An apparently healthy 26-year-old woman presented with a two-year history of painless upper neck swelling. There were no obstructive or constitutional symptoms. She denied features of hypo or hyperthyroid states. She had no otologic or nasal features.
On examination, the patient was comfortable in room air. She had a blood pressure of 110/70 mmHg, pulse rate of 68 bpm, respiratory rate of 16, and she was afebrile. A 4 × 3 cm oval or multinodular firm, mobile (in all planes), non-tender infrahyoid midline mass, with normal overlying skin, was noted. The mass was well-encapsulated and not adherent to surrounding structures with no external skin changes. Baseline blood investigations and thyroid function tests were within the normal range. A flexible nasopharyngolaryngoscopy revealed mobile vocal cords with normal supraglottic structures.
Cervical ultrasonography revealed a fluid-filled mass with solid components. Additionally, bilateral thyroid glands were present. A computed tomography of the neck revealed a septated complex cystic mass arising from the floor of the mouth measuring 2.9 × 3.1 × 3.3 cm [Figures 1 and 2]. There was focal and nodular enhancement of the septa measuring about 0.6 cm, and the mass appeared to be continuous with the geniohyoid muscles. No cervical lymphadenopathy was noted.
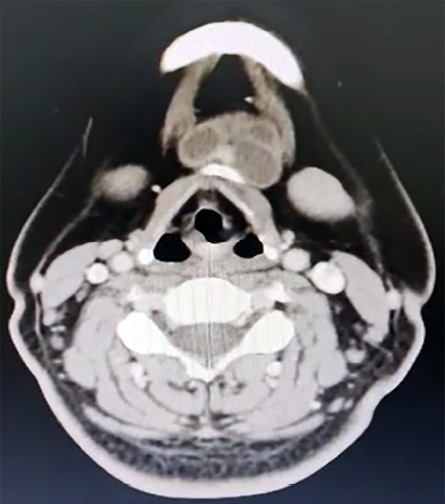 Figure 1: Axial view of CT showing a septated complex cystic mass arising from the floor of the mouth measuring 2.9 × 3.1 × 3.3 cm.
Figure 1: Axial view of CT showing a septated complex cystic mass arising from the floor of the mouth measuring 2.9 × 3.1 × 3.3 cm.
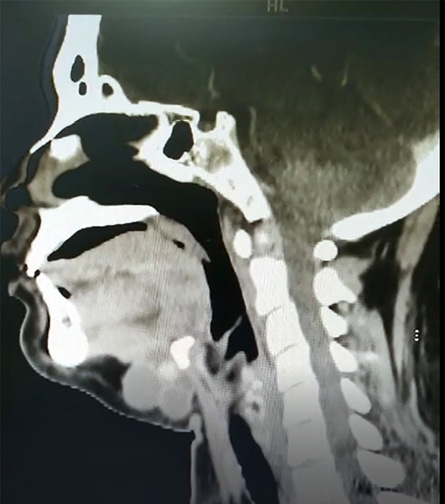 Figure 2: Sagittal view of CT showing a septated complex cystic mass arising from the floor of the mouth measuring 2.9 × 3.1 × 3.3 cm.
Figure 2: Sagittal view of CT showing a septated complex cystic mass arising from the floor of the mouth measuring 2.9 × 3.1 × 3.3 cm.
Question
- What is the diagnosis?
a. Thyroid cyst.
b. Thyroglossal duct cyst.
c. Thyroglossal duct carcinoma.
d. Extrapulmonary tuberculosis.
Answer
c. Thyroglossal duct carcinoma.
A preliminary diagnosis of thyroglossal duct cyst was made. The patient was counseled for a Sistrunk procedure. The surgery was successful, with clear margins and no lymphovascular invasion. There were no complications postoperatively, and the patient was discharged home on oral analgesia. The histopathological examination revealed papillary thyroid carcinoma (PTC) of the thyroglossal duct cyst.
Discussion
Thyroglossal duct cysts are remnants of the thyroglossal duct that failed to involute between the seventh and 10th weeks of gestation.1 These cysts can be found anywhere along the route of the thyroglossal duct and, depending on the rotation of the hyoid bone, can cause segmentation of the duct, whether in the pre-hyoid, transhyoid, or retrohyoid position.1 The thyroglossal duct can obliterate to form a fibrous cord or persist as a patent duct. A thyroglossal cyst is usually unilocular and can be isolated or associated with a duct or fibrous cord.1
Malignant thyroglossal cysts are rare.2 Most cases are diagnosed postoperatively, but a diagnosis of malignancy is possible with fine-needle aspiration cytology.3 We decided to proceed with the Sistrunk procedure as the mass appeared to be arising from the thyroglossal tract. It was reported that the majority of thyroglossal duct carcinomas are PTCs. There is a predilection for females, with a 3:1 female:male ratio,4 and a mean age at presentation of about 40 years.5 Our patient was a female in her 20s, with an age that is suggestive of thyroglossal duct cyst.
The patient is currently on a two-monthly follow-up with a six-monthly imaging follow-up. Options of total thyroidectomy and radioactive iodine are still being discussed.
Thyroglossal duct carcinoma typically presents as an asymptomatic midline neck swelling, as reported in our patient.5 Nonetheless, features such as rapid expansion, fixed cyst, and pain are telltale signs of malignancy of thyroglossal duct cyst. Rayess et al,5 reported that 73.3% of thyroglossal duct carcinoma are diagnosed incidentally, postoperatively.
The ideal investigation for thyroglossal duct carcinoma is still debatable, although most authors favor imaging, either a computed tomography scan or ultrasound.5 The role of fine-needle aspiration remains questionable due to its low sensitivity, which is attributed to the dilution of the aspirate with cystic fluid contents.5
It is worth noting that the presence of the thyroid gland must be confirmed before surgery. PTC of the thyroglossal duct may also occur as a primary entity due to ectopic thyroid gland tissue.
The Sistrunk procedure has been advocated by several authors as the majority of diagnoses are typically made postoperatively.5 In patients diagnosed postoperatively with thyroglossal duct carcinoma, whether a total thyroidectomy solely or followed by radioiodine ablation is required remains debatable. Some authors propose that patients younger than 45 years with no lymph node involvement, metastatic spread, radiation exposure, or suspicious imaging findings with negative margins do not require routine total thyroidectomy.6 All patients with thyroglossal duct carcinoma with no suspicious metastatic spread require annual imaging and blood investigations.
references
- 1. Amos J, Shermetaro C. Thyroglossal duct cyst. Treasure Island (FL): StatPearls Publishing; 2022.
- 2. Sturniolo G, Moleti M, Violi MA, Di Bella B, Presti S, Trimarchi F, et al. Prevalence of thyroglossal duct cyst carcinoma in adults having surgery for thyroglossal duct cysts. Thyroid 2012 Nov;22(11):1191-1192.
- 3. Heshmati HM, Fatourechi V, van Heerden JA, Hay ID, Goellner JR. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc 1997 Apr;72(4):315-319.
- 4. Thompson LD, Herrera HB, Lau SK. Thyroglossal duct cyst carcinomas: a clinicopathologic series of 22 cases with staging recommendations. Head Neck Pathol 2017 Jun;11(2):175-185.
- 5. Rayess HM, Monk I, Svider PF, Gupta A, Raza SN, Lin HS. Thyroglossal duct cyst carcinoma: a systematic review of clinical features and outcomes. Otolaryngol Head Neck Surg 2017 May;156(5):794-802.
- 6. Plaza CP, López ME, Carrasco CE, Meseguer LM, Perucho AdeL. Management of well-differentiated thyroglossal remnant thyroid carcinoma: time to close the debate? Report of five new cases and proposal of a definitive algorithm for treatment. Ann Surg Oncol 2006 May;13(5):745-752.