An 11-year-old boy presented with gradual thickening, scaling, and redness of the skin on his palms and soles that began at the age of seven for which he had been receiving topical corticosteroid treatment from the local primary health care center. Additionally, at age eight, the patient developed gingivitis, leading to a subsequent diagnosis of periodontitis [Figures 1 and 2].

 Figure 1: Gingival inflammation and spacing of teeth.
Figure 1: Gingival inflammation and spacing of teeth.

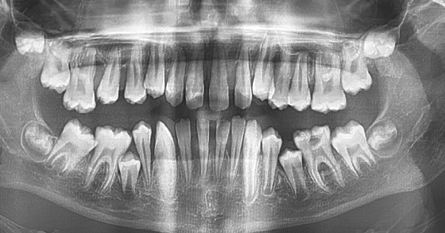 Figure 2: Orthopantomagram showing severe alveolar bone loss.
Figure 2: Orthopantomagram showing severe alveolar bone loss.
The patient has two siblings, aged 21 and 20 years old, who have been diagnosed with psoriasis but do not exhibit palmoplantar keratoderma (PPK)
or periodontitis.
On physical examination, he had a slender build, and dental abnormalities were noted. Systemic examinations were unremarkable. Dermatological examination [Figures 3 and 4] revealed transgradient PPK with well-defined margins on the dorsum of the hands and feet, as well as punctate keratoderma on the plantar surfaces of both feet. Additionally, there were small psoriasiform plaques on both knees.

 Figure 3: Transgradient palmoplantar keratoderma with sharp margins on the dorsum of the feet.
Figure 3: Transgradient palmoplantar keratoderma with sharp margins on the dorsum of the feet.

 Figure 4: Punctate keratoderma on the planter surfaces.
Figure 4: Punctate keratoderma on the planter surfaces.
Question
What is the most likely diagnosis?
a. Huriez syndrome.
b. Olmsted syndrome.
c. Papillon-Lefèvre syndrome.
d. pachyonychia congenita.
Answer
c. Papillon-Lefèvre syndrome.
The diagnosis is based on history, typical skin lesions, dental findings, and molecular genetic testing.
Discussion
The patient's compelling clinical features, including hyperkeratosis and erythema of the palms and soles, characterized as PPK, along with the development of severe destructive periodontal disease fits the diagnosis of Papillon-Lefèvre syndrome (PLS), also known as keratosis palmoplantaris with severe periodontitis.
PLS is an autosomal recessive disorder resulting from mutations in the cathepsin C (CTSC) gene.1,2 This rare autosomal recessive disorder is characterized by a combination of skin and periodontal abnormalities. The hallmark features of PLS include PPK as well as severe destructive periodontal
disease that affects primary and permanent teeth before the age of four.1 Patients with PLS generally report two episodes of periodontitis, the first of which occurs at the age of three and leads to the loss of primary teeth by the age of five. The second episode usually occurs around the age of 15 and leads to the loss of permanent teeth.1 Radiographic assessment in advanced cases shows a significant alveolar bone loss, giving the impression that the teeth are suspended without proper support as seen in our patient.3
Cutaneous lesions typically appear conco-mitantly with intraoral manifestations. The plantar hyperkeratosis is characterized by well-demarcated erythematous keratotic plaques, which may spread transgrediens to the edges of the soles and, in some cases, to the skin overlying the Achilles tendon and the external malleoli.2 Psoriasiform lesions, resembling psoriasis, may also develop over the elbows, knees, and knuckles in patients with PLS. Other symptoms of PLS may include hyperhidrosis, arachnodactyly, intracranial calcification, increased susceptibility to infections, and mental retardation.3
The differential diagnoses include Huriez syndrome, Olmsted syndrome, Pachyonychia congenita, and PLS, all rare genetic disorders that can cause skin and nail abnormalities. However, each syndrome has distinct clinical features that can help differentiate it from the others. Huriez syndrome is characterized by hyperkeratotic plaques, sclerodactyly-like appearance of hands and feet, nail changes, growth delays, and increased risk of squamous cell carcinoma.4 The Olmsted syndrome has two forms: the autosomal dominant form caused by mutations in TRPV337 and the X-linked form caused by a mutation in MBTPS248, both showing diffuse and mutilating PPK, perioral hyperkeratotic plaques with severe pruritus, and various other clinical features that are not present in this patient.4 Pachyonychia congenita is characterized by thickened nails, hyperkeratosis of the palms and soles, oral leukokeratosis, follicular keratosis, and pilosebaceous cysts, with mutations in the KRT6A, KRT6B, KRT16, and KRT17 genes.4
The diagnosis of PLS involves a thorough clinical evaluation that includes a detailed patient history and identification of characteristic physical findings. Additionally, urine analysis can be used to test for the activity of the cathepsin C enzyme. Little or no activity of this enzyme is diagnostic of PLS. The diagnosis can be further confirmed by molecular genetic testing. Whole exome sequencing of this patient showed a homozygous variant of uncertain significance in the CTSC gene.
A multidisciplinary approach involving dermatologists, pediatricians, and pediatric dentists is crucial for the comprehensive care of patients with PLS. Dental care and the use of prophylactic antibiotics are important in minimizing periodontitis and tooth loss.5 Oral retinoids, such as acitretin, have shown effectiveness in improving skin lesions and periodontal inflammation in PLS patients, potentially leading to normal dentition if treatment is initiated early.5 Genetic counseling is essential for affected individuals and their families, and psychosocial support is recommended for the entire family.
Conclusion
A thorough clinical evaluation and genetic testing are essential for distinguishing PLS from similar syndromes with skin and nail abnormalities. Early diagnosis and a multidisciplinary approach are vital for improving the quality of life for individuals with PLS and their families.
Disclosure
The authors declared no conflicts of interest. Written informed consent was obtained from the patient’s parents.
references
- 1. Kurban M, Cheng T, Wajid M, Kiuru M, Shimomura Y, Christiano AM. A novel mutation in the cathepsin C gene in a Pakistani family with Papillon-Lefevre syndrome. J Eur Acad Dermatol Venereol 2010 Aug;24(8):967-969.
- 2. National Organization for Rare Disorders. Papillon Lefèvre syndrome. 2019 [cited 2023 May 8]. Available from: https://rarediseases.org/rare-diseases/papillon-lefevre-syndrome/.
- 3. Sreeramulu B, Shyam ND, Ajay P, Suman P. Papillon-Lefèvre syndrome: clinical presentation and management options. Clin Cosmet Investig Dent 2015 Jul;7:75-81.
- 4. Sakiyama T, Kubo A. Hereditary palmoplantar keratoderma "clinical and genetic differential diagnosis". J Dermatol 2016 Mar;43(3):264-274.
- 5. Al-Khenaizan S. Papillon-Lefévre syndrome: the response to acitretin. Int J Dermatol 2002 Dec;41(12):938-941.