Pursuing advanced subspecialty training has become a crucial aspect of training across various medical specialties.1 Surgical specialties have undergone significant changes in training requirements, such as the elimination of the prerequisite for general surgery training to join subspecialty programs in plastic surgery, vascular surgery, and cardiothoracic surgery.2 As a result, subspecialty training is gaining popularity, and more residents are expected to pursue fellowship training.
While several published reports have explored factors influencing the choice of subspecialties among surgical residents and postgraduates, there is still limited understanding.1,3–5 Previous studies have considered factors such as gender, job availability, marketability, type of practice, geographic location, personal interest, damage repair, malpractice rates, job satisfaction, financial considerations, diversity of cases, motivation, intellectual stimulation, and lifestyle counseling.2,4,6 These studies provide a general indication of the factors influencing subspecialty choices.
Against this backdrop, our study aims to investigate the factors considered most important by surgical trainees in Oman, where a significant proportion of surgeons have yet to enroll in fellowship training. This dataset can offer guidance for designing residency curricula, optimizing rotations, improving recruitment and retention of surgical residents, structuring effective mentorship programs, and offering career counseling.
Methods
A cross-sectional study was conducted at the Oman Medical Specialty Board in Muscat, Oman, involving 202 residents, fellows, and postgraduates in surgical specialties over a 10-year period (September 2011 to September 2021). The survey formation process involved conducting an English-language literature review using online databases such as PubMed and Embase [Figure 1]. The purpose was to identify relevant studies on fellowship specialty selection in surgical specialties and other medical fields. By analyzing the factors evaluated in these studies, we developed a comprehensive list of factors that can influence the selection process in surgical specialties. Each investigator independently reviewed and evaluated these factors in the context of the national health system and postgraduate education setting. This evaluation process considered the relevance of these factors to our local context. Through thorough discussion and consensus-building, the research group finalized a list of important factors specifically tailored to our local context. Factors that were deemed irrelevant or incompatible with our local context, such as residency programs with a strong tradition of placing graduates into a specific subspecialty, altruism, and the relationship between residents and faculty in fellowship programs, were excluded from the final list. The final version of the list comprised of 14 separate factors that the research group assessed as relevant to our health system and postgraduate education context [Box 1]. Each factor’s influence on their choice of fellowship was assessed using a Likert scale rating ranging from 1 to 5, with 1 indicating ‘not at all important’ and 5 representing ‘extremely important’. These factors encompassed various domains relevant to the decision-making process. They included practice location, working hours/on-call duties, prestige, potential financial compensation, variety of cases, intellectually stimulating subspecialty, lifestyle associated with the subspecialty, personal interest, marketability, specialty primarily involving outpatient/daycare surgery, potential to join an academic practice, potential to join a private or hospital-employed practice model, interaction with physicians in other specialties, and the impact of a mentor or role model.
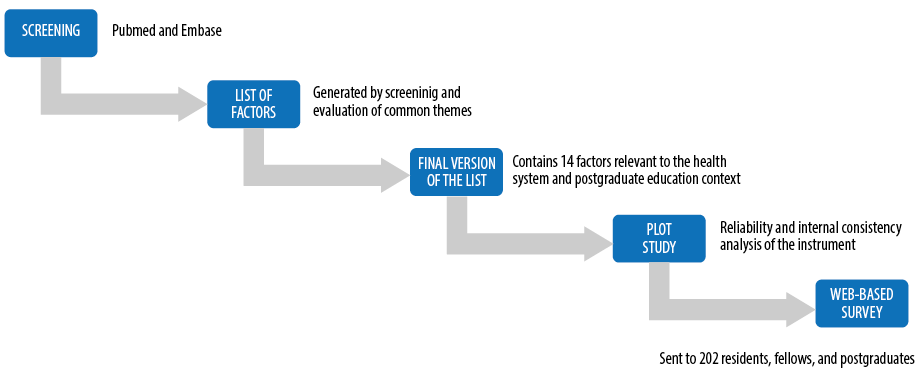 Figure 1: Flow chart illustrating the method of survey development.
Figure 1: Flow chart illustrating the method of survey development.
Box 1: Factors presented to survey respondents.
To ensure the reliability and internal consistency of the survey instrument, a pilot study was conducted. A sample of 20 residents from different surgical specialties participated in this pilot study. The survey was administered to them, and internal consistency was assessed by comparing the components of the questionnaire using Cronbach’s alpha. These results demonstrated satisfactory internal consistency and reliability of the survey instrument. In adherence to the guidelines set by the Institutional Review Board, the surveys were anonymized to ensure confidentiality and privacy of the participants.
Data analysis involved collecting survey responses, calculating sums and means, and presenting categorical data as proportions and percentages. Statistical significance was set at 5% (p < 0.05), and analysis was performed using SPSS (IBM SPSS Statistics for Windows, version 21.0; IBM, Armonk, NY, USA).
Ethical approval was obtained from the Research and Innovation Committee of Oman Medical Specialty Board on February 2022 No. 2022/09/7/1582.
Results
We received completed surveys from 123 respondents across six surgical programs (ear, nose, and throat (ENT), orthopedics, general surgery, obstetrics and gynecology, maxillofacial surgery, and ophthalmology), with a response rate of 60.9%. On average, each program was represented by 24 participants.
Prestige emerged as the most influential factor (average score of 2.7), followed by specialty involving outpatient/daycare surgery, potential to join academic practice, and interaction with physicians in other specialties (average score of 2.6). Variety of cases (average score of 1.8) and personal interest (average score of 1.4) were the least reported influential factors [Figure 2].
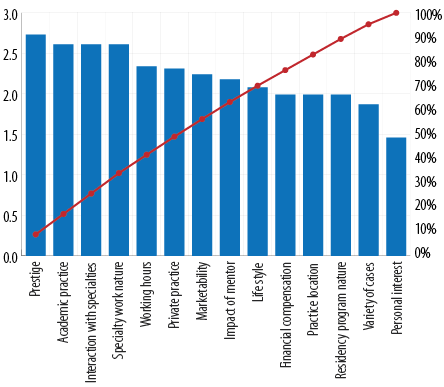 Figure 2: Mean of the score for factors influencing choice of subspecialty.
Figure 2: Mean of the score for factors influencing choice of subspecialty.
The analysis of the results for the 14 influencing factors according to the level of the surgeons who participated in the study (residents, fellows, and on-practice) did not show any significant differences in perception between the three groups. Further analysis did not show any significant difference in the perception of factors between genders or even between surgical specialties.
Participants reported receiving adequate help and support for career planning at a rate of 57.7%.
Discussion
Our study highlights several factors such as prestige, specialties primarily involving outpatient/daycare surgery, potential to join academic practice, and interaction with physicians in other specialties were the most influential in the pursuit of surgical careers. Reviewing the existing literature reveals that the factors influencing surgeons’ choice of subspecialties are still not well-understood. Several articles have identified employment opportunities, intellectual interest, strong mentorship, surgical diversity, and lifestyle as important factors in the selection of subspecialties by residents.3,7,8 However, there is ongoing controversy regarding factors such as the impact of subspecialties on lifestyle and
financial compensation.
Interestingly, our data differed from published works where personal interest and variety of cases in the specialty were identified as the least important factors affecting career choice. For example, Bakarman et al,9 reviewed a cohort of orthopedic surgeons and reported that personal interest in the specialty was the primary factor in career decision-making. Similarly, Kavolus et al,6 found that intellectual stimulation of subspecialties and case diversity were among the most important factors influencing career selection. In our data, orthopedic surgeons considered lifestyle associated with the subspecialty and marketability as the most important factors when applying for fellowship training. These observed differences could be attributed to cultural variations between the local society and the populations surveyed in similar studies. Furthermore, the structure of healthcare services in Oman, which may differ from other regions, could affect how participants plan their careers and select subspecialties to apply for.
Moreover, our data align with previous studies that examined gender differences. Bratescu et al,7 and Incorvaia et al,8 both examined gender differences and found that males were more likely to pursue fellowship training, while females placed more value on lifestyle factors. Our findings are in line with this, as female participants in our study showed that lifestyle associated with the subspecialty was more important when selecting their subspecialty compared to male participants. However, when comparing the data across surgical specialties, no significant statistical differences were observed. This may be because most surgical trainees in our study were government-employed, working under similar conditions, and facing comparable challenges. Furthermore, our data support and extend previous studies emphasizing the critical role of resident rotations and mentorship in choosing a subspecialty.7,9,10 Our findings highlight the importance of these factors in the decision-making process, as respondents prioritize them when choosing their future profession. From a training design perspective, this suggests that residents should be exposed to a wide range of subspecialties and potential mentors before making their own subspecialty choice. These findings have implications for influencing graduate professional decisions to address any surpluses or shortages of surgeons in specific subspecialties. This can be achieved primarily through providing adequate help and support in career planning and dispelling any misconceptions that may exist about certain subdisciplines. However, our results indicate that only 57.7% of participants felt they received appropriate guidance in their future career decisions. We call for the establishment of effective career guidance through collaborative efforts of stakeholders responsible for the development of the healthcare system in the country.
It is important to acknowledge that the study has limitations, such as a moderate response rate, which is consistent with similar study designs where response rates rarely exceed 75% at best.5,6,10 Additionally, some participants may have changed their specialty or career path, or their perspective on what is important may have changed over time. There is also the possibility of recall bias, as it has been a few years since they made their career decisions.
Conclusion
This study provides insights into factors influencing the career choices of surgical residents and postgraduates pursuing subspecialties. It emphasizes the importance of prestige, outpatient/daycare surgery, academic practice, and interdisciplinary collaboration. The findings can guide curriculum design, rotation optimization, recruitment and retention strategies, and effective career counseling. Further research is needed to explore these factors in different contexts and enhance understanding of subspecialty selection within surgery.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Chan JY, Charlton TP, Thordarson DB. Analysis of orthopaedic job availability in the United States based on subspecialty. J Am Acad Orthop Surg Glob Res Rev 2020 Nov 6;4(11):e20.00195.
- 2. Horst PK, Choo K, Bharucha N, Vail TP. Graduates of orthopaedic residency training are increasingly subspecialized: a review of the American board of orthopaedic surgery part II database. J Bone Joint Surg Am 2015 May;97(10):869-875.
- 3. Butler BA, Johnson D, Christian RA, Bigach SD, Beal MD, Peabody TD. Factors influencing subspecialty choice of orthopedic residents: effect of gender, year in residency, and presumptive subspecialty. Iowa Orthop J 2020;40(1):19-23.
- 4. Li X, Pagani N, Curry EJ, Alolabi B, Dickens JF, Miller AN, et al. Factors influencing resident satisfaction and fellowship selection in orthopaedic training programs: an American orthopaedic association North American traveling fellowship project. J Bone Joint Surg Am 2019 May;101(10):e46.
- 5. Matson AP, Kavolus JJ, Byrd WA, Leversedge FJ, Brigman BE. Influence of trainee experience on choice of orthopaedic subspecialty fellowship. J Am Acad Orthop Surg 2018 Feb;26(3):e62-e67.
- 6. Kavolus JJ, Matson AP, Byrd WA, Brigman BE. Factors influencing orthopedic surgery residents’ choice of subspecialty fellowship. Orthopedics 2017 Sep;40(5):e820-e824.
- 7. Bratescu RA, Gardner SS, Jones JM, Siff TE, Lambert BS, Harris JD, et al. Which subspecialties do female orthopaedic surgeons choose and why?: identifying the role of mentorship and additional factors in subspecialty choice. J Am Acad Orthop Surg Glob Res Rev 2020 Jan;4(1):e19.00140.
- 8. Incorvaia AN, Ringley CD, Boysen DA. Factors influencing surgical career decisions. Curr Surg 2005;62(4):429-435.
- 9. Bakarman KA, Zain KO, Alotaibi NA, Aldakhil AA, Alhassan AM. Factors that influence orthopedic surgeons when choosing their subspecialty in Saudi Arabia. J Musculoskelet Surg Res 2019 Apr;3:216.
- 10. Hull BP, Darrow DH, Derkay CS. The financial value of fellowship training in otolaryngology. Otolaryngol Head Neck Surg 2013 Jun;148(6):906-911.