Cardiovascular diseases (CVDs) are the leading causes of mortality and morbidity in the world, accounting for almost 18 million deaths representing 31% of global deaths. Heart attack and stroke accounts for 85% of these deaths.1 Coronary atherosclerosis and resulting first episodes of potentially lethal or disabling myocardial infarction events often strike apparently healthy asymptomatic individuals. Therefore, there is a great interest in routine screening, early detection, and primary prevention. Lifestyle modification and pharmacotherapy can lower the incidence of acute events in susceptible individuals. Statins are the main cholesterol-lowering drugs used for primary prevention of CVDs.2 Traditionally, coronary heart disease (CHD) risk is predicted by calculating the risk factor-based score, like Framingham Risk Score (FRS), which focuses on factors like age, sex, smoking, blood pressure, serum cholesterol level, and diabetes. However, there is growing evidence that including coronary artery calcium (CAC) in estimating CHD risk has a significant effect on treatment decisions. Therefore, the first part of the review evaluates the contribution of CAC scoring to a traditional 10-year CHD risk prediction scores.
Coronary arteries are the vessels that supply oxygen-rich blood and nutrients to the heart. Anatomical changes such as narrowing of coronary arteries due to deposition of calcium and other substances like cholesterol obstruct supply of oxygenated blood and nutrients thus causing CHD.3 Fractional flow reserve of a coronary artery in comparison to a hypothetical 100% normal coronary artery reveals the functional/physiological status of a coronary artery after variable calcium and/or cholesterol deposits. A CAC score provides an estimate of the burden of coronary atherosclerosis; hence, it is used for CHD risk stratification.4 To obtain the score, a non-contrast gated cardiac computed tomography (CT) scan is conducted, and areas with calcium are identified and quantified.
Figure 1 shows the CT of the chest with identified calcification which is used to calculate CAC score.5 The score produced may be an Agatston score (reflects the total area of calcium deposits along with the density of calcium), calcium volume score, or relative calcium mass score depending on the method.6 Commonly, CAC scoring requires manual identification of the areas that represent calcification; however, artificial intelligence (AI) enables clinicians to perform multiple tasks like processing on different atlases at the same time with more accuracy and least human error.
 Figure 1: Coronary artery calcification detection on CT pulmonary venograms. (a) Mild coronary calcification is seen as a spot of calcification in the proximal left anterior descending artery. (b) Moderate coronary calcification is seen as a bulky calcification in the proximal part of the left anterior descending artery. Another area of calcification is seen in the proximal part of the left circumflex artery. (c) Severe coronary calcification is seen as a very dense and long segment of the proximal and mid-portion of the left anterior descending artery. Additional coronary calcification is seen involving the left main coronary artery.
Figure 1: Coronary artery calcification detection on CT pulmonary venograms. (a) Mild coronary calcification is seen as a spot of calcification in the proximal left anterior descending artery. (b) Moderate coronary calcification is seen as a bulky calcification in the proximal part of the left anterior descending artery. Another area of calcification is seen in the proximal part of the left circumflex artery. (c) Severe coronary calcification is seen as a very dense and long segment of the proximal and mid-portion of the left anterior descending artery. Additional coronary calcification is seen involving the left main coronary artery.
The second part of the review summarizes methods developed to automate CAC scoring with AI.
Contribution of CAC scoring to traditional 10-year CHD risk prediction scores
CAC has been studied since the 1980s, and several studies have shown that it is effective in estimating CHD risk and is accurate for risk stratification.7–12 CAC scoring prevents overtreatment with lipid lowering drugs.13 Individuals with higher CAC and low-risk factor scores have higher mortality rate than those with low CAC and high-risk factor scores.11,14
The Multi-Ethnic Study of Atherosclerosis (MESA) risk scoring algorithm was developed to study the prevalence of risk factors and progression of subclinical CVDs among multiethnic population. Inclusion of CAC with traditional risk factors in MESA score improves the risk prediction by up to 80%.10 Others, compared MESA-CAC risk score with Reynolds Risk Score and atherosclerotic cardiovascular disease Risk calculator.4 Reynolds Risk Score overestimated the risk prediction for 30% of participants while atherosclerotic cardiovascular disease underestimated the risk for 23% suggesting that inclusion of CAC scores provides more accurate risk stratification.
Use of AI to automate CAC scoring on chest CTs
AI strives to develop mathematical models and algorithms that aim to mimic human intelligence to solve challenging problems. Artificial neural networks, inspired by the biological neural networks in human brains are one of the most influential technologies used to achieve this goal. Each artificial neuron can use its connections to receive and transmit signals to other neurons.
Neural networks have an input and output layer, which may have intermediate layers with connected neurons known as hidden layers. A neural network with multiple hidden layers is called a deep neural network. Whereas a convolutional neural network (CNN, or ConvNet) is a type of deep neural network, frequently used to process images from different domains.
Chest CT scans are often used for routine screening, for example in heavy smokers to detect lung cancer. With AI, information about the cardiovascular system (e.g., through CAC scoring) can easily be obtained at the same time. This is of importance as lung disease patients are also at risk for CVDs.15 Hence, several methods have been developed to automate CAC scoring from chest CT scans. The reviewed methods and their accuracy are summarized in Table 1.
Table 1: Summary of automated coronary artery calcium (CAC) scoring methods and accuracy.
|
Išgum et al,16 2012
|
Probabilistic coronary calcium map and statistical pattern recognition system
|
79% for CAC volume
82% for Agatston risk groups
|
|
Gonzalez et al,15 2016
|
Connected component analysis
|
86% for Agatston scores
|
|
Singh et al,17 2018
|
Convolutional neural network (CNN)
|
93% for Agatston scores
|
|
Sandstedt et al,18 2019
|
Artificial intelligence-based automatic post-processing software
|
93% for Agatston score, volume score, and mass score
|
|
De Vos et al,19 2019
|
3D image registration with CNN
|
93% for CAC
|
|
Fischer et al,20 2020
|
CNN with Long Short-Term Memory
|
90.3% for CAC
|
|
Lee et al,21 2021
|
Semantic segmentation with deep learning
|
93% for CAC
|
|
Gogin et al,22 2021
|
Ensemble of 5 CNNs with 3D U-Net model
|
95.1% for CAC
|
In one study,16 a probabilistic coronary calcium map and statistical pattern recognition system to automate CAC scoring from chest CT scans. Location, texture, size, and shape features are used to represent CAC lesions. Location features were determined by registering an input image to an atlas image and by extracting the location features from a map of a priori spatial probabilities of CAC. Chest CT scans were registered to create a probability map. The detected CACs were used to obtain CAC volume scores and Agatston scores. Using 231 chest CT scans, the results showed 79% accuracy for CAC volume and 82% accuracy for classifying Agatston risk groups. The sensitivity of their method for CAC volume was 79.2% but only 58.6% sensitivity for Agatston risk groups.
Chest CT scans of 1500 patients were used to automate Agatston scoring.15 Firstly, bones were identified by connected component analysis so that they would not be misidentified as CACs. Secondly, a machine learning-based object detector was used to detect the heart by finding the pulmonary artery and the aorta from the image. Thirdly, the region of interest was defined around the heart. After this, calcified voxels were identified and grouped in connected components to compute Agatston scores [Figure 2]. The results showed 86% agreement with manual Agatston scores.
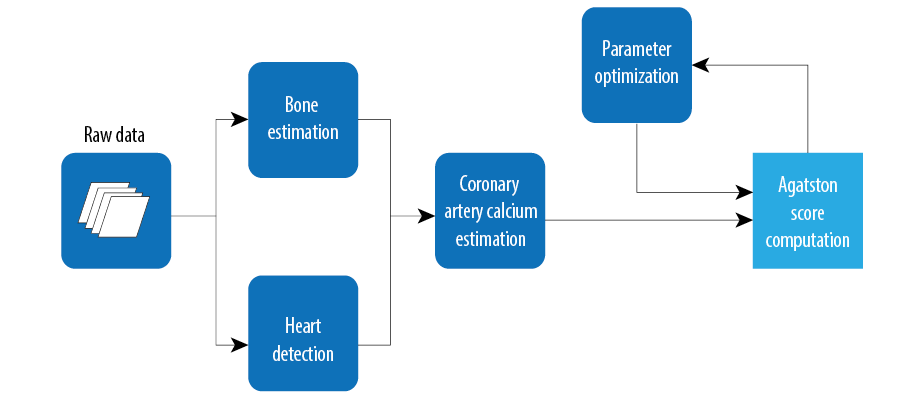 Figure 2: Computation flow for automating Agatston scoring.15
Figure 2: Computation flow for automating Agatston scoring.15
More recently, research has focused on the use of CNNs in the medical domain which were trained to obtain Agatston scores directly from chest CT scans [Figure 3].17 A database of 5973 chest CT scans with Agatston scores was used, of which 4973 scans were used for training and 1000 scans for testing. The results showed that CNN was able to predict Agatston scores from the test set with 93% accuracy.17
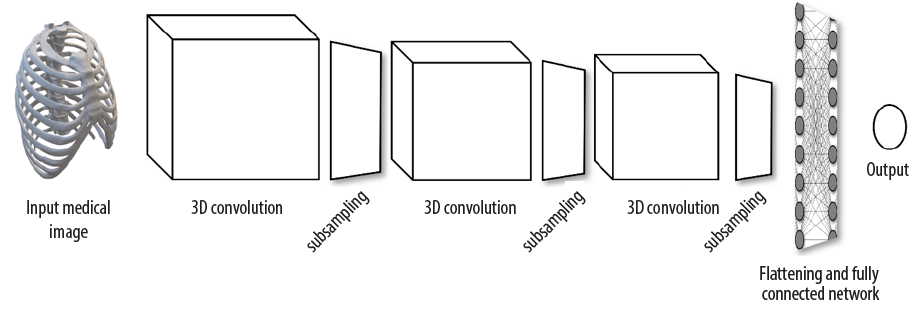 Figure 3: A typical architecture of a convolutional neural network used for medical image processing. Input medical 3D image goes through a series of convolution layers which extracts the convolutional features from previous layers and passes through the subsampling layer which reduces the size of convolutional layers. Flattening layer then converts the convolutional features to single dimension which is further connected to flattening layers via fully connected neurons. Output ( coronary artery calcium for instance) is then achieved in the output layer.17
Figure 3: A typical architecture of a convolutional neural network used for medical image processing. Input medical 3D image goes through a series of convolution layers which extracts the convolutional features from previous layers and passes through the subsampling layer which reduces the size of convolutional layers. Flattening layer then converts the convolutional features to single dimension which is further connected to flattening layers via fully connected neurons. Output ( coronary artery calcium for instance) is then achieved in the output layer.17
A study compared AI-based automatic post-processing software for automated CAC scoring and traditional semi-automatic CAC scoring that requires manual calcium identification.18 Three hundred and fifteen chest CT scans were used for both methods to determine Agatston score, the volume score, the mass score, and the number of calcified coronary lesions. The results showed that all outcomes between the automated and semi-automated methods were in ~93% correlation. Additionally, the median time for the automated method was 9 seconds and 59 seconds for the semi-automatic method. The study demonstrates that automatic CAC scoring is equally accurate to semi-automatic scoring and significantly faster.
CAC has higher attenuation differences between lesions. To address this, Lee et al,21 has used coronary CT angiography to generate labeled data. This dataset is used with CAC images for pixel level classification. Finally, the image details are fed into a software (AVIEW CAC, Coreline Soft, Co. Ltd., South Korea) that determines the CAC
score [Figure 4].21
 Figure 4: Labels from coronary CT angiography are transferred to coronary artery calcium (CAC) for registration purpose. These registered labels with CAC images are then forwarded to U-Net model.21
Figure 4: Labels from coronary CT angiography are transferred to coronary artery calcium (CAC) for registration purpose. These registered labels with CAC images are then forwarded to U-Net model.21
A study by de Vos et al,19 proposed a combination of two convolutional networks. One network is used for unsupervised atlas-registration and the second one is used for the calculation of calcium scoring [Figure 5]. Atlas registration CNN is used for image registration to align all the input images in the same 3D space or field of view. This is done by fixing the atlas image and warping the rest of the images available in the dataset by finding the transformation parameters and by interpolation. Calcium scoring CNN predicts the calcium scoring from the image slices.
 Figure 5: Image is first registered by Atlas registration Convolutional neural networks (ConvNet) to align the field of view (FOV) which is then fed to calcium scoring ConvNet to find the coronary artery calcium.19
Figure 5: Image is first registered by Atlas registration Convolutional neural networks (ConvNet) to align the field of view (FOV) which is then fed to calcium scoring ConvNet to find the coronary artery calcium.19
Fischer et al,20 proposed segmentation-based deep learning method (CNN and LSTM) for calcified scoring but this was only 90.3% accurate. Gogin et al,22 proposed an ensemble of five CNNs with 3D U-Net architecture. Each model is built with the depth of four levels having 16 initial filters. They used exponential linear unit as activation function. Residual connection is used in each convolutional layer with batch normalization. A final decision about the classification is made by the majority voting for each voxel (3D pixel) by all the five CNNs, and hence the CAC scoring is around 95% accurate. More recently, Zair et al,23 applied the preprocessing and extraction model prior to the segmentation of 3D heart. The whole process, as shown in Figure 6, estimates CAC score with an accuracy of 99%.

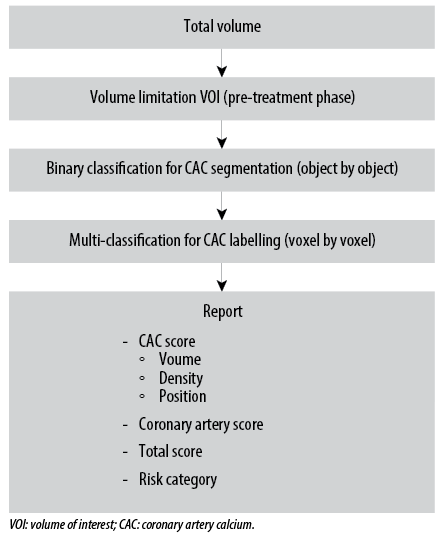 Figure 6: Pre-treatment phase - image volume is passed through preprocessing step in which Region of interest (ROI) is extracted in the form of 3D bounding box. During binary classification for CAC segmentation, ROI is classified if it is CAC or not. If it is CAC classified, then in the next phase it is further classified into the specified class where
Figure 6: Pre-treatment phase - image volume is passed through preprocessing step in which Region of interest (ROI) is extracted in the form of 3D bounding box. During binary classification for CAC segmentation, ROI is classified if it is CAC or not. If it is CAC classified, then in the next phase it is further classified into the specified class where
it belongs.23
Conclusion
Cardiovascular risk assessment can be improved using CAC scoring and AI. CAC score enhances risk stratification with traditional risk factors and the CAC score on its own is effective in predicting CHD risk.24,25 Traditional risk factors tend to overestimate or underestimate the actual CHD risk, meaning that including CAC score in risk stratification has a potential to reduce over- and undertreatment. Furthermore, several methods have been developed to automate CAC scoring. These methods are shown to be accurate and significantly more time effective compared to non-AI-based methods that required a lot of human efforts; however, more studies are required for cost and benefit analyses of automating CAC. Further research is recommended in investigating the effect of CAC score in reducing over- and undertreatment. Larger datasets are required for deep-learning systems (i.e., to evaluate the methods for coronary artery segmentation and calculation of CAC). Statistical parameters such as sensitivity, specificity, precision, recall, and F1 score need to be defined and for this purpose, several studies are required. Taken together, automated CAC scoring using deep-learning system coupled with electronic medical records can help clinicians identify patients at high risk in time-efficient manner.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. World Health Organization. Cardiovascular diseases (CVDs). 2021 [cited 2022 August 30]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
- 2. Byrne P, Cullinan J, Smith A, Smith SM. Statins for the primary prevention of cardiovascular disease: an overview of systematic reviews. BMJ Open 2019 Apr;9(4):e023085.
- 3. Lee S, Rim B, Jou SS, Gil HW, Jia X, Lee A, et al. Deep-learning-based coronary artery calcium detection from CT image. Sensors (Basel) 2021 Oct;21(21):7059.
- 4. Alashi A, Lang R, Seballos R, Feinleib S, Sukol R, Cho L, et al. Reclassification of coronary heart disease risk in a primary prevention setting: traditional risk factor assessment vs. coronary artery calcium scoring. Cardiovasc Diagn Ther 2019 Jun;9(3):214-220.
- 5. Dunleavy MP, Guha A, Cardona A, Fortuna C, Daoud EG, Raman SV, et al. Prevalence of coronary artery calcification on pre-atrial fibrillation ablation CT pulmonary venograms and its impact on selection for statin therapy. J Clin Med 2020;9(6):1631.
- 6. Neves PO, Andrade J, Monção H. Coronary artery calcium score: current status. Radiol Bras 2017 May-Jun;50(3):182-189.
- 7. Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, et al; American Heart Association Committee on Cardiovascular Imaging and Intervention; American Heart Association Council on Cardiovascular Radiology and Intervention; American Heart Association Committee on Cardiac Imaging, Council on Clinical Cardiology. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American heart association committee on cardiovascular imaging and intervention, council on cardiovascular radiology and intervention, and committee on cardiac imaging, council on clinical cardiology. Circulation 2006 Oct;114(16):1761-1791.
- 8. Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008 Mar;358(13):1336-1345.
- 9. Silverman MG, Blaha MJ, Krumholz HM, Budoff MJ, Blankstein R, Sibley CT, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the multi-ethnic study of atherosclerosis. Eur Heart J 2014 Sep;35(33):2232-2241.
- 10. McClelland RL, Jorgensen NW, Budoff M, Et A, McClelland RL, Jorgensen NW, et al. Ten-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: derivation in the multi-ethnic study of atherosclerosis with validation in the Heinz Nixdorf recall S. J Am Coll Cardiol 2015;66(15):1643-1653.
- 11. Grandhi GR, Mirbolouk M, Dardari ZA, Al-Mallah MH, Rumberger JA, Shaw LJ, et al. Interplay of coronary artery calcium and risk factors for predicting CVD/CHD mortality: the CAC consortium. JACC Cardiovasc Imaging 2020 May;13(5):1175-1186.
- 12. Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis. Arch Intern Med 2004 Jun;164(12):1285-1292.
- 13. Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet 2011 Aug;378(9792):684-692.
- 14. Nasir K, Rubin J, Blaha MJ, Shaw LJ, Blankstein R, Rivera JJ, et al. Interplay of coronary artery calcification and traditional risk factors for the prediction of all-cause mortality in asymptomatic individuals. Circ Cardiovasc Imaging 2012 Jul;5(4):467-473.
- 15. Gonzalez G, Washko GR, Estepar RS. Automated agatston score computation in a large dataset of non ECG-gated chest computed tomography. Proc - Int Symp Biomed Imaging 2016;2016:53-57.
- 16. Išgum I, Prokop M, Niemeijer M, Viergever MA, van Ginneken B. Automatic coronary calcium scoring in low-dose chest computed tomography. IEEE Trans Med Imaging 2012 Dec;31(12):2322-2334.
- 17. Singh SP, Wang L, Gupta S, Goli H, Padmanabhan P, Gulyás B. 3D deep learning on medical images: a review. Sensors 2020 Sep 7;20(18):5097.
- 18. Sandstedt M, Henriksson L, Janzon M, Nyberg G, Engvall J, De Geer J, et al. Evaluation of an AI-based, automatic coronary artery calcium scoring software. Eur Radiol 2020 Mar;30(3):1671-1678.
- 19. de Vos BD, Wolterink JM, Leiner T, de Jong PA, Lessmann N, Išgum I. Direct automatic coronary calcium scoring in cardiac and chest CT. IEEE Trans Med Imaging 2019 Sep;38(9):2127-2138.
- 20. Fischer AM, Eid M, De Cecco CN, Gulsun MA, van Assen M, Nance JW, et al. Accuracy of an artificial intelligence deep learning algorithm implementing a recurrent neural network with long short-term memory for the automated detection of calcified plaques from coronary computed tomography angiography. J Thorac Imaging 2020 May;35(Suppl 1):S49-S57.
- 21. Lee JG, Kim H, Kang H, Koo HJ, Kang JW, Kim YH, et al. Fully automatic coronary calcium score software empowered by artificial intelligence technology : validation study using three CT cohorts. Korean Journal of Radiology 2021;22(11):1764-1776.
- 22. Gogin N, Viti M, Nicodème L, Ohana M, Talbot H, Gencer U, et al. Automatic coronary artery calcium scoring from unenhanced-ECG-gated CT using deep learning. Diagn Interv Imaging 2021 Nov;102(11):683-690.
- 23. Zair AM, Bouzouad Cherfa A, Cherfa Y, Belkhamsa N. Machine learning for coronary artery calcification detection and labeling using only native computer tomography. Phys Eng Sci Med 2022 Mar;45(1):49-61.
- 24. Peters SA, Bakker M, den Ruijter HM, Bots ML. Added value of CAC in risk stratification for cardiovascular events: a systematic review. Eur J Clin Invest 2012 Jan;42(1):110-116.
- 25. Nasir K, Clouse M. Role of nonenhanced multidetector CT coronary artery calcium testing in asymptomatic and symptomatic individuals. Radiology 2012 Sep;264(3):637-649.