|
A thyroid mass, most often a non toxic colloid goiter or occasionally an adenoma, is not an unusual finding below the level of the thoracic inlet.1 In 1992 Creswell and Wells estimated that these tumors comprise 5.8% of all mediastinal lesions.1 There is no standard definition for thyroid glands extending below the thoracic inlet, but such masses descend from their original cervical location for more than 2 or 3 cm below the thoracic inlet, and are not truly primary tumors of the mediastinum. They preserve the connection between the thoracic and cervical portion and receive their blood supply from the neck.2,3 In 1940, the seminal report of Wakeley and Mulvany divided intrathoracic thyroid masses into 3 types; (1)”Small substernal extension” of a mainly cervical mass, (2) “Partial” intrathoracic, in which the major portion of the mass is situated within the thorax, and (3)”Complete” in which all of the mass lies within the thoracic cavity.1 It has been found that 80% of the substernal thyroid masses are of small extension type, 15% are of the partial type and 2-4% is of the complete type. These masses extend into the visceral compartment of the mediastinum and even the anterior substernal extension remains in the same compartment, being confined anteriorly by the pre-tracheal fascia.1
An intrathoracic goiter on the right side which is anterior or anterolateral to the trachea originally enters the mediastinum via the visceral compartment, but once within the thorax, the lower aspect of the mass may pass in front of the ascending arch of the aorta into the anterior mediastinum. Substernal enlargement of a goiter can cause compression of several mediastinal structures including the trachea, esophagus and superior vena cava, and these indicates urgent resection of the mass.4,5 These tumors either partial or complete will require surgical excision, usually through the cervical incision.4-8 In this study we review our experience and surgical approach for thyroid masses extending to a variable extent into the mediastinum and compressing the trachea.
This study is a retrospective one. This is a review of medical charts and radiological images of 16 patients with substernal extension of thyroid gland that were operated upon during the period of 2006 to 2009 at King Fahad University Hospital. Twelve patients (75%) were females and only four patients (25%) were males. The mean age was 45 years.
The prominent preoperative presentations were a palpable neck mass of variable size (15=93.75%), dyspnea (14=87.5%), and dysphagia (4=25%). Thyrotoxic manifestations were only present in 2 cases (12.5%), while all the other cases (14=87.5%) were euthyroid. Routine blood investigations, thyroid function tests and thyroid antibodies were done to all patients. Chest X-ray (CXR), Computed Tomography (CT) neck and upper chest were done to all patients and showed variable degrees of tracheal compression. (Figs. 1,2)
Indirect laryngoscopy was also done as a preoperative routine to all patients. Tracheal compression was clearly diagnosed radiologically, but in 4 cases (25%), bronchoscopic evaluation of the airways was needed to exclude infiltrations and to assess the condition of the trachea. Esophagoscopy was required in only 2(12.5%) patients presented with severe dysphagia to exclude esophageal lesions. Preoperative Fine Needle Aspiration Cytology (FNAC) was done in 5(31%) patients only when we suspected malignancy, while the other 11 patients were planned for thyroidectomy without FNAC.
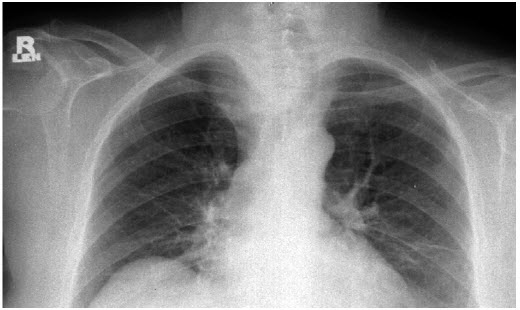
Figure 1: CXR of a partial substernal goiter compressing the trachea from the right side.

Figure 2: CT of a partial substernal goiter compressing the trachea from the left side.
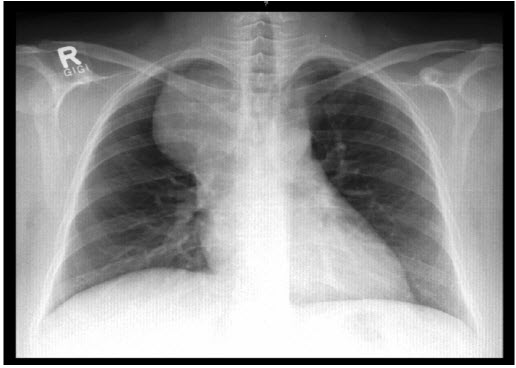
Figure 3: CXR of a right sided mediastinal mass, proved to be a substernal goiter of the complete type “Forgotten Goiter”

Figure 4: CT of a right sided mediastinal mass, proved to be a substernal goiter of the complete type “Forgotten Goiter”
Pre-operatively, 9 (56.25%) patients were diagnosed to have goiter with small substernal extension, 6 (37.5%) with the partial intrathoracic type, and 1 (6.25%) patinet was diagnosed with the complete substernal type. (Figs. 3,4)
In 12 (75%) cases cervical collar incision was adequate to remove the gland with substernal extension. An additional sternal split was required only in 3 (18.75%) cases. But one case with complete substernal type total excision was achieved only through a right posterolateral thoracotomy in the 4th intercostal space, (Fig 5). Midline sternotomy was not required in any of the patients cases.
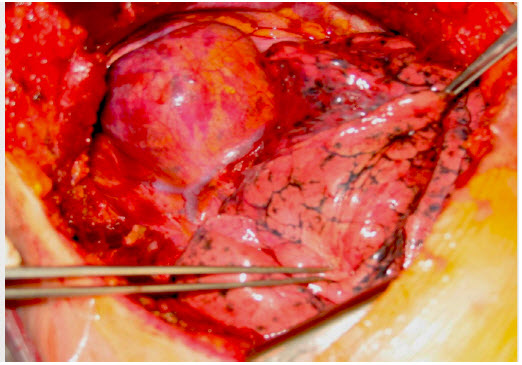
Figure 5: The complete substernal goiter covered by the mediastinal pleura as viewed though a right posterolateral thoracotomy.
All patients were extubated at the end of the procedure and transferred to the Intensive Care Unit (ICU) for overnight observation. There was neither mortality nor major morbidity among the sixteen patients except for one patient who developed transient hypoparathyroidism. The mean ICU stay was 24 hours and the mean hospital stay was 5 days (range from 5 to 11 days).
The mean follow-up period was 2 years (range from 3 months - 3 years). Pathological examination of the excised glands proved that 15 patients (93.75%) had a colloidal goiter, one case (6.25%) of autoimmune lymphocytic thyroiditis (Hashimoto’s disease) and there were no cases of malignancy. All 16 patients underwent clinical and radiological studies and remained recurrence- free for the period of follow up.
The definition of substernal goiter is not uniform and varies among authors, but it usually denotes a thyroid formation with cervical departure that goes beyond the superior thoracic inlet for at least 3 cm and preserves the connections between the thoracic and cervical portions.2 Surgery for mediastinal goiters should always be considered, even in elderly patients because of the high risk of tracheal compression and the low morbidity of the surgery.7 Although we have not seen cases of tracheomalacia, but radiological assessment of all our cases had shown a variable degree of tracheal compression and to a lesser extent esophageal compression. The majority of our cases (87.5%) presented with dyspnea. Most mediastinal goiters are benign and can be removed through a cervical approach with or without a sternal split.7,8 In our series there were no malignant cases. All the cases were of a colloidal goiter apart of one case of auto immune thyroiditis. In 75% of our cases the cervical collar incision was sufficient to perform the thyroidectomy and the partial sternal split was only required in 18.75% of the cases. Although preparation for sternotomy was stand by but it was not needed in any of our cases.
The “forgotten” goiter is an extremely rare disease; a mediastinal thyroid mass found after total thyroidectomy.1,2 We have one case of a right sided upper visceral mediastinal mass compressing the airways and presented 5 years after a previous thyroidectomy, with no data of the previous operation. This mass was completely removed through a right posterolateral thoracotomy in the 4th intercostal space. The mass was covered with mediastinal pleura and well encapsulated. The mass contained the characteristic colloid contents of the thyroid nature. We cannot consider this case as an ectopic goiter because it does not fulfill the required criteria mentioned by Shields.1
In conclusion, early surgery for all cases of substernal thyroid masses allows definitive diagnosis of the nature of the mass as well as curative. Tracheal compression will be relieved early to avoid the later development of tracheomalacia. Most of these masses are successfully removed through the cervical collar incision, with the need of partial sternal split in few cases to give better access to the mediastinum.
ACKNOWLEDGEMENTS
The authors reported no conflict of interest and funding has been received on this work.
|