A 32-year-old woman presented to the ear, nose, and throat clinic with a two-month history of nasal bleeding and discharge from the left nostril. Her past medical history was unremarkable, and she was not taking any regular medications. On examination, she was afebrile and maintained normal saturation in room air, with heart rate and blood pressure within normal limits. There was no evidence of diplopia or facial tenderness. Nasal endoscopic examinations showed a large polypoidal, rubbery-looking lesion filling the left nasal cavity and bulging from the left maxillary sinus through the ostiomeatal complex and extending posteriorly to the posterior choanae, with mild septum deviation [Figure 1]. The rest of the nasal examination was unremarkable. Computed tomography (CT) of the paranasal sinuses showed a hyperdense lesion in the left maxillary sinus extending to the left nasal cavity [Figure 2 a-c]. The lesion was associated with bone remodeling with expansion and bone thinning but without aggressive bone changes. Magnetic resonance imaging (MRI) showed the lesion as lobular in shape with a T2-hypointense rim. The lesion was T1 hypointense with mild internal hyperintensity and showed intense centrilobular enhancement [Figure 2 d-f].
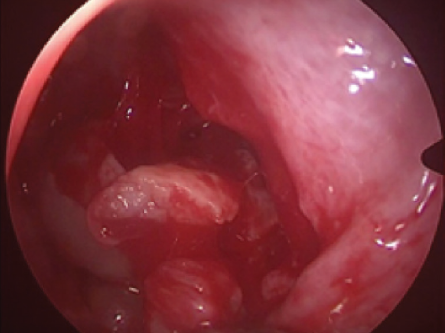 Figure 1: Endoscopic view showing a mass filling the left nasal cavity bulging through the ostiomeatal complex and extending to the posterior choanae and the edge of the biopsy area.
Figure 1: Endoscopic view showing a mass filling the left nasal cavity bulging through the ostiomeatal complex and extending to the posterior choanae and the edge of the biopsy area.
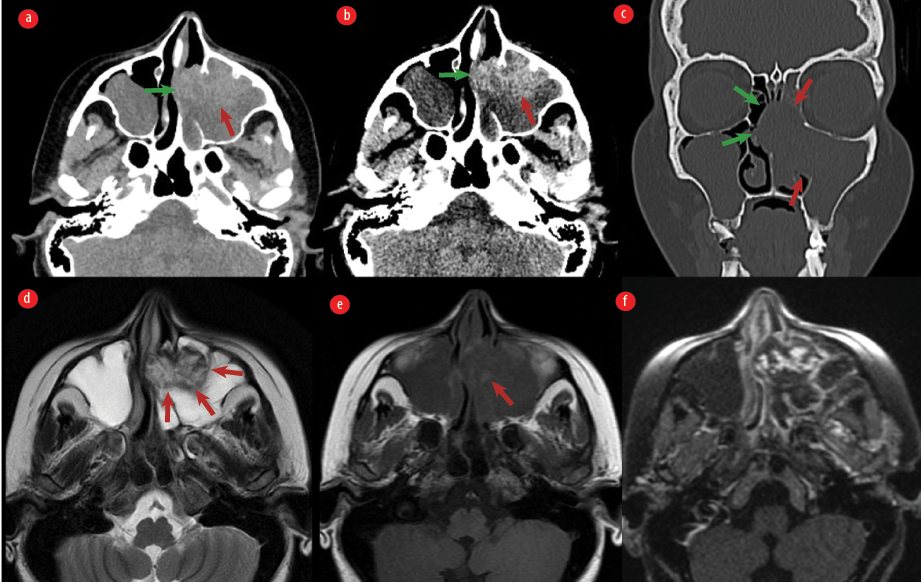 Figure 2: (a and b) Non-enhanced axial CT images of the paranasal sinuses showing a lesion in the anterior aspect of the left maxillary sinus (red arrow) extending to the left nasal cavity (green arrow). (b) The lesion is hyperdense which is accentuated using a narrow window in the image. (c) Coronal CT image with bone algorithm demonstrating bone expansion and remodeling (red arrows) with expansion and right-sided deviations of the nasal septum (green arrows). (d) Axial T2-weighted image showing the lobulated shape of the lesion with hypointense rim (red arrows) and internal heterogeneity. (e) T1-weighted image showing that the lesion is hypointense with areas of intrinsic T1 hyperintensity (red arrow). (f) Post-contrast image demonstrating internal avid lobular enhancement. The images also showed features of left maxillary obstructive sinusitis due to the lesion. An incidental retention cyst in the right maxillary sinus was seen.
Figure 2: (a and b) Non-enhanced axial CT images of the paranasal sinuses showing a lesion in the anterior aspect of the left maxillary sinus (red arrow) extending to the left nasal cavity (green arrow). (b) The lesion is hyperdense which is accentuated using a narrow window in the image. (c) Coronal CT image with bone algorithm demonstrating bone expansion and remodeling (red arrows) with expansion and right-sided deviations of the nasal septum (green arrows). (d) Axial T2-weighted image showing the lobulated shape of the lesion with hypointense rim (red arrows) and internal heterogeneity. (e) T1-weighted image showing that the lesion is hypointense with areas of intrinsic T1 hyperintensity (red arrow). (f) Post-contrast image demonstrating internal avid lobular enhancement. The images also showed features of left maxillary obstructive sinusitis due to the lesion. An incidental retention cyst in the right maxillary sinus was seen.
Question
What is the most likely diagnosis?
a. Inverted papilloma.
b. Mycetoma.
c. Sinonasal angiomatous polyp.
d. Hematoma.
e. Melanoma.
Answer
c. Sinonasal angiomatous polyp.
Discussion
The patient underwent right-side endoscopic sinus surgery for surgical resection of the lesion and type III endoscopic medial maxillectomy [Figure 3].
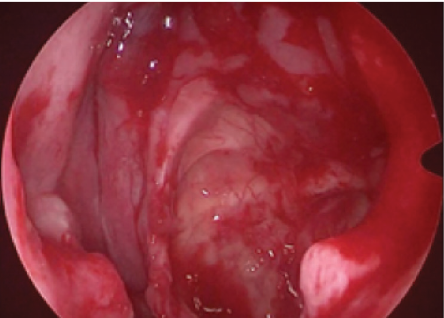 Figure 3: Endoscopic view of the left nasal cavity after the mass resection and medial maxillectomy type III.
Figure 3: Endoscopic view of the left nasal cavity after the mass resection and medial maxillectomy type III.
Histological examination of the tissue confirmed the diagnosis of sinonasal angiomatous polyp (SAP) with evidence of congested and dilated ectatic vessels, occasional areas showing thick blood vessels with luminal thrombosis, and those vessels were lined by endothelial cells, some of which displayed nuclear atypia under high power magnification [Figure 4].
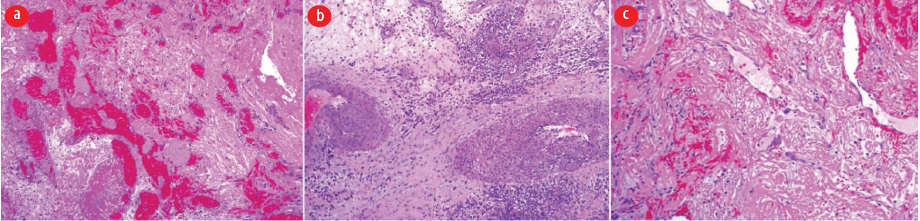 Figure 4: (a) Hematoxylin and eosin (H&E)-stained slide showing numerous dilated and constricted blood vessels, magnification = 10 ×. (b) H&E-stained slide showing thick-walled blood vessels with thrombosis, magnification = 10 ×. (c) H&E-stained section showing a blood vessel lined by endothelial cells showing nuclear atypia, magnification = 40 ×.
Figure 4: (a) Hematoxylin and eosin (H&E)-stained slide showing numerous dilated and constricted blood vessels, magnification = 10 ×. (b) H&E-stained slide showing thick-walled blood vessels with thrombosis, magnification = 10 ×. (c) H&E-stained section showing a blood vessel lined by endothelial cells showing nuclear atypia, magnification = 40 ×.
Sinonasal polyps can be classified histologically into five different groups: edematous, glandular, fibrous, cystic, and angiomatous. SAPs are relatively rare and account for 5% of sinonasal polyps.1
Various terms such as cavernous hemangioma, hemangioma, organized hematoma, and angiectatic/angiomatous polyp, have been used to describe SAPs in the literature.
The most common symptoms of SAP are nasal obstruction and epistaxis, and they occur in a wide age range without predominance of either sex.2,3 Sinonasal endoscopy may reveal a polypoidal mass originating from the maxillary sinus blocking the ostiomeatal complex with reddish areas and necrosis, and it typically bleeds on touching and can extend posteriorly to the choanae or nasopharynx.2,4
On CT, SAPs are heterogeneous, with areas of relatively high density, although calcifications are rare.5 The enhancement is heterogenous.3,5 The presence of bone changes is a characteristic feature of SAPs, which can manifest as bone remodeling, expansion, erosions, and destruction.5 Hyperostosis is a feature related to chronic sinusitis due to the obstruction of the maxillary sinus by SAPs.5
Magnetic resonance imaging (MRI) typically shows a circumscribed lesion with bone thinning. SAPs are usually T1 hypointense, with some cases showing T1 isointensity.2 Tam et al,4 on the other hand, described T1 hyperintensity as in our patient, which is likely related to the presence of internal hemorrhage. The lesions are classically T2 hyperintense with a hypointense rim, as seen in the present case as well.2,4 SAPs enhance avidly after contrast injection and show an internal enhancing nodular appearance.2,4 These lesions also show progressive enhancement in dynamic contrast-enhanced MRI.2
The histopathological hallmark of SAPs is extensive vascular proliferation and ectasia, with deposition of pseudo-amyloid and the presence of atypical stromal cells.1,6
Complete surgical resection with cauterization of the original attachment point is curative, and the risk of recurrence is low.2,5 The clinical and radiological features of SAPs can mimic other sinonasal pathologies.2,5,7 The differential includes other inflammatory sinonasal polyps, inverted papilloma, and mycetoma.2,5 Other rare sinonasal vascular lesions can mimic SAPs, like nasal lobular hemangioma.8 SAPs can also mimic malignant tumors like squamous cell carcinoma and melanoma when there is aggressive bone destruction.2
Recognizing this rare type of nasal polyp is essential, as surgical resection is curative. CT and MRI can be used to characterize the lesion, determine its extent, look for differentials, and assist in pre-operative planning.
Disclosure
The authors declared no conflicts of interest. The patient gave verbal consent for publication.
references
- 1. Yfantis HG, Drachenberg CB, Gray W, Papadimitriou JC. Angiectatic nasal polyps that clinically simulate a malignant process: report of 2 cases and review of the literature. Arch Pathol Lab Med 2000 Mar;124(3):406-410.
- 2. Wang YZ, Yang BT, Wang ZC, Song L, Xian JF. MR evaluation of sinonasal angiomatous polyp. AJNR Am J Neuroradiol 2012 Apr;33(4):767-772.
- 3. Kim HJ, Kim JH, Kim JH, Hwang EG. Bone erosion caused by sinonasal cavernous hemangioma: CT findings in two patients. AJNR Am J Neuroradiol 1995 May;16(5):1176-1178.
- 4. Tam YY, Wu CC, Lee TJ, Lin YY, Chen TD, Huang CC. The clinicopathological features of sinonasal angiomatous polyps. Int J Gen Med 2016 Jun;9:207-212.
- 5. Dai LB, Zhou SH, Ruan LX, Zheng ZJ. Correlation of computed tomography with pathological features in angiomatous nasal polyps. PLoS One 2012;7(12):e53306.
- 6. Purushothaman PK, Sharanya M, Manoj Pandian SP. Angiectatic sinonasal polyp: a diagnostic challenge. Indian J Otolaryngol Head Neck Surg 2021 Jun;73(2):260-262.
- 7. Shirazi N, Bist SS, Selvi TN, Harsh M. Spectrum of sinonasal tumors: a 10-year experience at a tertiary care Hospital in North India. Oman Med J 2015 Nov;30(6):435-440.
- 8. Al Washahi MK, Al Killidar A, Razek YA, Khamis T. Endonasal endoscopic complete excision of unilateral nasal hemangioma in a child: case report and technical note. Oman Med J 2019 Mar;34(2):156-159.