A four-month-old male infant was brought to the outpatient department of our tertiary care hospital with swelling in the right foot, which was noticed since the day of birth. The swelling increased in size and had bled profusely a month earlier,
which was managed with compression. On examination, a 7.2 × 7.8 cm, single non-pulsatile, well-defined reddish-purple lobulated mass was noted in the distal half of the right foot, involving the plantar side of the forefoot and mid-foot. There was a healed ulcer on the ventral aspect of the lesion. The third, fourth, and fifth toes were engulfed by the mass [Figure 1]. The mass had a variegated consistency, firm in some areas and hard in the rest. Blood investigations including hemoglobin and platelet count, yielded normal results.
 Figure 1: Reddish-purple mass in the distal half of the right foot.
Figure 1: Reddish-purple mass in the distal half of the right foot.
A plain X-ray of the foot suggested a soft tissue swelling with a few subtle radio opacities within the lesion suggestive of phleboliths [Figure 2]. Doppler ultrasound revealed multiple arterial channels with high flows and dilated venous channels. Contrast-enhanced magnetic resonance imaging showed a highly vascular mass in the right forefoot encasing the fourth toe, extending to third, fourth, and fifth web spaces and third and fourth metatarsal heads, along with the respective proximal phalanges [Figure 3].
Early arterial enhancement was noted.
 Figure 2: X-ray of the foot showing the shadow of the lesions. Note the splayed digits and subtle phleboliths in the distal foot.
Figure 2: X-ray of the foot showing the shadow of the lesions. Note the splayed digits and subtle phleboliths in the distal foot.
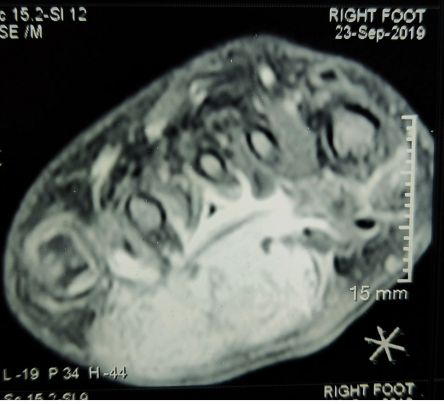 Figure 3: Contrast-enhanced MRI showing the mass in the right forefoot extending dorsally to the web spaces and metatarsal heads.
Figure 3: Contrast-enhanced MRI showing the mass in the right forefoot extending dorsally to the web spaces and metatarsal heads.
Question
What is the most likely diagnosis?
a. Benign vascular lesion.
b. Congenital infantile fibrosarcoma.
c. Infantile myofibroma.
d. Spindle cell rhabdomyosarcoma.
Answer
b. Congenital infantile fibrosarcoma.
Discussion
An excisional biopsy in the form of partial forefoot amputation was performed and the wound was covered with a split-thickness skin graft. On gross sectioning, a pale grey lesion was noted with focal areas of the hemorrhage. Histological examination revealed a cellular mass composed of sheets of monomorphic spindle cells with nuclei showing plump oval to short-spindled appearance, arranged in the form of vague bundles [Figure 4 a and b]. The focal areas were showing a few lymphocytes admixed with scattered interspersed thin-walled blood vessels. Mitotic figures with minimal pleomorphism were identified [Figure 4c]. The cells were found to be immunoreactive for vimentin [Figure 4d] and negative for cytokeratin, epithelial membrane antigen, S100, desmin, myogenin, and myoD1. A diagnosis of congenital infantile fibrosarcoma (CIF) was made. After ruling out regional and distant metastasis, a below-knee amputation was done to achieve surgically clear margins. The child was disease-free at the four years follow-up.
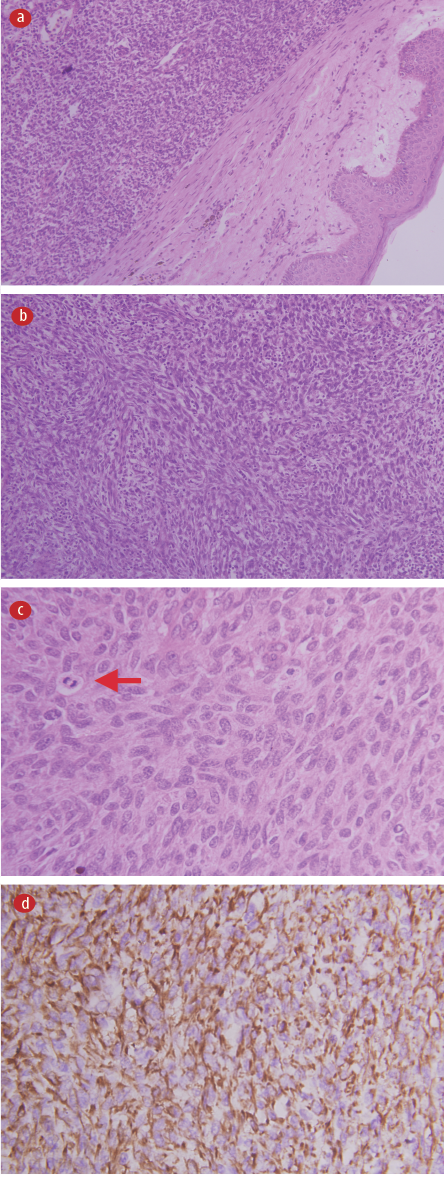 Figure 4: Hemoxylin and eosin stain. (a) Photomicrograph showing monomorphic cellular mass with multiple vascular spaces in the dermis, magnification = 40 ×. (b) Sheets of monomorphic plump spindle cells to oval short-spindled nuclei, arranged in the form of vague bundles with few infiltrating lymphocytes, magnification = 100 ×. (c) Mitosis (red arrow), magnification = 400 ×. (d) Vimentin showing cytoplasmic positivity, magnification = 100 ×.
Figure 4: Hemoxylin and eosin stain. (a) Photomicrograph showing monomorphic cellular mass with multiple vascular spaces in the dermis, magnification = 40 ×. (b) Sheets of monomorphic plump spindle cells to oval short-spindled nuclei, arranged in the form of vague bundles with few infiltrating lymphocytes, magnification = 100 ×. (c) Mitosis (red arrow), magnification = 400 ×. (d) Vimentin showing cytoplasmic positivity, magnification = 100 ×.
Although CIF is rare, it is one of the commonest soft tissue sarcomas in infants.1 The distal extremities are the most frequent site of its occurrence, which is also associated with a lesser risk of metastasis and mortality compared to its occurrence at axial sites such as the head and neck or trunk.2,3 More than a third of affected infants present the symptoms at birth and most of the rest develop them during the first year of life.
The high degree of vascularity, erythematous-purple color, bleeding episodes, and presentation in early infancy may lead to misdiagnosing CIF cases as vascular lesions, both clinically and radiologically, thus delaying the diagnosis and treatment.4,5 Spindle cell rhabdomyosarcoma is another differential diagnosis, but it presents in older children around seven years of age, usually in the paratesticular region and the head and neck. Immunoreactivity to desmin and myogenin clinches the diagnosis. Infantile myofibroma has a similar age of presentation as CIF, which may occur as well-circumscribed solitary or multi-centric masses usually in the head, neck, and trunk regions. However, it is composed of mature spindle cells in a whorled pattern and small immature round mesenchymal cells within a central vascular area.4 Further, these cells are immunoreactive to desmin, vimentin, and smooth muscle actin, thus differentiating it from CIF.
The presence of chromosomal translocation t(12;15) (p13;q25) for an ETV6-NTRK3 fusion gene is specific for CIF.2 In case of a dilemma despite histopathological examination, fluorescent in-situ hybridization to detect the translocation can be conducted for confirmation.
While the first line of treatment is wide local excision of the tumor (often leading to amputations of the distal limbs), neoadjuvant chemotherapy is often used to limit the extent of major disfiguring or debilitating surgery in the head and neck or trunk regions.1,2,5
The obstacle to the management of CIF is that it is easily confused with other benign conditions, thus delaying the diagnosis and treatment. Pediatricians and general practitioners have a crucial role to play in advising biopsy for suspicious soft tissue masses in newborns and neonates.
Disclosure
The authors declared no conflicts of interest. Informed consent was obtained from the patient’s father.
references
- 1. Parida L, Fernandez-Pineda I, Uffman JK, Davidoff AM, Krasin MJ, Pappo A, et al. Clinical management of infantile fibrosarcoma: a retrospective single-institution review. Pediatr Surg Int 2013 Jul;29(7):703-708.
- 2. Tsang HH, Dolman PJ, Courtemanche DJ, Rassekh SR, Senger C, Lyons CJ. Prenatal presentation of fronto-orbital congenital infantile fibrosarcoma: a clinicopathologic report. JAMA Ophthalmol 2013 Jul;131(7):965-967.
- 3. Huang JT, Huang JT, Dillon BJ, Gellis SE, Liang MG. Picture of the month: diagnosis: infantile fibrosarcoma. Arch Pediatr Adolesc Med 2012 Sep;166(9):864.
- 4. Enos T, Hosler GA, Uddin N, Mir A. Congenital infantile fibrosarcoma mimicking a cutaneous vascular lesion: a case report and review of the literature. J Cutan Pathol 2017 Feb;44(2):193-200.
- 5. Hu Z, Chou PM, Jennings LJ, Arva NC. Infantile fibrosarcoma-a clinical and histologic mimicker of vascular malformations: case report and review of the literature. Pediatr Dev Pathol 2013;16(5):357-363.