Globally, healthcare providers’ (HCP) preparedness, readiness, and response to COVID-19 align closely with the World Health Organization recommendations, which encompass technical guidance, training courses, coordination protocols, and communication agreements.1 HCP's knowledge, skills, and attitudes have been consistently emphasized as pivotal in managing COVID-19 patients, with a particular focus on the healthcare system and organizational measures.2
The readiness of HCPs has emerged as a prominent concern worldwide. Many HCPs routinely find themselves on-call, working extended hours, and striving to adhere to established protocols while maintaining their physical and mental well-being.3 This challenge is compounded by the surge in COVID-19 cases during the outbreak, necessitating strict compliance with preventive measures and the creation of safe conditions for healthcare staff and patients.4 Hence, the robust preparedness of healthcare institutions for infectious disease threats is imperative.
Recent experiences, such as the Ebola outbreaks in Nigeria between 2014 and 2016 and the 2020 outbreak, revealed that over 90% of HCPs believed that their healthcare facilities were inadequately equipped to respond to disease outbreaks.5 Similarly, during the MERS-CoV outbreak in Saudi Arabia, most HCPs, particularly nurses, expressed grave concerns about the risk of viral transmission at work, even when adhering to standard precautions.6 It has been recommended that hospital management incorporate outbreak planning strategies to bolster staff performance and their approach to treating infectious diseases.
Comparative studies between SARS-CoV, MERS-CoV, and COVID-19 underscore the critical importance of early identification of super-spreaders to minimize transmission, among patients and HCPs. Immediate implementation of comprehensive precautions and measures, both clinically and in public healthcare, is vital.7,8
There is a noticeable dearth of studies in the literature addressing the preparedness level of our HCP in managing and treating patients during pandemics, specifically focusing on the impact of training programs and continuous professional training post-graduation.
In Oman, most tertiary hospitals and healthcare institutions are concentrated in Muscat. Since the onset of the COVID-19 pandemic, the Royal Hospital in Muscat has developed a preparedness plan for HCPs and patients. This plan encompasses checklists, training sessions, and protocol guidance. However, the study seeks to ascertain the impact of this training and whether it adequately addresses the anticipated challenges faced by HCPs. Thus, the primary objective of our study was to examine HCPs across all categories’ perceptions of their preparedness in managing and treating COVID-19 patients. We aimed to evaluate this preparedness concerning their foundational education and the effectiveness of continuous training programs post-graduation and during their professional tenure.
Methods
The study was carried out at the Royal Hospital using a mixed-method design over a period of six weeks starting in August 2020.
The study aimed to reach all HCPs in the hospital across various categories within the specified timeframe. In the pilot phase, the questionnaire was electronically distributed to 20 HCPs. The research team utilized participant feedback to refine the questionnaire before its final distribution.
A questionnaire was designed according to the US Centers for Disease Control and Prevention to mirror the requirements for pandemic influenza preparedness training used for COVID-19 training.9 Our questionnaire was reviewed, and two independent experts confirmed the content validity.
The questionnaire was divided into four parts. Part I contained questions related to HCPs demographics: age, gender, and profession. Part II was divided into two sections. The first section focused on issues related to hospital plans and protocols, and the second section focused on the individual HCP receipt of knowledge related either by self-learning or formal training. Part III collected information related to positive effects that increased HCPs confidence in managing COVID-19 cases. These questions were coded on a Likert scale (not at all, not really, undecided, somewhat, and very much).
For the qualitative part, part IV had two open-ended questions asking individuals to identify challenges faced during the COVID-19 pandemic and training needs that were not covered during COVID-19. Data were collected through Google forms and distributed via emails and WhatsApp groups, with outreach efforts coordinated by head directors, department coordinators, and the human resources department.
Data were transferred to Excel and subsequently imported to SPSS Statistics (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.) for data analysis.
Regarding the knowledge and awareness section, each variable received a specific score, and we computed respondent percentages based on the total scores. We then examined group differences concerning scores exceeding 75% in awareness and knowledge.
The research aimed for 385 participants based on a targeted sample size calculation with 0.5% population, an effect size of 1, 5% absolute precision, and a 95% level of significance. To offer a descriptive overview, we calculated frequencies and percentages. Chi-square tests were used to assess differences between groups. A p-value < 0.05 was considered statistically significant. We employed a qualitative thematic analysis approach for the final two open-ended questions. Initially, we transcribed the data and conducted a manual analysis using qualitative manifest thematic analysis techniques. This process involved multiple readings of the transcriptions by the second and fourth authors to develop a comprehensive understanding of the dataset. The identified codes were subsequently shared with the research team for further discussion and validation.
The study received ethical approval from the Royal Hospital’s Ethical Committee (NO. SRC#42/2020) and adheres to the Declaration of Helsinki.
Results
The questionnaire was distributed to all 3000 HCPs within the hospital; 241 HCPs responded, giving a response rate of 62.6%, as calculated based on the specified sample size. Most respondents were female, comprising 84.6% (n = 204), and nearly half fell within the 31–40 years age group (n = 120; 49.8%). In terms of profession, nurses constituted two-thirds of the sample (n = 163; 67.6%), followed by doctors (n = 63; 26.1%), and others (n = 15; 6.2%).
Significant differences were observed in awareness [Table 1] and knowledge levels [Table 2] among different genders (p = 0.018 and p = 0.001) and professions (p < 0.001 and p < 0.001), but not among age groups. Female respondents and nurses reported higher average awareness and knowledge scores [Figure 1]. When comparing female doctors to female nurses, female nurses demonstrated superior awareness (p < 0.001), while female doctors exhibited better knowledge (p < 0.001). Furthermore, significant differences were noted when comparing different age groups among nurses, with higher awareness and knowledge scores associated with increasing age.
Table 1: Awareness of the hospital’s plan and protocol (N= 241).
|
The hospital's plan for protecting patients, HCPs, and visitors from COVID-19, which addresses all required elements that must be followed.
|
214
(88.8)
|
25
10.4
|
2
(0.8)
|
0.640
|
0.011
|
0.001
|
|
The hospital’s protocol for identifying, monitoring, and reporting COVID-19 among hospitalized patients, volunteers, and HCPs (e.g., weekly or daily number of patients and staff with COVID-19).
|
184
(76.3)
|
48
(19.9)
|
9
(3.7)
|
0.290
|
0.008
|
< 0.001
|
|
The hospital’s protocol for evaluating and diagnosing hospitalized patients, volunteers, and HCPs with COVID-19 symptoms.
|
198
(82.2)
|
35
(14.5)
|
8
(3.3)
|
0.767
|
0.020
|
0.001
|
|
The hospital’s management protocol for persons with possible COVID-19 (criteria for detecting a possible case, the diagnostic work-up to be performed, infection control measures to be implemented, supportive medical treatment, and directions for notifying).
|
209
(86.7)
|
26
(10.8)
|
6
(2.5)
|
0.952
|
0.008
|
0.001
|
|
The hospital’s system for monitoring and internally reviewing healthcare-associated transmission of COVID-19 among patients and HCPs in the facility.
|
179
(74.3)
|
53
(22.0)
|
9
(3.7)
|
0.577
|
0.006
|
< 0.001
|
HCP: healthcare provider..
Table 2: Knowledge precaution and management of COVID-19 cases (N= 241).
|
Know basic microbiology and how infections can be transmitted in healthcare settings.
|
228
(94.6)
|
7
(2.9)
|
6
(2.5)
|
0.135
|
0.661
|
0.038
|
|
Know routine practices and transmission-based precautions.
|
233
(96.7)
|
7
(2.9)
|
1
(0.4)
|
0.397
|
0.178
|
0.158
|
|
Know the selection of appropriate PPE.
|
237
(98.3)
|
2
(0.8)
|
2
(0.8)
|
0.420
|
0.011
|
0.027
|
|
Know how to appropriately wear PPE.
|
233
(96.7)
|
6
(2.5)
|
2
(0.8)
|
0.311
|
0.272
|
< 0.001
|
|
Know how to appropriately manage sharps, blood, and body fluids.
|
235
(97.5)
|
5
(2.1)
|
1
(0.4)
|
0.566
|
0.814
|
< 0.001
|
|
Recognize appropriate first aid activities for different exposures such as blood and body fluids.
|
219
(90.9)
|
18
(7.5)
|
4
(1.7)
|
0.082
|
0.380
|
< 0.001
|
|
Recognize that reusable equipment that has been in direct contact with a patient should be cleaned and reprocessed before use in the care of another patient.
|
222
(92.1)
|
16
(6.6)
|
4
(1.7)
|
0.895
|
0.435
|
0.003
|
|
Appreciate the differences between clean, disinfected (low, medium, and high-level), and sterile items.
|
214
(88.8)
|
25
(10.4)
|
2
(0.8)
|
0.102
|
0.169
|
0.041
|
|
Know the difference between regular and biohazard wastes.
|
222
(92.1)
|
18
(7.5)
|
1
(0.4)
|
0.208
|
0.120
|
< 0.001
|
|
Know the infectious conditions that require absence from work or work restrictions.
|
207
(85.9)
|
31
(12.9)
|
3
(1.2)
|
0.101
|
0.072
|
< 0.001
|
|
Know the signs and symptoms of COVID-19.
|
239
(99.2)
|
2
(0.8)
|
0
(0.0)
|
0.177
|
0.716
|
0.001
|
|
Know how to monitor patients with signs and symptoms of COVID-19.
|
217
(90.0)
|
18
(7.5)
|
6
(2.5)
|
0.330
|
0.137
|
0.003
|
|
Know how to keep patients, visitors, and healthcare providers safe by using correct infection control practices including proper hand hygiene, selection, and use of PPE with a required demonstration of competency.
|
229
(95.0)
|
8
(3.3)
|
4
(1.7)
|
0.340
|
0.007
|
< 0.001
|
|
Know proper assessment and recognition of critically ill patients.
|
201
(83.4)
|
26
(10.8)
|
14
(5.8)
|
0.069
|
0.106
|
0.071
|
PPE: personal protective equipment.
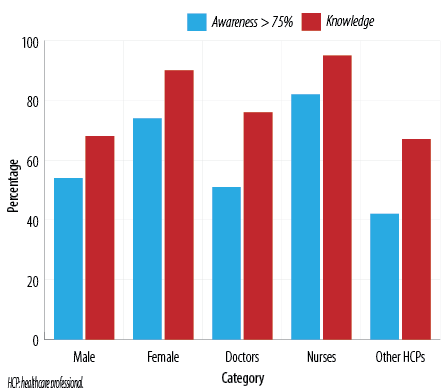 Figure 1: Average percentage of total awareness and knowledge on preparedness plans among gender and profession groups.
Figure 1: Average percentage of total awareness and knowledge on preparedness plans among gender and profession groups.
Approximately, a quarter of HCPs (n = 59; 24.5%) were unaware of the hospital’s plans to track COVID-19-related staff absences, and a similar proportion (n = 53; 22.0%) were unaware of the hospital’s system for monitoring COVID-19 transmission and reporting the numbers of COVID-19 patients and staff [Table 1]. Notably, 76.5% of surveyed HCPs recognized the importance of tracking COVID-19-related staff absences, while 69.7% were aware of the hospital’s system for monitoring COVID-19 transmission and reporting COVID-19 statistics.
Most HCPs reported good knowledge except for a few areas where non-doctor and non-nurse HCPs acknowledged gaps in their knowledge [Table 2]. A notable knowledge gap was identified in understanding the management of patients on ventilators, affecting 26.6% (n = 64), with higher incidence among younger HCPs (p < 0.015). Additionally, younger age group HCPs reported more knowledge gaps in assessing and recognizing critically ill patients, although this difference was not statistically significant (p < 0.069).
Physicians, particularly males, reported more knowledge gaps compared to nurses regarding the selection and proper use of personal protective equipment (PPE), appropriate management of sharps, blood, and body fluids, recognition of first aid protocols for various exposures, awareness of the need to clean and reprocess reusable equipment, and understanding the differences between clean, disinfected (low, medium, and high-level), and sterile items.
The findings suggested that HCP’s confidence and effectiveness in managing COVID-19 cases are influenced by various factors [Table 3]. Positive perceptions of their knowledge and skills in critical care and infectious disease management correlate with higher confidence levels. However, fear of infection and stress in handling COVID-19 patients are prevalent, potentially impacting performance. Trust in team expertise and hospital readiness positively affect confidence, while confidence in national containment plans varies. Overall, addressing stressors and bolstering confidence through training, support systems, and clear communication may enhance HCPs’ ability to manage COVID-19 effectively.
Table 3: Factors affecting confidence levels of management of COVID-19 cases (N= 241).
|
My knowledge of managing critically ill patients.
|
134
(55.6)
|
76
(31.5)
|
31
(12.9)
|
0.502
|
0.219
|
0.001
|
|
My skills to manage critically ill patients.
|
129
(53.5)
|
80
(33.2)
|
32
(13.3)
|
0.892
|
0.563
|
0.001
|
|
My knowledge of managing highly contagious diseases.
|
135
(56.0)
|
75
(31.1)
|
31
(12.9)
|
0.539
|
0.517
|
0.102
|
|
My experience of managing highly contagious diseases.
|
120
(49.8)
|
84
(34.9)
|
37
(15.4)
|
0.072
|
0.010
|
0.030
|
|
My fear of catching/transmitting the infection.
|
103
(42.7)
|
112
(46.5)
|
26
(10.8)
|
0.495
|
0.283
|
< 0.001
|
|
My stress in handling COVID-19 patients.
|
93
(38.6)
|
114
(47.3)
|
34
(14.1)
|
0.514
|
0.256
|
< 0.001
|
|
My trust towards the experts and senior healthcare providers in my team.
|
132
(54.8)
|
71
(29.5)
|
38
(15.8)
|
0.083
|
0.155
|
0.001
|
|
My confidence in the level of readiness of the hospital to handle the COVID-19 outbreak.
|
136
(56.4)
|
65
(27.0)
|
40
(16.6)
|
0.337
|
0.039
|
0.329
|
After analyzing the data using thematic coding for the two open-ended questions, the data under the first question was analyzed into: 1) fear/insecurity, 2) PPE, 3) patients/relatives, and 4) workplace. The data under the second question was analyzed into:
1) critical care and resuscitation courses, 2) COVID-19 infection control courses, and 3) psychological support.
HCP concerns
- fear
HCPs working in COVID-19 wards, dealing with or exposed to confirmed or suspected cases expressed fear of getting infected with COVID-19. Among this group, some feared transmitting the disease to their family members, especially those who lived with elderly people or children.
HCP expressed a sense of insecurity because of insufficient updates about the status of the pandemic, false news from social media, and poor emotional and psychological preparedness.
- PPE
PPE was one of the major challenges that was repeatedly mentioned by HCPs. HCPs think that since the demand for PPE has globally increased, there was insufficient supply and what was available was low quality. Even when PPE was available, HCP used one mask during each shift. Some of the HCPs mentioned that the patient’s relatives were not strict in wearing facemasks, which puts the HCP at additional risk of infection.
- patients/relatives
Few respondents claimed that patients attending clinics or emergency rooms were not screened for COVID-19, which was a concern since despite not exhibiting any signs and symptoms. They can carry and spread the virus.
In addition, HCPs encountered difficulties with uncooperative patients either while taking the history of traveling and their symptoms or by maintaining social distance.
- workplace
The need to reallocate HCPs into demanding clinical areas was very challenging. Some HCPs stated that they had been reassigned to a new ward without any experience or training.
The HCP training needs
- critical care and resuscitation courses
In this theme, critical care and resuscitation courses were perceived as the main needs. Most HCP mentioned that they need to attend basic and advanced resuscitation courses such as basic life support and advanced cardiopulmonary life support. In addition, HCPs mentioned that the management of critically ill patient's course is essential, such as managing critically ill patients in an intensive care unit setting and dealing with ventilators.
- covid-19 infection control course
COVID-19 infection control course was mentioned a few times by HCPs as a required course. According to HCPs, they need to be trained on how to approach, isolate, transfer, and provide death care for COVID-19 patients.
PPE training will assist HCPs on how to wear and dispose of PPE, handle and sterilize equipment used for COVID-19 patients, clean and disinfect methods, waste management, and hand washing.
- psychological support
Since the beginning of the pandemic, HCPs started to feel distressed or anxious in dealing with depressed COVID-19 patients, therefore, The stress management course and psychological support course were among the required courses.
Discussion
Since the outset of the COVID-19 pandemic, HCPs have faced many challenges and exhaustion. As infection rates surged across different regions, hospitals and healthcare institutions strained beyond capacity, struggling to accommodate admissions while maintaining stringent safety protocols.10
A prevalent concern among HCPs was fear of transmitting the virus to their family members and loved ones at home, more than their fear of contracting the disease themselves. This is similar to findings during the MERS-CoV outbreak in Saudi Arabia11 and COVID-19 experiences worldwide12 including Nepal,13 the Middle East and North Africa regions, and Southeast Asia.14 A study conducted in the Netherlands further validates these observations, illustrating widespread anxiety among HCPs fueled by both traditional and social media sources.15
The present study unveiled that most participants possessed a reasonable awareness of their hospital’s strategies for protecting patients, HCPs, and visitors from COVID-19. They were also well-versed in the protocols established by the hospital for identifying, monitoring, and reporting COVID-19 cases among hospitalized patients, volunteers, and staff, including the weekly monitoring of patient and staff COVID-19 statistics. However, despite their knowledge and awareness of the pandemic and the established protocols, HCPs reported low confidence levels, particularly concerning the management of critically ill and highly contagious patients, and their general preparedness for pandemics.
Our research revealed variations in levels of awareness and knowledge across professions (p < 0.001 and p < 0.001) and between genders (p = 0.018 and p = 0.001). In a recently published study by Schaffler-Schaden,16 female HPCs displayed significantly lower self-confidence and higher perceived risk related to COVID-19 than their male counterparts. Low self-confidence in treating COVID-19 patients was common among female HPCs across participating countries. These findings underscore the importance of realistic self-assessment for HPCs to ensure optimal medical care. The observed gender differences in self-confidence and risk perception align with previous studies, suggesting a consistent pattern across medical professionals.
A study showed that despite their first feelings of anxiety and uncertainty, nurses showed readiness and flexibility in carrying out their frontline tasks. Their confidence was originally hampered by their lack of training and understanding. Similar experiences have been noted in previous qualitative research of Almomani among nurses’ experiences, skills, and desire to care for COVID-19 patients.17
A survey was undertaken to investigate the knowledge, attitudes, perceptions, experiences, and preventative measures of primary healthcare centers in relation to the COVID-19 pandemic and immunizations.18 Sixty-two countries participated in the survery with comparable representation from both high-, low-, and middle-income countries. Overall, physicians worldwide demonstrated an adequate understanding of COVID-19 and its vaccinations. Nevertheless, there was still an opportunity for improvement in guaranteeing compliance with preventative measures.
Participants exhibited heightened fear and stress related to disease transmission within the hospital, primarily due to direct contact with COVID-19 patients. Additionally, they expressed limited confidence and trust in their senior colleagues within their teams, which adversely impacts their performance.
While HCPs may know where to access guidance on COVID-19, their confidence in managing highly contagious patients is hampered by a lack of practical experience. Elevated stress levels and anxiety further hinder their ability to provide care for these patients, contributing to psychological distress and burnout.
Prescott et al,19 underscored the critical importance of knowledge and skills training for HCPs to effectively manage pandemics. In their study, the majority of participants had over a decade of experience, implying that prior experience during disease outbreaks over the past two decades had provided them with valuable knowledge on how to manage novel infectious diseases.
In contrast to some other countries, Oman had not encountered a pandemic since the 2009 H1N1 outbreak, which was not comparable in scale to SARS-CoV-2. Consequently, HCPs in Oman are less prepared to manage the continuous influx of patients while ensuring the safety of themselves and their loved ones, both at work and at home.
The principal recommendation is the implementation of effective and efficient training for HCPs to comprehensively address pandemics. This training should encompass the management of critically ill patients in intensive care unit settings, the handling of highly contagious cases, and an understanding of the nuances of caring for patients on ventilators. Given the extended hours HCPs devote to treating COVID-19 patients, they must receive training on infection control measures, correct usage of PPE and N95 masks, adherence to hand hygiene protocols, and other essential safety measures necessary for managing SARS-CoV-2. Extensive evidence supports the importance of evidence-based education and training for HCPs in enhancing their skills, confidence, preparedness, and emotional well-being during pandemics.5
Moreover, it is imperative to ensure that staff are well-informed about where to access key guidance and support, as this is crucial for reducing anxiety and optimizing their performance.10 Valuable insights gleaned from the 2014 Ebola outbreak underscore the necessity of prioritizing interventions aimed at safeguarding the health and mental well-being of frontline HCPs in the context of the COVID-19 response.
Finally, there is a pressing need to increase the availability of HCPs to alleviate the burden of care. This entails shifting staff from other disciplines to medical wards, expediting the inclusion of medical students and resident doctors in the workforce, canceling leave for healthcare workers, and calling upon retired HCPs to contribute their expertise.
Policymakers, public health authorities, medical educators, and trainers must recognize the urgency of adapting training methodologies for physicians, nurses, and all allied health professionals involved in pandemic responses. This includes revising training methods in medical schools, nursing colleges, and related institutions. While knowledge and awareness are undoubtedly critical for HCP, the absence of practical hands-on training and exposure can result in diminished performance, productivity, and emotional well-being. Practical, hands-on training using real-life scenarios, rather than simulations, has demonstrated significant benefits in enhancing the confidence levels of HCPs, both in routine clinical practice and during disease outbreaks.
Another vital facet of HCP training should focus on stress management and emotional intelligence. Over the past two decades, workplace resiliency has emerged as a crucial factor in mitigating occupational stress and enhancing overall performance. In a manner similar to employees undergoing health and safety induction during their initial weeks at work, HCP, along with other essential workers, should receive training to develop psychological preparedness and resilience to navigate turbulent times effectively.
By heeding these recommendations, the healthcare system can better prepare HCPs to address pandemics comprehensively and efficiently, ensuring they are well-equipped to respond effectively to any future disease outbreak.
The study’s principal limitation was the low response rate among other specialties since most responders were nurses owing to the crucial time of the pandemic and lockdowns, which may not accurately represent the wider HCP population at Royal Hospital.
Conclusion
Our study underscores the need to bridge the gap between HCPs knowledge and their preparedness for dealing with highly contagious patients. This can be achieved through enhanced medical training and expanded psychological support programs tailored to HCP needs. Future research should employ qualitative methods to delve deeper into preparedness and training issues.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Satcher D. Emerging infections: getting ahead of the curve. Emerg Infect Dis 1995;1(1):1-6.
- 2. Berkelman RL, Bryan RT, Osterholm MT, LeDuc JW, Hughes JM. Infectious disease surveillance: a crumbling foundation. Science 1994 Apr;264(5157):368-370.
- 3. Low DE. SARS: lessons from Toronto. In: Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K, editors. Learning from SARS: preparing for the next disease outbreak -- workshop summary. Washington: The National Academic Press; 2004. p. 63-71.
- 4. de Rooij D, Belfroid E, Eilers R, Roßkamp D, Swaan C, Timen A. Qualitative research: institutional preparedness during threats of infectious disease outbreaks. Biomed Res Int 2020 Jan;2020(1):5861894.
- 5. Ughasoro MD, Esangbedo DO, Udorah IM. Health-care workers’ perspectives on preparedness of health-care facilities for outbreak of communicable diseases in Nigeria: a qualitative study. Am J Trop Med Hyg 2019 Apr;100(4):1022-1028.
- 6. Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, Salam M, Al-Assiri MH, Balkhy HH. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis 2017 Jan;17(1):4.
- 7. Xiao J, Fang M, Chen Q, He B. SARS, MERS and COVID-19 among healthcare workers: a narrative review. J Infect Public Health 2020 Jun;13(6):843-848.
- 8. McCloskey B, Heymann DL. SARS to novel coronavirus - old lessons and new lessons. Epidemiol Infect 2020 Feb;148(e22):e22.
- 9. Centers for Disease Control and Prevention. Hospital pandemic influenza planning checklist. 2007 [cited 2022 August 1]. Available from: https://www.cdc.gov/flu/pandemic-resources/pdf/hospitalchecklist.pdf.
- 10. Badahdah A, Khamis F, Al Mahyijari N, Al Balushi M, Al Hatmi H, Al Salmi I, et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatry 2021 Feb;67(1):90-95.
- 11. Temsah MH, Al-Sohime F, Alamro N, Al-Eyadhy A, Al-Hasan K, Jamal A, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health 2020 Jun;13(6):877-882.
- 12. Moussa ML, Moussa FL, Alharbi HA, Omer T, Khallaf SA, Al Harbi HS, et al. Fear of nurses during COVID-19 pandemic in Saudi Arabia: a cross-sectional assessment. Front Psychol 2021 Oct;12:736103.
- 13. Khanal P, Paudel K, Devkota N, Dahal M, Mishra SR, Joshi D. Corona virus fear among health workers during the early phase of pandemic response in Nepal: a web-based cross-sectional study. PLOS Glob Public Health 2021 Dec;1(12):e0000083.
- 14. Nashwan AJ, Valdez GF, Al-Fayyadh S, Al-Najjar H, Elamir H, Barakat M, et al. Stigma towards health care providers taking care of COVID-19 patients: a multi-country study. Heliyon 2022 Apr;8(4):e09300.
- 15. Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. J Anxiety Disord 2020 Aug;74:102258.
- 16. Schaffler-Schaden D, Stöllinger L, Avian A, Terebessy A, Scott AM, Streit S, et al. Gender differences in perceived working conditions of general practitioners during the COVID-19 pandemic-a cross-sectional study. J Gen Intern Med 2023 Jun;38(8):1894-1901.
- 17. Almomani MH, Khater WA, Akhu-Zaheya LM, Alloubani A, AlAshram SA, Azab M, et al. Nurses’ experiences of caring for patients with COVID-19: a qualitative study. Sage Open 2022 Dec;12(4):21582440221144982.
- 18. Mansour R, Rallapalli S, Baidwan HK, Razai MS, Abou-Abbas L. Knowledge and experience of physicians during the COVID-19 pandemic: a global cross-sectional study. PLOS Glob Public Health 2022 Jul;2(7):e0000639.
- 19. Prescott K, Baxter E, Lynch C, Jassal S, Bashir A, Gray J. COVID-19: how prepared are front-line healthcare workers in England? J Hosp Infect 2020 Jun;105(2):142-145.