrent multifocal osteomyelitis in children: a multidisciplinary approach is needed to establish a diagnosis. World J Nucl Med 2013 Sep;12(3):120-123.
- 16. Roderick MR, Shah R, Rogers V, Finn A, Ramanan AV. Chronic recurrent multifocal osteomyelitis (CRMO) - advancing the diagnosis. Pediatr Rheumatol Online J 2016 Aug;14(1):47.
- 17. Jansson A, Renner ED, Ramser J, Mayer A, Haban M, Meindl A, et al. Classification of non-bacterial osteitis: retrospective study of clinical, immunological and genetic aspects in 89 patients. Rheumatology (Oxford) 2007 Jan;46(1):154-160.
- 18. Ostrov BE, Goldsmith DP, Athreya BH. Differentiation of systemic juvenile rheumatoid arthritis from acute leukemia near the onset of disease. J Pediatr 1993 Apr;122(4):595-598.
- 19. Brix N, Rosthøj S, Herlin T, Hasle H. Arthritis as presenting manifestation of acute lymphoblastic leukaemia in children. Arch Dis Child 2015 Sep;100(9):821-825.