Pelvic organ prolapse (POP) is a prolapse of one or more of the anterior or posterior vaginal walls, uterus (cervix), or vaginal vault (after hysterectomy). It is a common clinical condition prevalent in 40% of women aged over 45 and in 50% of parous women.1 Cervical elongation is clinically defined as the presence of cervical length > 3.38 cm or a cervix-to-corpus ratio > 0.79.2
Cervical elongation that accompanies uterine prolapse is associated with a greater likelihood of prolapse recurrence after uterine-sparing surgeries such as hysteropexy.3 Performing a vaginal hysterectomy in such conditions is associated with increased operative time, procedural difficulties, and potential complications.4 Compared to cervical amputation, transvaginal hysterectomy has a significantly higher rate of severe complications, viz., intra-abdominal bleeding, severe intra-abdominal infection, ureteric injuries, bowel injuries, myocardial infarction, and severe anesthesia-related complications.5
We present this successful case management to share our experience in the classical surgical management of uterine prolapse accompanied by cervical elongation. Each step is illustrated to emphasize the importance of understanding each and the necessity of patience through this relatively long procedure.
Case Report
A 42-year-old woman was referred to our urogynecology clinic with the main complaint of a protruding mass coming out of her vagina since one year, which became worse with Valsalva. She had a history of tubectomy. No urinary or defecation complaint was reported.
Physical examination revealed a mass that protruded outside the hymen, uterine sondage was 10 cm, levator ani muscle tone and anal sphincter tone score was 3, with negative results in cough test, prolapse reduction test, and urinary residual test. The POP quantification measurement, as shown in Figure 1 and Table 1, corresponded to stage 3 uterine prolapse, stage 2 cystocele, stage 2 rectocele, and cervical elongation.
 Figure 1: Pelvic organ prolapse quantification examination.
Figure 1: Pelvic organ prolapse quantification examination.
Table 1: Pelvic organ prolapse quantification results.
|
Anterior wall +2
|
Genital hiatus 6
|
|
Posterior wall +2
|
|
Anterior wall +3
|
Perineal body 2
|
|
Posterior wall +2
|
|
Total vaginal length 9
|
Transvaginal ultrasound revealed anteflexed uterus size of 10.0 × 4.12 × 3.75 cm with a cervical length of 5.7 cm regular endometrium and endometrial thickness of 8.5 mm, and no adnexal mass [Figure 2].
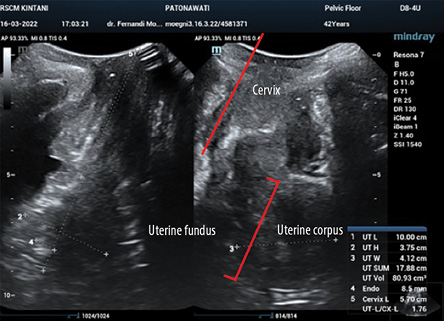 Figure 2: Cervical length examination using transvaginal ultrasound.
Figure 2: Cervical length examination using transvaginal ultrasound.
Total vaginal hysterectomy, bilateral salpingectomy, anterior colporrhaphy, colpoperineorrhaphy, and uterosacral ligament suspension were performed by an experienced urogynecologist. The procedure was performed in three hours. The surgical steps were as follows:
- Uterine exteriorization: epinephrine solution infiltration to vaginal mucosa performed and continued by hydrodissection of anterior, lateral, and posterior vaginal mucosa [Figure 3a].

 Figure 3: (a-n) All the steps of the total vaginal hysterectomy procedure with bilateral salpingectomy, anterior colporrhaphy, colpoperineorrhaphy, and uterosacral ligament suspension. (o) Postoperative condition.
Figure 3: (a-n) All the steps of the total vaginal hysterectomy procedure with bilateral salpingectomy, anterior colporrhaphy, colpoperineorrhaphy, and uterosacral ligament suspension. (o) Postoperative condition.
- Diamond incision made on vaginal mucosa around cervix [Figure 3b].
- Vaginal mucosa dissected and peeled off, and the bladder shifted cranially [Figure 3c].
- Posterior pouch of Douglas and vesicouterine fold opened [Figure 3d].
- Bilateral complex uterosacral cardinal ligaments were clamped, cut, and sutured [Figure 3e].
- Bilateral uterine vessels were clamped, cut, and sutured [Figure 3f].
- Bilateral round ligaments, proximal fallopian tubes, and utero-ovarian ligaments were clamped, cut, and sutured [Figure 3g].
- Bilateral salpingectomy was performed
[Figure 3h].
- Peritoneum closure [Figure 3i].
- Dissection of pubocervical fascia until it separates from vaginal mucosa [Figure 3j].
- Suturing of pubocervical fascia (multiple interrupted mattress sutures) [Figure 3k].
- Uterosacral ligament suspension on vaginal vault [Figure 3l].
- Hydrodissection of posterior vaginal mucosa continued by V-shaped incision of posterior vaginal mucosa [Figure 3m].
- Rectovaginal fascial plication [Figure 3n].
- Closure of anterior to posterior vaginal mucosa [Figure 3o].
After an uneventful recovery period, the patient was discharged on the second day post-operation in satisfactory condition. The histopathology report showed no signs of uterine pathology. At the follow-up three months later, she was free of complaints.
Discussion
We presented an illustrated case of step-by-step classical vaginal hysterectomy management in a 42-year-old woman with POP with cervical elongation. Uterine preservation was not a priority for the current patient, but where it is, the preferred option is Hedge’s modification of Fothergill surgery, reported to have a high degree of satisfaction and a low morbidity rate.6 A study in 2019 that compared Manchester surgery and vaginal hysterectomy for similar cases reported that the recurrence rates of POP and complication rates between the two groups were not statistically significant, but that the Manchester procedure time was shorter than vaginal hysterectomy.7
Hysteropexy is contraindicated in cases of uterine prolapse with cervical elongation because of its high rate of prolapse recurrence.3,4,8 Compared to hysterectomy, hysteropexy is associated with less blood loss, shorter operating time, and faster return to work. Other advantages of hysteropexy include fertility sparing and natural timing of menopause. The main disadvantages of hysteropexy are long-term prolapse repair outcomes and the need to continue surveillance for gynecological cancers.8
In women with no fertility desire (as in our patient), vaginal hysterectomy should be preferred to the uterine-sparing procedures mentioned above. Furthermore, total vaginal hysterectomy is preferred over a uterine-sparing technique or a supracervical hysterectomy where cervical elongation (as in the present case) is a factor.5
Vaginal hysterectomy in cases with cervical elongation requires a longer operating time. There is also difficulty in anterior and posterior colpotomy steps due to the greater number of clamps required to be applied to the sacrouterine and cardinal ligaments [Figure 3 e-g].9
The surgical steps we performed were consistent with those of classical vaginal hysterectomy, with the addition of strategies from the laparoscopic approach.10,11 First, continue to completely excise the vaginal attachments to the cervix. This will allow the uterus to descend into the operative field and improve exposure/visualization. Second, as the cardinal ligament is reached, separate the leaves of the broad ligament to visualize the uterine vessels; isolate the descending uterine branches at the three and nine o’clock positions. Third, continue to secure the uterine vessels laterally until the lower uterine segment is reached. Fourth, once the ascending branches of the uterine artery are isolated, the vesicouterine peritoneal fold can be approached from lateral to medial, and anterior entry can be accomplished.10
To prevent future vaginal vault prolapse, we performed uterosacral ligament suspension and colpoperineorrhaphy. Vaginal vault prolapse is a common disorder,12 particularly when there is pre-existing pelvic floor defect.13 Suspension of the vaginal apex to the uterosacral ligaments (McCall culdoplasty) or to the sacrospinous ligaments at the time of vaginal hysterectomy is the main choice for the prevention of vaginal vault prolapse.12 The overall prolapse recurrence in any vaginal compartment after a total hysterectomy with concurrent uterosacral ligament suspension has been estimated at 20%, with a 10% risk of recurrent surgery.14
Conclusion
Managing POP accompanied by cervical elongation is challenging since uterine preservative surgery has a high risk of prolapse recurrence, and increased operative time for vaginal hysterectomy. The choice of surgical method is determined by factors such as the patient’s desire for fertility preservation, the risk of bleeding, the length of the cervix, and prolapse recurrence risk. Classical vaginal hysterectomy steps can be performed safely without complications in cases of cervical elongation and POP with patience in each step.
Disclosure
The authors declared no conflicts of interest. Informed consent was obtained from the patient.
references
- 1. Vitale SG, La Rosa VL, Rapisarda AM, Laganà AS. The importance of a multidisciplinary approach or women with pelvic organ prolapse and cystocele. Oman Med J 2017 May;32(3):263-264.
- 2. Chavali K, Hiremath AC, Ramamurthy C. Hegde’s modification of fothergill surgery for cervical elongation: a 7-year retrospective review. J Obstet Gynaecol Can 2021 Mar;43(3):300-305.
- 4. Hyakutake MT, Cundiff GW, Geoffrion R. Cervical elongation following sacrospinous hysteropexy: a case series. Int Urogynecol J 2014 Jun;25(6):851-854.
- 5. Geoffrion R, Hyakutake MT, Koenig NA, Lee T, Cundiff GW. Bilateral sacrospinous vault fixation with tailored synthetic mesh arms: clinical outcomes at one year. J Obstet Gynaecol Can 2015 Feb;37(2):129-137.
- 6. Berger MB, Ramanah R, Guire KE, DeLancey JO. Is cervical elongation associated with pelvic organ prolapse? Int Urogynecol J 2012 Aug;23(8):1095-1103.
- 3. Ayhan A, Esin S, Guven S, Salman C, Ozyuncu O. The Manchester operation for uterine prolapse. Int J Gynaecol Obstet 2006 Mar;92(3):228-233.
- 7. Park YJ, Kong MK, Lee J, Kim EH, Bai SW. Manchester operation: an effective treatment for uterine prolapse caused by true cervical elongation. Yonsei Med J 2019 Nov;60(11):1074-1080.
- 8. Bergman I, Söderberg MW, Kjaeldgaard A, Ek M. Cervical amputation versus vaginal hysterectomy: a population-based register study. Int Urogynecol J 2017 Feb;28(2):257-266.
- 9. Alay I, Kaya C, Karaca I, Yildiz S, Cengiz H, Ekin M, et al. Diagnostic value of preoperative ultrasonography, cervical length measurement, and POP-Q examination in cervical elongation estimation. Int Urogynecol J 2020 Dec;31(12):2617-2623.
- 10. Messingschlager C, Orlando MS, Russo ML, Kho R. Surgical principles of vaginal hysterectomy with cervical elongation. Am J Obstet Gynecol 2021;226(3):S1369.
- 11. Pillarisetty LS, Mahdy H. Vaginal hysterectomy. InStatPearls; 2021.
- 12. Segev Y, Auslander R, Lavie O, Lissak A, Abramov Y. [Post hysterectomy vaginal vault prolapse: diagnosis prevention and treatment]. Harefuah 2008 May;147(5):406-412.
- 13. Uzoma A, Farag KA. Vaginal vault prolapse. Obstet Gynecol Int 2009;2009:275621.
- 14. Rappa C, Saccone G. Recurrence of vaginal prolapse after total vaginal hysterectomy with concurrent vaginal uterosacral ligament suspension: comparison between normal-weight and overweight women. Am J Obstet Gynecol 2016 Nov;215(5):601.e1-601.e4.