Neonatal respiratory distress syndrome (RDS) is a significant contributor to morbidity and mortality in newborns. Clinical manifestations often occur within minutes of birth, and include diminished breath sounds or increased respiratory effort (e.g., tachypnea, expiratory grunting, nasal flaring, accessory muscle use, cyanosis, and poor peripheral perfusion).1,2 The incidence of RDS is inversely related to gestational age, with more severe disease seen in smaller and more premature neonates.3
The primary etiology of neonatal RDS is a deficiency of surfactant due to immature lungs, causing surfactant inadequacy or inactivation. Surfactant reduces surface tension at the air-fluid interface, preventing the collapse or fluid filling of the alveoli, while its deficiency increases surface tension, exacerbating respiratory compromise.4,5
Management of neonatal RDS includes antenatal corticosteroids, surfactant therapy, and advanced respiratory support. Exogenous surfactant administration is recommended for preterm infants diagnosed with RDS when oxygen requirements exceed an FiO2 of 0.5. Surfactant replacement therapy is typically administered by trained personnel in settings equipped for intubation and resuscitation.6,7 Timing for surfactant administration is crucial: prophylactic treatment (within 30 minutes of birth), early (within 2–3 hours), or selective treatment (after appearance of clinical signs of RDS).8
Various surfactant delivery techniques exist, each with its own distinct risk-benefit profiles. The standard method —intratracheal surfactant replacement therapy via an endotracheal tube—can cause transient airway obstruction, pulmonary injury, pulmonary air leak, or airway injury.9 Another technique, intubation-surfactant administration-extubation (INSURE), involves intubation and surfactant administration, followed by extubation. This approach facilitates uniform distribution of surfactant in the lungs and is considered the easiest way, but requires correct endotracheal tube positioning and carries a risk of hemodynamic instability.10,11
A third method, less invasive surfactant administration (LISA), involves of the placement of a thin, flexible catheter in the trachea using direct laryngoscopy during spontaneous breathing, typically supported by nasal continuous positive airway pressure (NCPAP). LISA does not require intubation, is associated with a lower rate of barotrauma and death, and is currently practiced in Europe and Australia. Its disadvantages include the risk of accidental catheter removal, slow surfactant delivery, increased possibility of surfactant reflux, and the need for adequate spontaneous breathing by the baby.12,13
Similar to LISA, but used relatively less, is minimally invasive surfactant therapy (MIST), which uses a feeding tube to instill surfactant while the infant remains on non-invasive respiratory support and breathes spontaneously through a respiratory device. This method is increasingly used to minimize intubation and associated complications.14–16
Further research is required to establish MIST as a standard alternative to endotracheal intubation. This study compares INSURE and MIST techniques in premature neonates with RDS in terms of the necessity for additional surfactant doses, durations of mechanical ventilation and nasal CPAP, oxygen requirement, and associated side effects.
Methods
This randomized clinical trial included premature neonates with RDS admitted to the Namazee Neonatal Intensive Care Unit (NICU), the largest neonatal care center in Fars province, Southwestern Iran from July to December 2020. The study protocol was approved by the Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1400.509). Informed consent was obtained from parents before including neonates in this study.
Premature newborns were defined as those born before 37 weeks of gestation, and the diagnosis of RDS was made by the neonatologist based on clinical signs such as skin color, tachypnea, and retractions, as well as chest X-ray, and arterial blood gas findings. Premature newborns with pulmonary air leak syndromes, cyanotic congenital heart disease, thoracic dystrophy, suspected bacterial pneumonia, or early-onset sepsis were excluded from the study. Selected neonates’ information, including gestational age, sex, birth weight, mode of delivery (vaginal or caesarian section), Apgar score at the fifth minute and multiple pregnancies were recorded.
All newborns with signs of RDS were treated immediately with NCPAP at a pressure range of 5–8 cmH2O, and an orogastric tube was inserted to prevent abdominal distension. Cardiopulmonary monitoring and continuous monitoring of oxygen saturation were employed. If the need for fraction of inspired oxygen (FiO2) was > 40%, 200 mg/kg of surfactant (Curosurf, Chiesi Farmaceutici Group, Italy) was administered 30 minutes after initiating NCPAP to maintain SpO2 in the range of 85–92%. At our center, surfactant therapy usually requires placing an endotracheal tube using the standard method.
The selected neonates were randomly assigned to one of two groups using block randomization: (i) the INSURE group and (ii) the MIST group.
In the INSURE group, infants on NCPAP were intubated without sedation; the position of the endotracheal tube was confirmed by auscultation. A surfactant dose of 200 mg/kg was given over 1–2 minutes through the endotracheal tube, followed by mechanical ventilation with a peak inspiratory pressure of 20–22 cmH2O, positive end-expiratory pressure of 5–6 cmH2O, and respiratory rate of 30–40 breaths/min to achieve a tidal volume of 4–6 mL/kg. The endotracheal tube was withdrawn after a minimum of 30 minutes if the infant exhibited a satisfactory respiratory drive.
In the MIST group, a dose of 200 mg/kg of surfactant was administered during spontaneous breathing via a number 5F feeding tube inserted into the trachea using laryngoscopy without sedative and took 1 to 3 minutes. The insertion depth of the feeding tube was determined using the formulas: weight in kg (weight + 6). The newborn’s SpO2 and heart rate were constantly monitored using pulse oximetry during the procedure. If the catheter failed to pass through within 30 seconds, a second attempt was made to insert the catheter. After completing the procedure, the infant’s stomach was suctioned to confirm that the surfactant had entered the lung. The catheter was removed following the surfactant injection and CPAP was continued. If apnea persisted, intratracheal surfactant administration was performed via an endotracheal tube, followed by mechanical ventilation if necessary.
For infants in both INSURE and MIST groups, a second surfactant dose of 100 mg/kg could be administered 12–24 hours later, if FiO2 > 40% was still required to maintain O2 saturation within the range of 85–95%. If the newborn persisted having pH < 7.2, FiO2 > 60%, and PCO2 > 60 mmHg for longer than two hours or apnea occurred, the infant was reintubated and surfactant was administered. Skilled neonatologists performed both the INSURE and MIST techniques.
The outcomes data included the timing of surfactant treatment, the frequency of surfactant administration, duration of oxygen requirement, need for mechanical ventilation in the first 72 hours, duration of NCPAP, the incidence of bronchopulmonary dysplasia, intraventricular hemorrhage, patent ductus arteriosus, pneumothorax, pulmonary hemorrhage, disseminated intravascular coagulation, necrotizing enterocolitis, sepsis, duration of hospital stay, and mortality up to 28 days.
A total of 98 premature newborns with RDS were required for this study, considering α of 0.05 and β1 of 0.80 (d = 0.15, s1 = 0.26, s2 = 0.09), calculated using the PASS software (NCSS LLC, Kaysville, Utah, USA). The data were analyzed using IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA). Continuous variables were presented as mean ± SD or median IQR, and categorical variables were presented as frequencies and percentages. Differences between the two groups were analyzed using t-test or Mann-Whitney U test for continuous variables, and chi-square test or Fisher’s exact test for categorical variables. A p-value of < 0.05 was considered statistically significant.
Results
Of the 98 premature neonates initially recruited, 16 were excluded from the study due to asphyxia, early-onset sepsis, congenital pneumonia, and congenital heart disease. Ultimately, 82 preterm infants (34 females, 48 males) with a mean gestational age of 31.0 ± 2.3 weeks (range = 26–36 weeks) were enrolled [Figure 1].
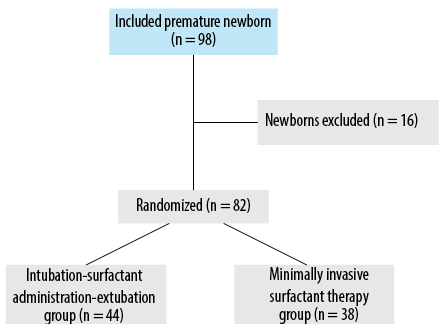 Figure 1: Flow diagram of participant selection for this study.
Figure 1: Flow diagram of participant selection for this study.
The demographic and clinical characteristics of the two study groups, INSURE and MIST, are presented in Table 1. No statistically significant differences were observed between the groups.
Table 1: Characteristics data of premature neonates treated with INSURE or MIST technique (N = 82).
|
Boys
|
25 (56.8)
|
23 (60.5)
|
0.700
|
|
Girls
|
19 (43.2)
|
15 (39.5)
|
|
Gestational weeks, mean ± SD
|
31.1 ± 2.2
|
30.8 ± 2.3
|
0.290
|
|
Birth weight in grams, mean ± SD
|
1486.0 ± 515.8
|
1460.0 ± 444.2
|
0.710
|
|
Multiple pregnancies
|
22 (50.0)
|
18 (47.4)
|
0.520
|
|
Cesarean sections
|
35 (79.6)
|
33 (86.8)
|
0.380
|
*Significant; INSURE: intubation-surfactant administration-extubation; MIST: minimally invasive surfactant therapy.
Surfactant was administered in the range of 1–180 minutes after birth in all premature newborns. Table 2 describes the key clinical complications and outcomes using the INSURE or MIST techniques.
Table 2: Comparison of neonatal complications and outcomes of INSURE or MIST techniques (N = 82).
|
Surfactant treatment time, mean ± SD, minutes
|
10.5 ± 17.0
|
42.0 ± 42.5
|
< 0.001*
|
|
Intraventricular hemorrhage
|
13
|
10
|
0.740
|
|
Bronchopulmonary dysplasia
|
4
|
6
|
0.780
|
|
Pneumothorax
|
4
|
2
|
0.800
|
|
Pulmonary hemorrhage
|
1
|
4
|
0.110
|
|
DIC
|
2
|
2
|
0.880
|
|
NEC
|
0
|
0
|
–
|
|
Sepsis
|
0
|
0
|
–
|
|
Hospital stay, mean ± SD, days
|
19.3 ± 13.4
|
21.2 ± 16.3
|
0.650
|
INSURE: intubation-surfactant administration-extubation; MIST: minimally invasive surfactant therapy; DIC: disseminated intravascular coagulation;
NEC: necrotizing enterocolitis.
Table 2 shows that the mean timing of surfactant treatment was 10.5 ± 17.0 minutes in the INSURE group and 42.0 ± 42.5 minutes in the MIST group (p < 0.001). All neonates received an initial dose of surfactant, with 17 (38.6%) neonates in the INSURE group and 18 (47.4%) in the MIST group requiring a second dose (p = 0.400). The mean duration of NCPAP requirement was 3.3 ± 3.1 days in the INSURE group and 3.2 ± 3.0 days in the MIST group (p = 0.220). The proportion of neonates requiring mechanical ventilation was 18 (40.9%) in the INSURE group and 9 (23.7%) in the MIST group, but this difference was not statistically significant (p = 0.090). Incidence of intraventricular hemorrhage, bronchopulmonary dysplasia, patent ductus arteriosus, pneumothorax, pulmonary hemorrhage, and disseminated intravascular coagulation did not differ significantly between the INSURE and MIST groups. Similarly, no significant differences were found between the two groups on the duration of hospital stay or mortality rate. None of the infants developed necrotizing enterocolitis or sepsis.
Discussion
This study investigated the effects and outcomes of administering surfactant to premature neonates with RDS via the MIST technique compared with the INSURE method. The demographic and clinical characteristics, including sex, gestational age, birth weight, multiple pregnancies, mode of delivery, and Apgar scores were comparable between the groups, indicating homogeneity.
Although the MIST approach demonstrated a lower requirement for mechanical ventilation in the first 72 hours after birth compared to INSURE, this difference did not reach statistical significance (p = 0.090), which may be attributed to the relatively small number of neonates requiring mechanical ventilation in each group. Hassan et al,17 (Iran) and Kribs et al,18 (systematic review) reported a significant reduction in the need for mechanical ventilation when the surfactant was administered via a thin endotracheal catheter compared to INSURE. Similarly, a Turkish study found a significantly lower requirement and duration of mechanical ventilation in preterm infants treated with the thin catheter technique during spontaneous breathing.16 In Iran, Choupani et al,19 found no significant difference in the need for mechanical ventilation 72 hours after birth, which was similar to our study. However, their mechanical ventilation need was lower with catheter insertion versus INSURE.
In our study, a second dose of surfactant was required for infants in INSURE (38.6%) and MIST (47.4%) groups. In a Turkish study, about 20% of infants in both groups required a second doses.16 Mosayebi et al,’s Iranian study showed about 15% of infants in the INSURE group and 7.5% in the MIST group required a second dose of surfactant.20 Interestingly, a Spanish study found that significantly more infants in the MIST group (36%) needed a second administration of surfactant compared to 6.5% in the INSURE group (p < 0.001).21 While we did not evaluate the severity of RDS in our study, it appears that newborns exhibiting more severe RDS required a second dose of surfactant more frequently.
The average duration of need for NCPAP in newborns was about three days in both groups with no significant difference. A multicenter study in Iran by Mirnia et al,22 also reported varying results across two NICUs, where CPAP duration decreased in two and increased in another, but with no overall difference between tracheal catheterization and INSURE groups.
Regarding complications, the incidence of intraventricular hemorrhage, bronchopulmonary dysplasia, patent ductus arteriosus, pneumothorax, pulmonary hemorrhage, and disseminated intravascular coagulation did not differ significantly between our INSURE and MIST groups (p > 0.050). These findings are consistent with an Indian study, which found no significant differences in the incidence of ductus arteriosus, intraventricular hemorrhage, or bronchopulmonary dysplasia between the two surfactant administration techniques.23 Similarly, Mosayebi et al. found no differences in the incidence of early and delayed complications between the MIST and INSURE methods in Iranian newborns.20
Overall, using surfactants is preferable to not using them, as found by a recent systematic review and meta-analysis of 17 randomized controlled trials involving 2408 preterm infants.24 The study found that surfactant administration via a thin catheter decreased the risk of bronchopulmonary dysplasia in survivors compared to controls.
In this study, the duration of hospital stay and mortality rates did not differ significantly between the MIST and INSURE groups. In contrast, Mirnia et al,22 reported a significantly lower mortality rate in the tracheal catheterization group compared to the INSURE group. Another Iranian study also found no significant differences in mortality and the combined outcome of chronic lung disease between MIST and INSURE.25
Our study had limitations. All patients were recruited from one referral center in Shiraz; and therefore, the results may not be generalizable. Second, our sample size was relatively small. Third, data on the administration of antenatal steroids to pregnant women was not available for comparison between the two groups. Multicenter research that eliminates the above limitations is needed to fully elucidate the advantages or disadvantages of these two surfactant administration methods.
Conclusion
Our results showed no significant differences between MIST and INSURE in terms of the need for additional surfactant doses, duration of NCPAP and mechanical ventilation, incidence of complications like intraventricular hemorrhage and bronchopulmonary dysplasia, hospital length of stay, and mortality. Both methods appear to be effective strategies for surfactant delivery in preterm infants with RDS, allowing clinicians to choose the approach that best fits their unit’s resources and expertise. Overall, this study provides valuable evidence to guide surfactant therapy in the care of premature neonates with RDS.
Disclosure
The authors declare no conflicts of interest. The results presented in this paper were part of a fellowship thesis for a neonatologist degree by Batool Abbasi and were supported by a grant from Shiraz University of Medical Sciences, Shiraz, Iran (no: 23252).
references
- 1. Martin R, Fanaroff AA, Walsh M. Fanaroff and Martin’s neonatal-perinatal medicine. 11th ed. Amsterdam: Elsevier; 2019. p. 1159-1173.
- 2. Warren JB, Anderson JM. Core concepts: respiratory distress syndrome. NeoReviews 2009;10(7):e351-e361 .
- 3. Yadav S, Lee B, Kamity R. Neonatal respiratory distress syndrome. [cited 2023 Jul 25]. In: StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560779/.
- 4. Guagliardo R, Pérez-Gil J, De Smedt S, Raemdonck K. Pulmonary surfactant and drug delivery: focusing on the role of surfactant proteins. J Control Release 2018 Dec;291:116-126.
- 5. Nkadi PO, Merritt TA, Pillers DA. An overview of pulmonary surfactant in the neonate: genetics, metabolism, and the role of surfactant in health and disease. Mol Genet Metab 2009 Jun;97(2):95-101.
- 6. Rigo V, Lefebvre C, Broux I. Surfactant instillation in spontaneously breathing preterm infants: a systematic review and meta-analysis. Eur J Pediatr 2016 Dec;175(12):1933-1942.
- 7. Walsh BK, Daigle B, DiBlasi RM, Restrepo RD; American Association for Respiratory Care. AARC clinical practice guideline. Surfactant replacement therapy: 2013. Respir Care 2013 Feb;58(2):367-375.
- 8. van Kaam AH, Niemarkt HJ, Onland W. Timing of surfactant treatment in respiratory distress syndrome. Semin Fetal Neonatal Med 2023 Dec;28(6):101495.
- 9. Ng EH, Shah V. Guidelines for surfactant replacement therapy in neonates. Paediatr Child Health 2021;26(1):35-49.
- 10. Fortas F, Loi B, Centorrino R, Regiroli G, Ben-Ammar R, Shankar-Aguilera S, et al. Enhanced INSURE (ENSURE): an updated and standardised reference for surfactant administration. Eur J Pediatr 2022 Mar;181(3):1269-1275.
- 11. De Bisschop B, Derriks F, Cools F. Early predictors for intubation-surfactant-extubation failure in preterm infants with neonatal respiratory distress syndrome: a systematic review. Neonatology 2020 Aug;117(1):33-45.
- 12. Herting E, Härtel C, Göpel W. Less invasive surfactant administration: best practices and unanswered questions. Curr Opin Pediatr 2020 Apr;32(2):228-234.
- 13. Conlon SM, Osborne A, Bodie J, Marasch J, Ryan RM, Glenn T. Introducing less-invasive surfactant administration into a level IV NICU: a quality improvement initiative. Children (Basel) 2021;8(7):580.
- 14. Shim GH. Update of minimally invasive surfactant therapy. Korean J Pediatr 2017 Sep;60(9):273-281.
- 15. Dargaville PA, Aiyappan A, De Paoli AG, Kuschel CA, Kamlin CO, Carlin JB, et al. Minimally-invasive surfactant therapy in preterm infants on continuous positive airway pressure. Arch Dis Child Fetal Neonatal Ed 2013 Mar;98(2):F122-F126.
- 16. Kanmaz HG, Erdeve O, Canpolat FE, Mutlu B, Dilmen U. Surfactant administration via thin catheter during spontaneous breathing: randomized controlled trial. Pediatrics 2013 Feb;131(2):e502-e509.
- 17. Hassan B, Gholamali M, Reza GJ, Maryam Z. Comparative study of the effect of the administration of surfactant through a thin endotracheal catheter into trachea during spontaneous breathing with intubation (Intubation-Surfactant-Extubation Method). J Clin Neonatol 2019;8(4):227-231.
- 18. Kribs A, Roberts KD, Trevisanuto D, O’Donnell C, Dargaville PA. Surfactant delivery strategies to prevent bronchopulmonary dysplasia. Semin Perinatol 2023 Oct;47(6):151813.
- 19. Choupani R, Mashayekhy G, Hmidi M, Kheiri S, Khalili Dehkordi M. A comparative study of the efficacy of surfactant administration through a thin intratracheal catheter and its administration via an endotracheal tube in neonatal respiratory distress syndrome. Iranian J Nematol 2018;9(4):33-40.
- 20. Mosayebi Z, Kadivar M, Taheri-Derakhsh N, Nariman S, Mahdi Marashi S, et al. A Randomized trial comparing surfactant administration using InSurE technique and the minimally invasive surfactant therapy in preterm infants (28 to 34 Weeks of Gestation) with respiratory distress syndrome. J Compr Ped 2017;8(4):e60724.
- 21. Aguar M, Cernada M, Brugada M, Gimeno A, Gutierrez A, Vento M. Minimally invasive surfactant therapy with a gastric tube is as effective as the intubation, surfactant, and extubation technique in preterm babies. Acta Paediatr 2014 Jun;103(6):e229-e233.
- 22. Mirnia K, Heidarzadeh M, Hoseini MB, Sadeghnia A, Akrami F, Balila M, et al. Surfactant administration via thin catheter during spontaneous breathing: randomized controlled trial in Alzahra hospital. Iranian J Nematol 2013;4(2):5-9.
- 23. Gupta BK, Saha AK, Mukherjee S, Saha B. Minimally invasive surfactant therapy versus InSurE in preterm neonates of 28 to 34 weeks with respiratory distress syndrome on non-invasive positive pressure ventilation-a randomized controlled trial. Eur J Pediatr 2020 Aug;179(8):1287-1293.
- 24. Yeung TY, Zhou Q, Kanmaz Kutman HG, Pandita A, Philippopoulos E, Jasani B. Surfactant delivery via thin catheter in preterm infants: a systematic review and meta-analysis. PLoS One 2023: 26;18(4):e0284792.
- 25. Mohammadizadeh M, Ardestani AG, Sadeghnia AR. Early administration of surfactant via a thin intratracheal catheter in preterm infants with respiratory distress syndrome: feasibility and outcome. J Res Pharm Pract 2015;4(1):31-36.