A 73-year-old lady presented to the outpatient department with a large midline neck mass [Figure 1], which was present for the past 40 years. She complained of a sudden increase in the size of the mass and weight loss of about 10 kg over the last four months. She also reported a dry cough, progressive dysphagia for the past 10 days, and shortness of breath for three days. There was hoarseness of voice but no stridor. There was no history of fever or sore throat. The neck lump was a hard, nodular mass extending from the lower border of the thyroid cartilage to the sternal notch, with encasement of unilateral carotid vessels and skin invasion, as suggested by dermal edema. The trachea and the bilateral cervical lymph nodes could not be appreciated due to the large size of the goiter and induration. There were no signs of discharge, inflammation, or visible pulsation over the mass. Informed consent was obtained from the patient.
 Figure 1: The patient’s neck shows an apparent mass.
Figure 1: The patient’s neck shows an apparent mass.
Ultrasonography of the neck revealed a large, heterogeneous, predominantly hypoechoic lesion replacing the entire thyroid gland, with a few small cystic areas and some calcifications (TIRADS-5) [Figure 2]. A chest X-ray showed multiple patchy opacities throughout both lung fields, giving a cannonball appearance and a right-sided tracheal deviation and bilateral mild pleural effusion [Figure 3]. A neck computed tomography (CT) showed a large hypo-enhancing space-occupying lesion from the thyroid gland, infiltrating bilateral sternocleidomastoid muscles associated with enlarged level VI lymph nodes. A contrast-enhanced CT (CECT) of the thorax suggested multiple randomly distributed nodules in both lung fields and multiple enlarged mediastinal lymph nodes, with mild bilateral pleural effusion.
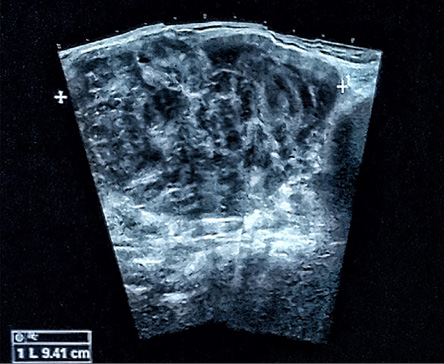 Figure 2: Ultrasound image showing a large, heterogeneous, predominantly hypoechoic lesion replacing the entire thyroid gland, with a few small cystic areas.
Figure 2: Ultrasound image showing a large, heterogeneous, predominantly hypoechoic lesion replacing the entire thyroid gland, with a few small cystic areas.
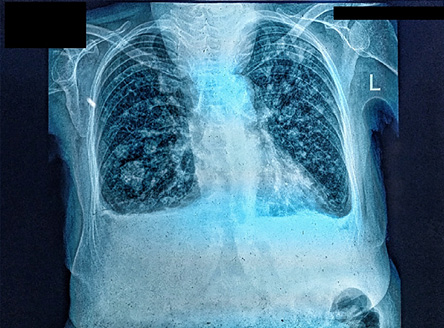 Figure 3: Chest X-ray showing multiple patchy opacities throughout both lung fields.
Figure 3: Chest X-ray showing multiple patchy opacities throughout both lung fields.
Fine-needle aspiration cytology from the neck mass showed high cellularity with focal clusters of markedly atypical cells and multiple giant cells. Mitotic figures were prominent. The patient did not consent to a core biopsy procedure.
Questions
- What is the diagnosis?
- What stage is it?
- What are the immediate palliative measures that can be taken?
- What are the targeted therapies of benefit?
Answers
- Anaplastic thyroid carcinoma (ATC) with metastatic lung disease.
- Stage IV C.
- Isthmusectomy with tracheostomy.
- The targeted therapies of benefit are as follows:
- Dabrafenib/trametinib (for BRAF V600E mutation-positive).
- Larotrectinib or entrectinib (for NTRK gene fusion-positive).
- Pralsetinib or selpercatinib (for RET gene fusion-positive).
- Other recommended chemotherapy regimens include paclitaxel and doxorubicin-based therapies.
Discussion
ATC, a highly aggressive tumor with nearly 100% mortality, is mainly diagnosed in females around the age of 70. Its incidence has declined due to improved thyroid cancer management and increased iodine intake. ACT emerges from the dedifferentiation of other thyroid tumors, often linked to p53 protein loss. Clinical symptoms include rapid growth of a neck mass, dyspnea, dysphagia, and distant metastases, mainly to the lungs and pleura.
ATC tumors exhibit diverse morphologies, including biphasic spindle and giant cell features. Diagnosis is made through core or surgical biopsy. Laryngeal examination and imaging (ultrasound, CT scans) assess tumor extension and invasion. Positron emission tomography/CT or magnetic resonance imaging helps with staging. Testing for actionable mutations (BRAF, NTRK) is recommended for targeted therapy.1
The prognosis of ATC is poor, with a median survival of about five months, often due to airway obstruction or complications. Age, metastases, and symptoms influence the prognosis. Recent studies suggest that targeted therapies and surgery following neoadjuvant BRAF-targeted therapy may improve survival. Conventional therapies, including radioactive iodine therapy, are usually ineffective against ATC. As a result, palliative and supportive care should be initiated early to improve survivability. 2,3
Treatment modalities by stage
stage Ia and Ib
resectable
- Neoadjuvant dabrafenib/trametinib for BRAF V600E-mutated disease.
- Total thyroidectomy with lymph node dissection, followed by adjuvant external beam radiation therapy (EBRT)with radiosensitising chemotherapy for R0/R1 resection and EBRT with chemotherapy for R2 resection.
unresectable or borderline resectable
- Molecularly targeted neoadjuvant therapy or EBRT with chemotherapy.
- Surgery may be considered a post-neoadjuvant chemotherapy response.
Stage IVC
Aggressive therapy
- Total thyroidectomy with lymph node dissection if resectable (R0/R1).
- Tracheostomy and steroids if indicated.
Local radiation therapy and chemotherapy.
Pallitative care
- Palliative local radiotherapy.
- Local excision or radiotherapy.
- Tracheostomy and supportive management.
After initial therapy, contrast CT/magnetic resonance imaging scans of the chest, neck, abdomen, pelvis, and brain are crucial for disease monitoring. An fluorodeoxyglucose-positron emission tomography scan may follow three to six months after initial therapy. If there is no further evidence of disease, continued monitoring and consideration of palliative local radiotherapy, disease control measures, second-line chemotherapy, or systemic therapy is advised.1
Preferred treatment options include dabrafenib, entrectinib, pralsetinib, or selpercatinib, with alternative regimens including paclitaxel, doxorubicin, and carboplatin.
Disclosure
The authors declare no conflicts of interest.
references
- 1. National Comprehensive Cancer Network. Thyroid carcinoma. 2024 [cited 2024 September 11]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/thyroid.pdf.
- 2. Park JW, Choi SH, Yoon HI, Lee J, Kim TH, Kim JW, et al. Treatment outcomes of radiotherapy for anaplastic thyroid cancer. Radiat Oncol J 2018 Jun;36(2):103-113.
- 3. Siironen P, Hagström J, Mäenpää HO, Louhimo J, Heikkilä A, Heiskanen I, et al. Anaplastic and poorly differentiated thyroid carcinoma: therapeutic strategies and treatment outcome of 52 consecutive patients. Oncology 2010;79(5-6):400-408.