Venous thromboembolism (VTE) is the third most common vascular disease.1 In Europe and the USA, VTE is reported to cause “more deaths each year than breast cancer, HIV disease, and motor vehicle crashes combined”, and that “approximately 60% of VTE events are associated with a recent hospital stay”.2 Moreover, VTE is the leading preventable cause of death among inpatients.3 Pulmonary embolism, which causes blockage of arteries in the lungs, is responsible for an additional 5–10% of in-hospital deaths.4 Long-term complications of VTE such as chronic thromboembolic hypertension and post-thrombotic syndrome can lead to significant lifelong morbidity and increased cost of management.3 Timely prophylaxis can substantially reduce the likelihood of these.
Organizations such as the American College of Chest Physicians (ACCP) and the American Society of Hematology have provided evidence-based recommendations on the appropriate VTE prophylaxis based on the patient’s comorbidities and risk factors.1,5 Despite this, studies and audits suggest that the recommended guidelines are often not followed and mechanical prophylaxis facilities remain markedly underused.6
The 2008 Epidemiologic International Day for the Evaluation of Patients at Risk for Venous Thromboembolism in the Acute Hospital Care Setting (ENDORSE) study had 32 participating countries including three Arabian Gulf countries. The study was benchmarked on the 2004 ACCP evidence-based consensus guidelines, which reported that 51.8% of hospitalized patients were at risk for VTE. However, among them, only 58.5% of surgical patients and 39.5% of medical patients received the recommended VTE prophylaxis.3
Oman was not a participant in the ENDORSE study and there is no published data regarding the local compliance with standards and recommendations in VTE prophylaxis for hospitalized patients. Recently, some of the tertiary care hospitals in Oman adopted VTE risk assessment questionnaires which are filled by the admitting physicians for each newly admitted patient, but no local audit has been conducted to assess the compliance and practice. Besides, these risk assessment charts are only electively filled, and they do not give recommendations on the type, timing, or dose of the prophylactic regimen based on the patient’s medical history and risk factors. To develop stricter local protocols in Oman, we should initially assess the prevalence of patients at VTE risk in acute care hospital settings and the proportion that receives the appropriate thromboprophylaxis.
The findings from the ENDORSE study in countries adjacent to Oman do not negate the necessity for a local investigation. Furthermore, the ENDORSE study did not assess the initiation timing of VTE prophylaxis, thereby not accounting for potential delays in initiating VTE prophylaxis for patients at risk. Consequently, the need for a national multicenter study became essential, culminating in the present study. Accordingly, we aimed to evaluate the prevalence of patients at VTE risk in acute care settings in Oman and to find the proportion of patients who received appropriate thromboprophylaxis. A secondary objective was to identify the types of thromboprophylaxis used and estimate the timing of their initiation.
Methods
This multicenter cross-sectional study was conducted from August to September 2022 in three large hospitals in Oman: Sultan Qaboos University Hospital, Royal Hospital, and Sohar Hospital. Ethical approval for the study was given by the Health Studies and Research Approval Committee, Ministry of Health (Ref. MoH/CSR/22/2542) and the Medical Research Ethics Committee, Sultan Qaboos University Hospital (Ref. SQU-EC/ 001/2022 MREC #2697). No consent was taken from the included patients.
The study included medical patients aged ≥ 35 years who were admitted under general acute medicine, medical subspecialties, hematology, and oncology, as well as surgical patients aged ≥ 18 years admitted under general surgery, orthopedics, and gynecology. We excluded patients who, at the time of data collection, were in intensive care units and obstetric wards, patients admitted solely for the treatment of VTE, patients on long-term anticoagulation treatment for any reason (e.g., atrial fibrillation or history of thrombosis), and patients admitted for elective procedure under local anesthesia.
Data on patient demographics, reason of admission, risk factors for thrombosis and bleeding, and type and time of administering the VTE prophylaxis were obtained from the respective hospital information systems. EpiData software (EpiData Association, Denmark, version 4.6.0.6) was used to collect and organize patient information. We used the 2012 ACCP guidelines to assess our subjects’ VTE risk and prophylaxis data. Trained physicians collected the data in all three hospitals.
For sample size calculation, we estimated a VTE risk of about 50% (as found in the ENDORSE study), with a desired CI of 95%, power of 80%, and alpha error of 5%. This resulted in a sample size of 384. A convenient sampling method was used for sample selection.
Continuous variables were presented as mean, median, IQR, and SD. Categorical variables were presented as frequencies and percentages with 95% CI. SPSS Statistics (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.) was used for data analysis.
Results
The subjects were comprised of 384 inpatients; of whom, 240 (62.5%) were medical patients and 144 (37.5%) were surgical patients. The median age was 61 (IQR = 43–73) years. The median length of hospital stay as on the day of data collection was three days (IQR = 1–5) [Table 1].
Table 1: Characteristics of patients included in the study (N = 384).
|
Sex, female
|
185 (48.2)
|
|
Age, years, median (IQR)
|
61 (43–73)
|
|
Days hospitalized till the survey date, median (IQR)
|
3 (1–5)
|
|
No. of patients per hospital
|
|
|
Royal Hospital
|
133 (34.6)
|
|
Sultan Qaboos University Hospital
|
118 (30.7)
|
|
Sohar Hospital
|
133 (34.6)
|
|
Patient category
|
|
|
Medical
|
240 (62.5)
|
Table 2: Reasons for hospitalization of medical and surgical inpatients (N = 384).
|
Medical patients
|
|
|
Acute heart failure
|
21 (8.8)
|
|
Acute respiratory disease (infectious and noninfectious)
|
55 (22.9)
|
|
Non-respiratory infection
|
40 (16.7)
|
|
Ischemic stroke
|
9 (3.8)
|
|
Hemorrhagic stroke
|
6 (2.5)
|
|
Active malignancy
|
32 (13.3)
|
|
Hematological disease
|
32 (13.3)
|
|
Gastrointestinal/hepatobiliary disease
|
15 (6.3)
|
|
Other medical conditions
|
30 (12.5)
|
|
Surgical patients
|
|
|
Hip or knee replacement
|
4 (2.8)
|
|
Hip fracture
|
3 (2.1)
|
|
Other orthopedic trauma
|
25 (17.4)
|
|
Gastrointestinal/colorectal/hepatobiliary surgery
|
52 (36.1)
|
|
Gynecological surgery
|
16 (11.1)
|
|
Conservative management of acute surgical illness
|
14 (9.7)
|
The most common causes of admission for medical patients were acute respiratory disease and non-respiratory infections. Most surgical patients were admitted for gastrointestinal, colorectal, and hepatobiliary surgery, followed by orthopedic trauma [Table 2].

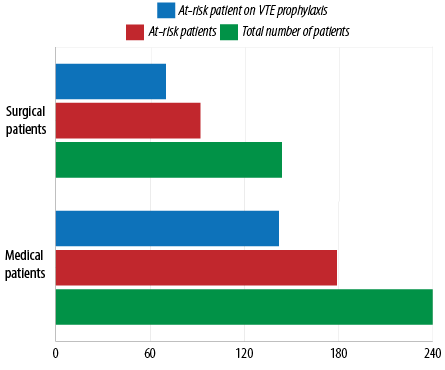 Figure 1: Prophylaxes administered to patients compared to their risk of venous thromboembolism (VTE).
Figure 1: Prophylaxes administered to patients compared to their risk of venous thromboembolism (VTE).
The most common risk factors for VTE were complete immobilization or immobilization with bathroom privilege, long-term immobility, active cancer, and obesity (body mass index > 30) [Table 3].
Table 3: Most common risk factors for venous thromboembolism among inpatients (N = 384).
|
Obesity (BMI > 30)
|
40 (10.4)
|
|
Active cancer
|
68 (17.7)
|
|
Long-term immobility
|
107 (27.9)
|
|
Acute heart failure or other respiratory disease
|
46 (12.0)
|
|
Pulmonary infection
|
56 (14.6)
|
|
Complete immobilization or immobilization with bathroom privilege
|
177 (46.1)
|
|
Sepsis
|
57 (14.8)
|
|
Acute neurological disease
|
29 (7.6)
|
|
Mechanical ventilation
|
28 (7.3)
|
The total number and percentage exceeded the number of participants because some patients had more than one risk.
BMI: body mass index; ICU: intensive care unit.
The most common bleeding risk factors among the patients were significant renal impairment, thrombocytopenia, bleeding during admission, and significant liver disease [Table 4].
Table 4: Bleeding risk factors among hospitalized patients (N = 384).
|
Deranged coagulation screen (inherited or acquired)
|
6 (1.6)
|
|
Thrombocytopenia
|
|
|
Platelet (50–100) × 109/L
|
12 (3.1)
|
|
Platelet (25–49) × 109/L
|
7 (1.8)
|
|
Platelet < 25 × 109/L
|
5 (1.3)
|
|
Bleeding during admission
|
16 (4.2)
|
|
Intracranial hemorrhage
|
3 (0.8)
|
|
Significant liver disease
|
13 (3.4)
|
|
Active gastrointestinal bleeding
|
8 (2.1)
|
GFR: glomerular filtration rate.
Among the medical inpatients, 179 (74.6%) were at risk of VTE, of whom 142 (79.3%) received appropriate prophylaxis. Among the surgical patients, 92 (63.9%) had VTE risk, of whom 70 (76.1%) received appropriate prophylaxis [Figure 1]. Interestingly, both VTE risk prevalence and the rate of compliance on VTE prophylaxis for at-risk patients were similar in all three hospitals with overlapping 95% CI [Table 5].
Table 5: Prevalence of risk of venous thromboembolism and prophylaxis use.
|
Royal Hospital
|
133
|
87
|
65.4 (57.3–73.5)
|
68
|
78.2 (69.5–86.8)
|
|
SQU Hospital
|
118
|
83
|
70.3 (62.1–78.6)
|
66
|
79.5 (70.8–88.2)
|
|
Sohar Hospital
|
133
|
101
|
75.9 (68.7–83.2)
|
78
|
77.2 (69.1–85.4)
|
SQU: Sultan Qaboos University.
The high-risk patients in this study (59; 15.4%) who did not receive appropriate prophylaxis were separately evaluated for bleeding risk that could have contraindicated pharmacological prophylaxis. Of them, 29 (49.2%) were found to have bleeding risk [Table 6].
All the three institutions studied used mechanical prophylaxis the least frequently as Figure 2 shows.

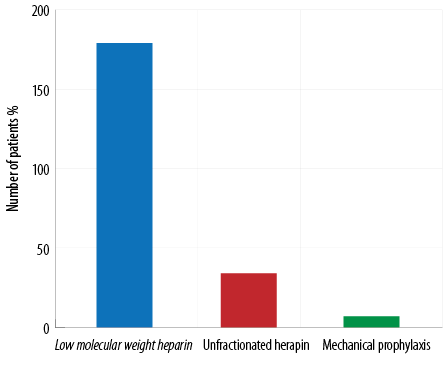 Some patients required more than one type of VTE prophylaxis throughout their hospitalization period based on their bleeding risk and medical condition.
Some patients required more than one type of VTE prophylaxis throughout their hospitalization period based on their bleeding risk and medical condition.
Figure 2: Types of prophylaxis used for at-risk patients for venous thromboembolism (n = 220).
Table 6: Patients at high risk for both venous thromboembolism and bleeding, but were not given prophylaxis (n = 59).
|
Bleeding risk
|
|
|
Bleeding during admission
|
13 (22.0)
|
|
Thrombocytopenia
|
8 (13.6)
|
|
Significant liver disease
|
5 (8.5)
|
|
Deranged coagulation screen
|
3 (5.1)
|
|
Significant renal impairment
|
11 (18.6)
|
|
Family refused prophylactic anticoagulation
|
1 (1.7)
|
The VTE prophylaxis was initiated on median day one (IQR = 1–2) of admission for medical patients and surgical patients who did not undergo surgical intervention. For surgical patients who did undergo surgery, VTE prophylaxis was initiated on median postoperative day one (IQR = 0–1).
Discussion
This is the first study in Oman to evaluate VTE prevalence and the practice of prophylaxis. It showed that most acutely ill inpatients in Oman are at significant risk of VTE and require prophylaxis. However, despite all national efforts, around one-fifth of the patients in our study did not receive appropriate prophylaxis. We also found that the prevalence of VTE risk and the rate of compliance with VTE prophylaxis recommendations were similar in the three hospitals.
We found that 70.6% of hospitalized patients in Oman were at risk of VTE is higher than, yet comparable to, the mean VTE risk of 62% in the three neighboring Arabian Gulf countries that participated in the ENDORSE.6 The rate of compliance with VTE prophylaxis recommendations in Oman is relatively better than the majority of countries involved in the ENDORSE study.3 However, this may not be a fair comparison because the ENDORSE study was conducted more than a decade earlier than ours. A more recent study in South Africa in 2019, which evaluated VTE risk among surgical patients and the rate of compliance with ACCP recommended prophylaxis and Caprini risk assessment model showed that 77% of the patients were at risk of VTE (similar to ours), but only 26% of them received the appropriate prophylaxis (much less than ours).7
While 49.2% of our at-risk patients had a significant risk of bleeding and could not be given pharmacological prophylaxis, those patients were not kept on the recommended prophylaxis in such cases which is the mechanical prophylaxis. In other Gulf countries, mechanical prophylaxis was used in 8% of high-risk patients.6 A South African study suggested a shortage of mechanical prophylaxis devices as a contributing factor to the poor compliance with VTE prophylaxis among patients with bleeding risk.7 Besides, under-documentation of mechanical VTE prophylaxis in a hospital can produce incorrect statistics. Awareness issues among clinicians may also lead to underutilization of mechanical prophylaxis. Mechanical prophylactic devices should be available in sufficient numbers. New research and audits should assess the availability of mechanical prophylaxis devices and clinicians’ awareness of their importance and availability.
This study evaluated an important factor that was not assessed in the ENDORSE study. We assessed the time of initiating VTE prophylaxis, a new evidence-based requirement. According to the 2021 National Institute for Health and Care Excellence guidelines for the management of VTE in adults, prophylaxes should be initiated within 14 hours of admission.8 A University of Michigan study found that initiation of VTE prophylaxis within 24 hours of hospital presentation in stable trauma patients was associated with significantly lower rates of VTE.9 A more recent study reported that delayed initiation (after 24 hours of admission) in critically ill patients with low bleeding risk was independently associated with higher mortality.10 The current study showed that in most cases, VTE prophylaxis was initiated early—within one day of admission/surgery—indicating good awareness and compliance among medical professionals in Oman. One limitation, however, was that our physicians reported the initiation time in days post-admission/surgery. For the future, we recommend that the time of initiating VTE prophylaxis is recorded in hours after admission/surgery for a more accurate assessment of compliance.
This study has several limitations. First, the cross-sectional design required us to rely on patient data from the hospital information system rather than meeting the patient to take detailed updated history. Second, the median day of admission on which the survey was conducted was day three, which means that the study was unable to assess whether all patients were kept on prophylaxis for optimum periods. This might have caused some overestimation of the rate of compliance. Third, the possibility that a few trauma patients with contraindications to both pharmacological and mechanical prophylaxis may have been falsely counted among high-risk patients who did not receive the appropriate prophylaxis. Finally, as mentioned earlier, mechanical prophylaxis is not well documented in our hospital information systems, and the data was only extracted from the clinical notes. This carries a strong possibility of underestimating the actual use of the facility.
Despite the relatively good local compliance in Oman on VTE prophylaxis recommendations compared to other international studies, for a such feasibly preventable leading cause of mortality among inpatients, our target compliance rate should be much higher and approaching 100%. A stricter tool that provides recommendations according to the individualized patient risk scores should be developed. This tool should also allow for easy monitoring of compliance. More objective VTE risk assessment models and scales such as the Padua and Caprini scores should be utilized to build risk assessment tools to guide clinicians.11,12 Assessment of the duration of VTE prophylaxis during and after hospital stay for orthopedic surgery patients is required to ensure that the appropriate prophylaxis is maintained for the entire ACCP-recommended period.13 Awareness of the importance of mechanical prophylaxis should be inculcated. An adequate number of devices must be made available in all local healthcare institutions.
Conclusion
VTE is a preventable complication that can lead to mortality, morbidity, and increase the cost of management among hospitalized medical and surgical patients. This study showed that a substantial proportion of hospitalized patients in Oman are at risk of VTE. However, despite the efforts, many patients do not receive appropriate prophylaxis. A national VTE risk assessment and guiding tool that allows for monitoring compliance is required. Alternative mechanical prophylaxis facilities should be utilized when indicated.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgments
We would like to thank Mr. Sathiya Murthi Panchatcharam, Statistics Specialist, Oman Medical Specialty Board for his support.
references
1. Schünemann HJ, Cushman M, Burnett AE, Kahn SR, Beyer-Westendorf J, Spencer FA, et al. American society of hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv 2018 Nov;2(22):3198-3225.
2. Raskob E; ISTH Steering Committee for World Thrombosis Day. Venous thromboembolism: a call for risk assessment in all hospitalised patients. Thromb Haemost 2016 Oct;116(5):777-779.
3. Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B, et al; ENDORSE Investigators. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 2008 Feb;371(9610):387-394.
4. Qaseem A, Chou R, Humphrey LL, Starkey M, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2011 Nov;155(9):625-632.
5. Anderson FA Jr, Goldhaber SZ, Tapson VF, Bergmann JF, Kakkar AK, Deslandes B, et al; ENDORSE Investigators. Improving practices in US hospitals to prevent venous thromboembolism: lessons from ENDORSE. Am J Med 2010 Dec;123(12):1099-1106.e8.
6. Alsayegh F, Kamaliddin H, Sheshah E, Bukhamseen N, Alkhuwaitir T, Elhoufi A. Assessment of venous thromboembolism risk and adequacy of prophylaxis in selected acute care medical centres in Arabian Gulf States: results from the ENDORSE study. Med Princ Pract 2012;21(6):522-528.
7. Rocher WD, Page T, Rocher M, Nel D. Venous thromboembolism risk and prophylaxis prescription in surgical patients at a tertiary hospital in Eastern Cape Province, South Africa. S Afr Med J 2019 Feb;109(3):178-181.
8. National Institute for Health and Care Excellence. Venous thromboembolism in adults. 2021 [cited 2023 May 14]. Available from: https://www.nice.org.uk/guidance/qs201.
9. Hecht JP, Han EJ, Cain-Nielsen AH, Scott JW, Hemmila MR, Wahl WL. Association of timing of initiation of pharmacologic venous thromboembolism prophylaxis with outcomes in trauma patients. J Trauma Acute Care Surg 2021 Jan;90(1):54-63.
10. Sahle BW, Pilcher D, Peter K, McFadyen JD, Litton E, Bucknall T. Mortality data from omission of early thromboprophylaxis in critically ill patients highlights the importance of an individualised diagnosis-related approach. Thromb J 2023 May;21(1):59.
11. Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of chest physicians evidence-based clinical practice guidelines. Chest 2012 Feb;141(2)(Suppl):e195S-e226S.
12. Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, et al. Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of chest physicians evidence-based clinical practice guidelines. Chest 2012 Feb;141(2)(Suppl):e227S-e277S.
13. Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of chest physicians evidence-based clinical practice guidelines. Chest 2012 Feb;141(2)(Suppl):e278S-e325S.