Cardiac tumors are rare, with a reported prevalence of 0.002–0.3%. Most (75%) are benign, with myxoma being the most common benign cardiac tumor.1 The clinical presentation of cardiac tumors is usually not specific but influenced by the size, location, and embolism tendency.2 Cardiac papillary fibroelastoma (PFE) is the second most common benign cardiac tumor, and the vast majority are related to cardiac valves. PFEs rarely arise from the left ventriclar (LV) endocardium. We report a rare case of an LV mass that was excised and histopathologically confirmed to be PFE. To our knowledge, this is the first case of LV papillary fibroelastoma detected on cardiac magnetic resonance imaging (MRI) to be reported in Oman.
Case report
A 75-year-old man, known to have diabetes mellitus, was admitted to the Royal Hospital, a tertiary hospital with a history of exertional chest discomfort. His electrocardiogram showed sinus rhythm. Further evaluation with an echocardiogram revealed severe aortic valve stenosis with concentric LV hypertrophy and normal LV systolic function; ejection fraction was 59%. There was an incidental mobile lesion related to the anterolateral papillary muscle of the LV measuring 1 × 0.6 cm. Coronary angiography showed normal coronary arteries. Cardiac MRI showed a small mobile mass related to the anterolateral papillary muscle of the left ventricle, measuring 0.8 × 0.5 cm. The lesion was hyperintense in T2-weighted images and hypointense in T1-weighted images, with homogenous enhancement on post-contrast sequence [Figure1]. The impression from the cardiac MRI was suggestive of a LV myxoma.

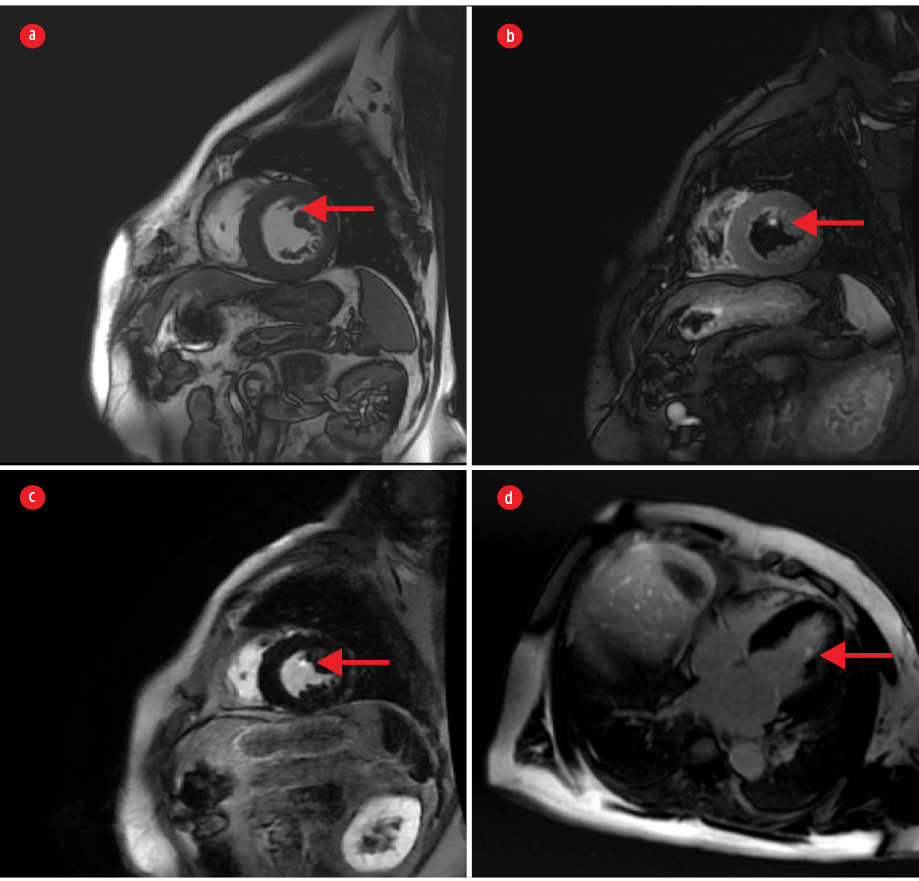 Figure 1: Cardiac magnetic resonance images showing (a) a steady-state free precision short-axis oblique and (b) T2-weighted images showing a small lesion related to the left ventricle anterolateral papillary muscle 9. An enhancing lesion related to the left ventricle anterolateral papillary muscle 9 is shown by the (c) late gadolinium enhancement short-axis oblique and (d) four-chamber view.
Figure 1: Cardiac magnetic resonance images showing (a) a steady-state free precision short-axis oblique and (b) T2-weighted images showing a small lesion related to the left ventricle anterolateral papillary muscle 9. An enhancing lesion related to the left ventricle anterolateral papillary muscle 9 is shown by the (c) late gadolinium enhancement short-axis oblique and (d) four-chamber view.
The patient underwent open cardiac surgery for aortic valve replacement and excision of the LV mass. Microscopic examination of the excised lesion showed branching papillary fronds composed of avascular fibroblastic cores surfaced by a single layer of bland endocardium [Figure 2]. Histopathology findings were consistent with PFE.

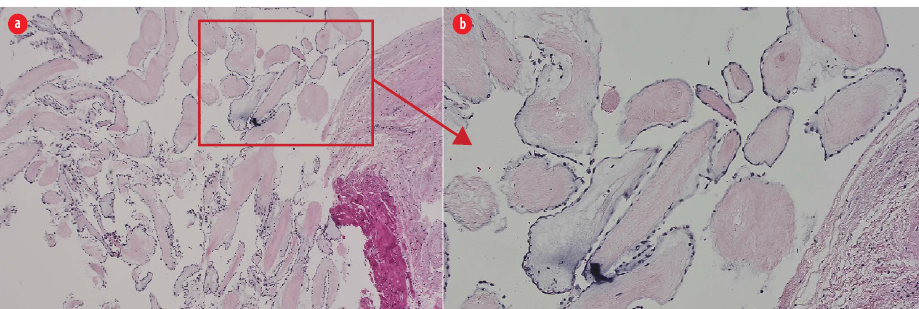 Figure 2: Microscopic section of the excised lesion in two magnifications. (a) The lesion is seen composed of many papillary fronds, (hematoxylin and eosin staining, magnification = 40 ×). (b) The papillary fronds reveal avascular hyalinized cores lined by a single layer of endocardial cells, magnification = 100 ×.
Figure 2: Microscopic section of the excised lesion in two magnifications. (a) The lesion is seen composed of many papillary fronds, (hematoxylin and eosin staining, magnification = 40 ×). (b) The papillary fronds reveal avascular hyalinized cores lined by a single layer of endocardial cells, magnification = 100 ×.
Discussion
PFE is a small, benign endocardial tumor accounting for < 10% of all primary cardiac tumors.3,4 They are thought to be acquired rather than inherited.4,5 A 2015 study reported that PFEs were more common than cardiac myxomas, reversing a previous assumption.4,6 PFEs present at a mean age of 60 years but can occur at any age and in both sexes.4,5,7,8 Another study that assessed 54 PFE cases found increased prevalence in the sixth and eighth decades; indeed, our patient was in his eighth decade
at presentation.5
Around 90% of cases, PFE is found in the cardiac valves. The other locations include LV or atrium, right ventricle or atrium, atrial septum, papillary muscle, chordate tendinea, Eustachian valve, and Chiari network.7 Nonvalvular right-sided PFEs are more common than those found on the left side.6
Being mostly asymptomatic, PFEs are usually detected incidentally during echocardiogram, cardiac surgery, or autopsies.5 Some patients are symptomatic and may present with acute stroke related to embolization, syncope, angina, myocardial infarction, and even sudden cardiac death.4,7 The clinical presentation depends on the size, location, growth rate, and mobility of the tumor. As they are predominantly found in the left side of the heart (particularly the aortic valve), symptoms related to embolization are common.4,5,9 The usual presenting symptom is a neurological event—either transient ischemic attack or stroke.6 A meta-analysis of 725 cases reported the most common presenting symptom of PFE as transient ischaemic attack or stroke (44%) followed by angina (18%).8
We could not find any prior study that discussed the most frequent symptoms of LV PFE, such as in our patient, who presented with exertional chest pain. Hyun et al,7 reported a patient with LV PFE who presented with chest pain, while de Klerk et al,4 reported dyspnea.
PFEs are composed of fibroelastic tissue surrounded by the endocardium. The hallmark of PFE is the presence of elastic fibers in variable distribution, making their demonstration difficult.8 The proposed predisposing pathological processes leading to PFE include epithelial hyperproliferation from hemodynamic damage to the endothelium, trauma, and organized thrombus.5
Multimodality imaging is essential for the evaluation of all cardiac mass including PFEs. On transthoracic echocardiogram, PFE typically appears as a round mobile homogenous echogenic lesion with a stalk connecting to the endocardium.4,10 Transesophageal echocardiogram has higher sensitivity, especially for smaller lesions.4,8 Cardiac MRI, which we used, gives better details of the tumor tissue characteristics.11,12 The MRI typically reveals a mass on the endocardial surface of the cardiac structure, commonly on the valve leaflets.3,8 On T1- and T2-weighted images, PFE demonstrates a well-circumscribed homogenous intermediate signal intensity to the myocardium, which represents fibroelastic tissue. The cine gradient echo sequence may show the tumor mobility and perilesional flow artifact due to turbulent blood flow.3,8,9,13 PFE shows diffuse homogenous late gadolinium enhancement which differentiates the tumor from thrombus, a well-known tumor mimicker.8,13
As tumor characteristics often overlap on imaging, differentiating between PFE and myxoma can be difficult, especially when PFE arises from a non-valvular cardiac structure, as in our case.4,9 Here, electrocardiogram-gated (computed tomography) imaging can show thinner sections and better anatomical details such as the details of small stalk PFE more clearly than MRI,11 and can better demonstrate calcifications, often found in cardiac myxoma.4,12 Contrast-enhanced CT is another imaging method able to provide enhanced images of PFE lesions.11
Both MRI and CT can assess the integrity of cardiac valves and the extent of any tumor arising from a valve.12 The presence of valvular destruction helps in differentiating infective endocarditis vegetation from PFE, although infective endocarditis is generally clear clinically.9,13
The treatment options include curative surgical removal versus follow-up. Surgical excision is the treatment of choice in symptomatic patients.8 Both short and long-term prognoses after surgery are excellent with no reported recurrence.4,7 Tumor mobility is an independent predictor of embolization and death.4,8 Therefore, cases of asymptomatic mobile PFE should be considered for surgical removal. Follow-up is an option for asymptomatic patients with non-mobile PFE. In a follow-up group of 317 patients, the risk of cerebrovascular accident was 6% and 13% at one and five years, respectively.6
Conclusion
Cardiac papillary fibroelastomas are rare benign tumors that are typically related to cardiac valves. Occasionally, PFE can also grow in the LV cavity. Most PFE patients are asymptomatic; however, some patients can present with symptoms depending on the size and location of the lesion. Awareness of the cardiac MRI findings of characteristic of PFE can facilitate pre-operative diagnosis with high confidence.
Disclosure
The authors declared no conflicts of interest. Informed consent for publication of this case was obtained from the patient.
references
- 1. Leja MJ, Shah DJ, Reardon MJ. Primary cardiac tumors. Tex Heart Inst J 2011;38(3):261-262.
- 2. Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S. MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology 2013 Jul;268(1):26-43.
- 3. Grebenc ML, Rosado de Christenson ML, Burke AP, Green CE, Galvin JR. Primary cardiac and pericardial neoplasms: radiologic-pathologic correlation. Radiographics 2000;20(4):1073-1103, quiz 1110-1111, 1112.
- 4. de Klerk S, Dogon C, Grossman M, Adler JE, McFalls J, Furukawa S, et al. Left ventricular papillary fibroelastoma presenting with dyspnea on exertion. CASE (Phila) 2020 Feb;4(4):278-282.
- 5. Cianciulli TF, Soumoulou JB, Lax JA, Saccheri MC, Cozzarin A, Beck MA, et al. Papillary fibroelastoma: clinical and echocardiographic features and initial approach in 54 cases. Echocardiography 2016 Dec;33(12):1811-1817.
- 6. Tamin SS, Maleszewski JJ, Scott CG, Khan SK, Edwards WD, Bruce CJ, et al. Prognostic and bioepidemiologic implications of papillary fibroelastomas. J Am Coll Cardiol 2015 Jun;65(22):2420-2429.
- 7. Hyun JY, Jung IH, Lee HJ, Lee SJ, Kim JS, Na CY, et al. A case of papillary fibroelastoma in the left ventricle. Korean J Intern Med 2013 Jan;28(1):89-93.
- 8. Gowda RM, Khan IA, Nair CK, Mehta NJ, Vasavada BC, Sacchi TJ. Cardiac papillary fibroelastoma: a comprehensive analysis of 725 cases. Am Heart J 2003 Sep;146(3):404-410.
- 9. Sparrow PJ, Kurian JB, Jones TR, Sivananthan MU. MR imaging of cardiac tumors. Radiographics 2005;25(5):1255-1276.
- 10. Mariscalco G, Bruno VD, Borsani P, Dominici C, Sala A. Papillary fibroelastoma: insight to a primary cardiac valve tumor. J Card Surg 2010 Mar;25(2):198-205.
- 11. Rahsepar AA, Ghasemiesfe A, Sawlani RN, Ferreira Botelho MP, Paintal AS, Tumer Y, et al. A papillary fibroelastoma involving aortic and pulmonary valves: findings on multimodality imaging. Ann Thorac Surg 2017 Jan;103(1):e73-e75.
- 12. Wintersperger BJ, Becker CR, Gulbins H, Knez A, Bruening R, Heuck A, et al. Tumors of the cardiac valves: imaging findings in magnetic resonance imaging, electron beam computed tomography, and echocardiography. Eur Radiol 2000;10(3):443-449.
- 13. Hoey ET, Shahid M, Ganeshan A, Baijal S, Simpson H, Watkin RW. MRI assessment of cardiac tumours: part 1, multiparametric imaging protocols and spectrum of appearances of histologically benign lesions. Quant Imaging Med Surg 2014 Dec;4(6):478-488.