A21-year-old primigravida at 27 weeks of pregnancy presented with complaints of spotting per vaginum and a vulval mass. She had noticed the growth in the perineal region over the past two months increasing in size. The patient reported good fetal movements and had no significant comorbidities. General and systemic examinations were unremarkable. On abdominal examination, the uterus height corresponded to the period of gestation, and fetal parts were palpable. Local examination of the vulva revealed a large cauliflower-like lesion containing multiple raised, skin-colored, fleshy papules measuring a few millimeters [Figure 1]. The lesion involved both labia majora, the lower part of the anterior vaginal wall near the urethral orifice, and the vaginal orifice around the fourchette. The lesion exhibited superficial keratinization and some bleeding points. Secondary infection was noted with the formation of pus points. No other vaginal or cervical lesions were obeserve on per speculum examination.
 Figure 1: Vulval lesion on admission.
Figure 1: Vulval lesion on admission.
Question
What is the diagnosis?
- Condyloma acuminata.
- Vestibular papillomatosis.
- Molluscum contagiosum.
- Angiokeratoma.
- Seborrheic keratosis.
- Giant condylomatosis or Buschke-Lowenstein tumor.
Answer
- Condyloma acuminata.
Condyloma acuminata is predominantly caused by human papillomavirus (HPV) types 6 and 11. It is a common sexually transmitted infection, with the highest incidence in women aged 20–24 years and men aged 25–29 years.1 Risk factors include multiple sexual partners, early sexual debut, tobacco use, coexisting sexually transmitted diseases, immunocompromised status, lack of condom use, and low educational level.2,3 Clinically, the painless warty growth is often accompanied by discomfort, itching, foul-smelling discharge, and dyspareunia. In pregnancy, condyloma acuminata may exhibit larger and more numerous lesions, occasionally affecting the mode of delivery.
Discussion
Vertical transmission of HPV during childbirth can occur through direct contact with maternal infected cells, whether during vaginal delivery or following early rupture of membranes in a cesarean section.4
In-utero transmission may happen through an ascending infection from the mother’s genital tract or via HPV-infected semen after intercourse. Transplacental transmission is supported by the presence of HPV DNA in amniotic fluid. It has been detected in various tissues, including the endometrium, ovaries, placental cells, cord blood, and breast milk.
Treatment options for HPV during pregnancy encompass topical imiquimod, cryotherapy, diathermy electrocoagulation, CO2 laser therapy, and surgical excision.5 Reports on using trichloroacetic acid as a single agent in pregnant women are scarce. Topical imiquimod therapy spans 3–10 weeks, with local erythema being the most common side effect. Cryotherapy, requiring multiple sessions, may result in scars and pigment changes, posing a higher relapse risk for larger lesions. Diathermy electrocoagulation is effective for smaller warts but may cause permanent scarring in larger lesions. CO2 laser therapy, with a higher success rate particularly in refractory cases and immunocompromised patients, carries a heightened risk of infection dissemination. The duration between treatment and recurrence is the lowest following CO2 laser therapy and highest following imiquimod and cryotherapy.
In this case, surgical excision with a scalpel was chosen because of the larger lesion. This approach minimizes scarring and preserves healthy tissue, resulting in favorable outcomes [Figure 2a and b]. HPV DNA testing was not done for this patient as it does not add to the management. Histopathology of the lesion revealed markedly acanthotic papillomatosis, stratified squamous epithelium with hyperkeratosis. The papillae showed a thin fibrovascular core with lining stratified squamous epithelium with koilocytic changes in the upper third of the epithelium [Figure 2c and d]. The patient underwent at 37 weeks a cesarean section for fetal distress delivering a female baby weighing 2.5 kg. The baby was well, and the patient was discharged on the fourth postoperative day. There were no genital lesions during this admission.
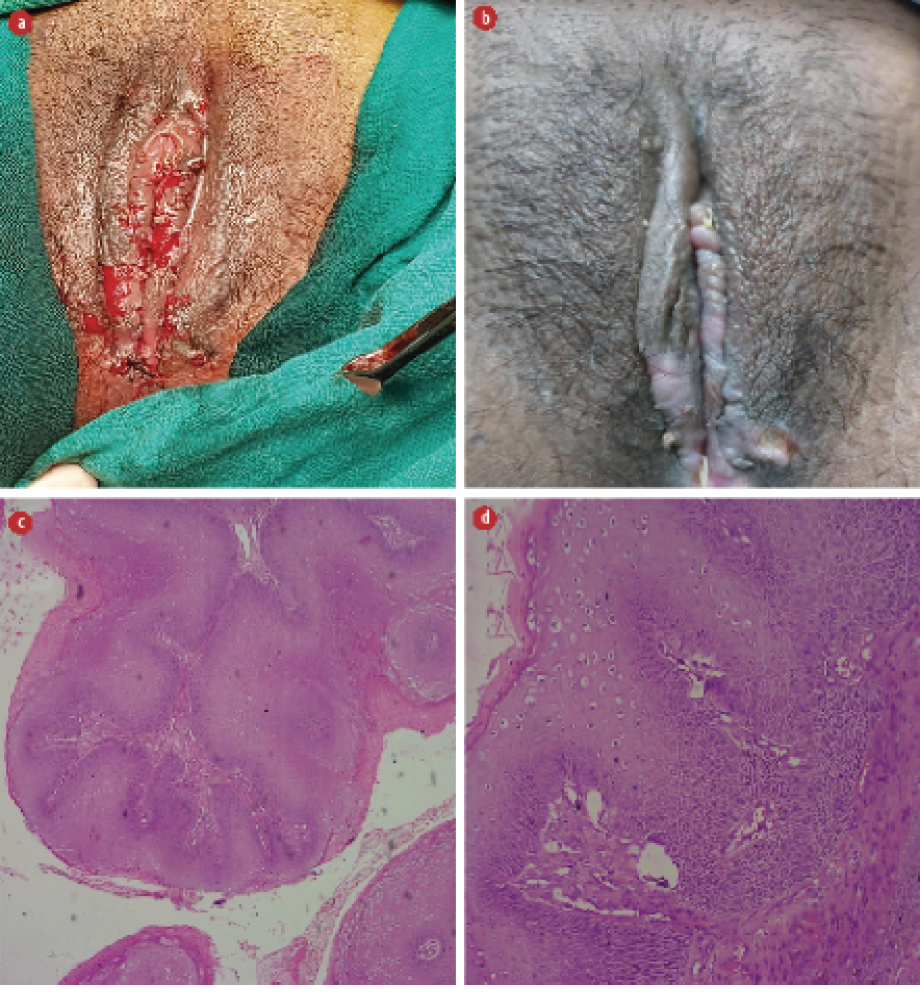 Figure 2: (a) Local examination of vulva after excision of the lesion, (b) local examination of the vulva two weeks after excision. (c) Hyperplastic papillary exophytic squamous epithelium with fibrovascular core, hematoxylin and eosin staining, magnification = 10 ×, and (d) koilocytosis confined to the upper third of squamous epithelium, hematoxylin and eosin staining, magnification = 40 ×.
Figure 2: (a) Local examination of vulva after excision of the lesion, (b) local examination of the vulva two weeks after excision. (c) Hyperplastic papillary exophytic squamous epithelium with fibrovascular core, hematoxylin and eosin staining, magnification = 10 ×, and (d) koilocytosis confined to the upper third of squamous epithelium, hematoxylin and eosin staining, magnification = 40 ×.
The diagnosis of condyloma acuminata was based on clinical examination and histopathological findings. It emphasizes the importance of individualized treatment approaches, particularly during pregnancy. HPV vaccination remains the most effective preventive measure, and treatment should be tailored to the patient’s unique circumstances. Vertical mother-to-child transmission of HPV can occur in children born via cesarean section.5 Cesarean section is indicated only when lesions obstruct the birth canal or pose a risk of excessive bleeding.
Condyloma acuminata presenting as a large vulval lesion during pregnancy poses a challenge for diagnosis and management. Other potential differential diagnoses should always be considered. The advantages and disadvantages of various treatment modalities should be weighed and the patient should be managed accordingly.
Disclosure
The authors declared no conflicts of interest. Written consent was obtained from the patient.
references
- 1. Patel H, Wagner M, Singhal P, Kothari S. Systematic review of the incidence and prevalence of genital warts. BMC Infect Dis Jan 25;13(1):39.
- 2. Goldstone S, Palefsky JM, Giuliano AR, Moreira ED Jr, Aranda C, Jessen H, et al. Prevalence of and risk factors for human papillomavirus (HPV) infection among HIV-seronegative men who have sex with men. J Infect Dis 2011 Jan;203(1):66-74.
- 3. Veldhuijzen NJ, Snijders PJ, Reiss P, Meijer CJ, van de Wijgert JH. Factors affecting transmission of mucosal human papillomavirus. Lancet Infect Dis 2010 Dec;10(12):862-874.
- 4. Trottier H, Mayrand MH, Coutlée F, Monnier P, Laporte L, Niyibizi J, et al. Human papillomavirus (HPV) perinatal transmission and risk of HPV persistence among children: design, methods and preliminary results of the HERITAGE study. Papillomavirus Res 2016 Dec;2:145-152.
- 5. Sugai S, Nishijima K, Enomoto T. Management of condyloma acuminata in pregnancy: a review. Sex Transm Dis 2021 Jun 1;48(6):403-409.