The anterolateral ligament (ALL) of the knee joint was initially described by Paul Segond in 1879 as a distinct fibrous band from the knee capsule, often associated with an avulsion fragment of the proximal anterolateral tibia due to traumatic internal rotation.1 In brief, ALL shows an oblique intracapsular course with its origin on the posterior proximal region of the lateral femoral epicondyle and its insertion between Gerdy’s tubercle and the fibular head. Additionally, ALL may have almost constant attachments to the periphery of the lateral meniscus around its middle portion.2 The ALL can be divided into three anatomical regions: the femoral, the middle, and the tibial. Studies have reported similar rates of injury location for the femoral and tibial regions, up to 72% and 100%, respectively, while abnormalities in the middle portion of the ligament occur in only 11% of cases [Figure 1].3–5 This may be explained by the ligament being more easily identified in the distal and proximal portions than in the meniscal portion.6 Furthermore, Claes et al,3 assumed that the distal portion of the ALL acts as a lever arm far away from the functional axis (transepicondylar axis) of the knee joint, increasing tension on the distal part and explaining the high proportion of injuries in this anatomical site. Claes et al,3 characterized abnormal ALL as cases of complete fiber disruption of the ligament, irregular contour appearance, and intra- or peri-ligament edema [Figure 1].

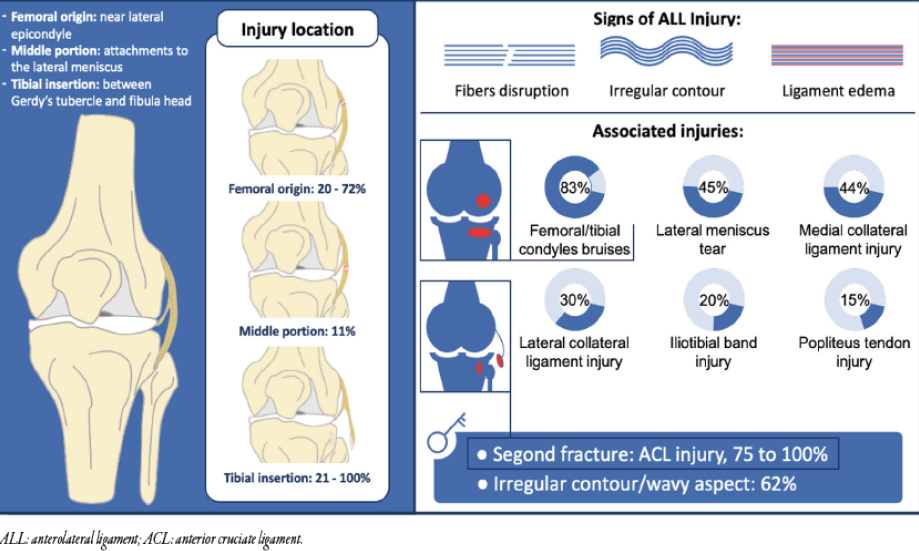 Figure 1: Anterolateral ligament abnormalities and its associated injuries.
Figure 1: Anterolateral ligament abnormalities and its associated injuries.
In the setting of an acute knee injury, magnetic resonance imaging (MRI) has a slice thickness of 3 mm and may be problematic in detecting an ALL tear.7 Thus, to assist radiologists in diagnosing ALL tears accurately, several direct and/or indirect signs on MRI have been proposed, such as Segond fracture, bone bruises of the lateral femoral/tibial condyle, and the wavy appearance of the ALL shape [Figure 1].5,7 Furthermore, ALL abnormalities can be significantly associated with femoral/tibial bone bruises, lateral meniscus tear, medial/ lateral collateral ligament injury, iliotibial band injury, and popliteus tendon injury [Figure 1].1,2 It is well noted in the literature that a Segond fracture has a high association with anterior cruciate ligament (ACL) ruptures, being present in 75% to 100% of cases.8 Additionally, there is a significant deviation, ranging from 40% to 80%, of ALL injury on MRI when an ACL tear is present.2 Thus, clinicians should have a high index of suspicion for ALL injury when evaluating MRI scans for an acute ACL tear.
references
- 1. Puzzitiello RN, Agarwalla A, Zuke WA, Garcia GH, Forsythe B. Imaging diagnosis of injury to the anterolateral ligament in patients with anterior cruciate ligaments: association of anterolateral ligament injury with other types of knee pathology and grade of pivot-shift examination: a systematic review. Arthroscopy 2018 Sep;34(9):2728-2738.
- 2. Ferretti A, Monaco E, Redler A, Argento G, De Carli A, Saithna A, et al. High prevalence of anterolateral ligament abnormalities on MRI in knees with acute anterior cruciate ligament injuries: a case-control series from the SANTI study group. Orthop J Sports Med 2019 Jun;7(6):2325967119852916.
- 3. Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 2014 Mar;80(1):45-49.
- 4. Marshall T, Oak SR, Subhas N, Polster J, Winalski C, Spindler KP. Can the anterolateral ligament be reliably identified in anterior cruciate ligament – intact and anterior cruciate ligament – injured knees on 3-T magnetic resonance imaging? Orthop J Sports Med 2018 Sep;6(9):2325967118796452.
- 5. Helito CP, Helito PV, Costa HP, Demange MK, Bordalo-Rodrigues M. Assessment of the anterolateral ligament of the knee by magnetic resonance imaging in acute injuries of the anterior cruciate ligament. Arthroscopy 2017 Jan;33(1):140-146.
- 6. Sonnery-Cottet B, Daggett M, Fayard J-M, Ferretti A, Helito CP, Lind M, et al. Anterolateral ligament expert group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament - deficient knee. J Orthop Traumatol 2017 Jun;18(2):91-106.
- 7. Shekari I, Shekarchi B, Abbasian M, Minator Sajjadi M, Momeni Moghaddam A, Kazemi SM. Predictive factors associated with anterolateral ligament injury in the patients with anterior cruciate ligament tear. Indian J Orthop 2020 Jun;54(5):655-664.
- 8. Arneja SS, Furey MJ, Alvarez CM, Reilly CW. Segond fractures: not necessarily pathognemonic of anterior cruciate ligament injury in the pediatric population. Sports Health 2010 Sep;2(5):437-439.