A 71-year-old man presented at the emergency department (ED) and reported having acute onset central chest pain the same day while gardening. He described the pain as pressing, throbbing, and radiating posteriorly toward the nape of the neck. The pain was associated with excessive sweating including cold sweats. The patient had a history of hypertension and type 2 diabetes mellitus but denied experiencing any trauma, gastrointestinal symptoms, fever, or constitutional symptoms preceding the episode.
On presentation, the patient appeared diaphoretic and in obvious discomfort. There was no discrepancy in blood pressure between his left and right upper limbs. His heart rate was 110 beats/min with a regular rhythm, and he was afebrile. Oxygen saturation was 100% in ambient air. Systematic physical examination results were unremarkable. No murmurs were detected on the cardiovascular examination. Bedside point-of-care cardiac troponin level was grossly elevated at 1220.8 ng/L (99th percentile is 40 ng/L). The patient’s electrocardiogram (ECG) and chest radiograph were taken [Figures 1 and 2].
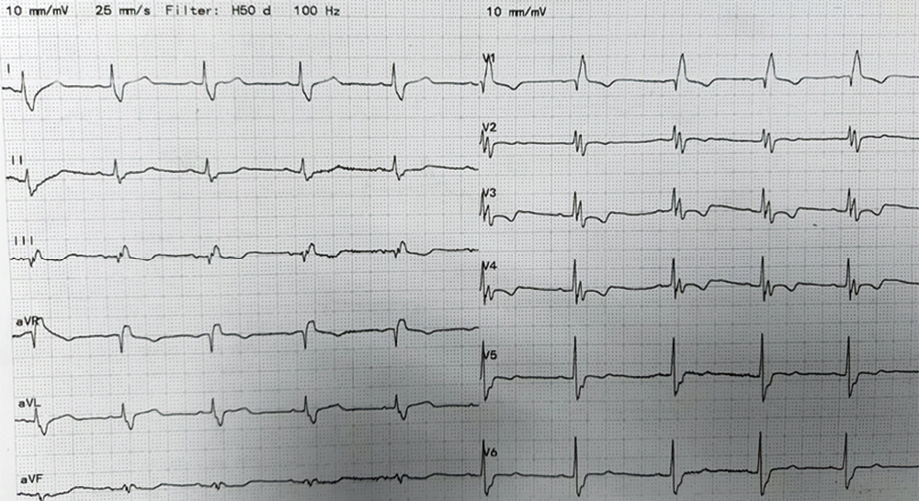 Figure 1: Electrocardiogram at presentation.
Figure 1: Electrocardiogram at presentation.
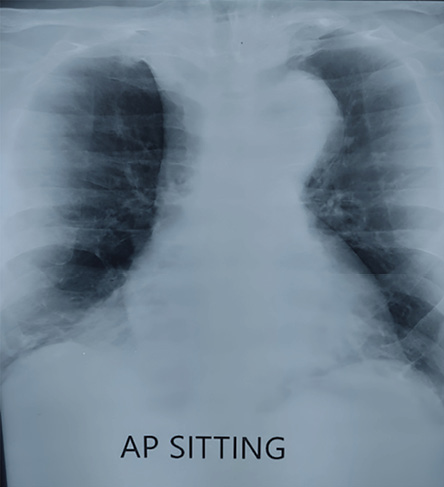 Figure 2: Chest radiograph at presentation.
Figure 2: Chest radiograph at presentation.
Question
What would be the best next step for management?
a. Administer intravenous thrombolytics for an acute ST-elevation myocardial infarction.
b. Request cardiology consultation for an angiogram.
c. Arrange a computed tomography (CT) aortogram for suspected aortic dissection.
d. Monitor serial ECGs.
Answer
c. Arrange a CT aortogram for suspected aortic dissection.
The CT aortogram of the patient revealed an impending rupture of an aortic arch aneurysm [Figure 3].
Upon closer review, the patient’s ECG revealed a right bundle branch block with appropriate discordance in leads V1–V4. There was also a subtle ST elevation in lead aVR. In addition, his chest radiograph had a widened aortic knuckle raising suspicion of an aortic arch aneurysm or dissection [Figure 4].
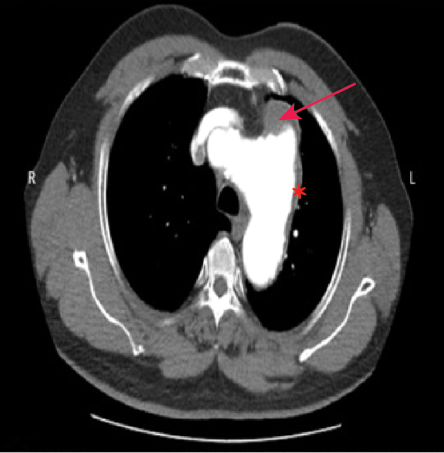 Figure 3: CT aortogram showing dilated
Figure 3: CT aortogram showing dilated
aortic arch and aortic knuckle with an irregular
wall, indicating an aortic arch aneurysm
(asterisk). Hematoma surrounds the wall of the aneurysm (arrow).
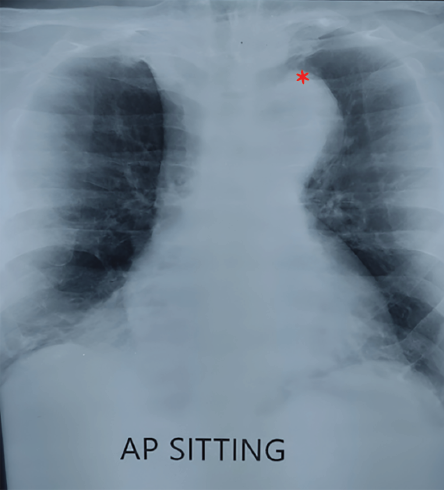 Figure 4: Dilated aortic knuckle on chest radiograph on initial presentation (asterisk).
Figure 4: Dilated aortic knuckle on chest radiograph on initial presentation (asterisk).
Unfortunately, before the CT aortogram, the patient had been given intravenous thrombolytics for a presumed ST-elevation myocardial infarction in a center without a resident cardiologist. The patient was referred to the cardiothoracic surgery team and made an uncomplicated recovery.
Discussion
A thoracic aortic aneurysm with impending rupture is one of the acute aortic syndromes (AASs). Given the non-specific symptoms and physical signs, a high clinical index of suspicion is necessary to detect the disease before irreversible lethal complications occur.1 The 2014 guidelines of the European Society of Cardiology on the diagnosis of aortic diseases are recommended for emergency physicians for assessing the pre-test probability of an AAS.2
Emergency clinicians tend to face a diagnostic dilemma when patients with suspected AASs present with ST-elevations on the ECG, however subtle. This is understandable, as acute coronary syndromes (ACSs) are far more common than AASs.3 Furthermore, much emphasis has been placed on the need for urgent and timely thrombolysis or primary percutaneous coronary intervention in patients with ST-elevations on the ECG, further skewing the decisions toward thrombolysis. However, it should be noted that acute aortic syndromes can also present with ST-elevations on the ECG. A study from Japan reported ST-elevations in 8.2% of the cases with confirmed AASs.4
In the assessment of a patient with acute chest pain, clinical history serves as the first discriminator to differentiate AAS and ACS. A patient presenting with chest pain radiating to the back and the nape of the neck should always raise suspicion of an aortic dissection. A physical examination should look for unequal blood pressure or unequal pulses in both upper limbs with bruits at the subclavian region, which helps narrow down the diagnostic conundrum. Ultimately, diagnostic imaging remains the mainstay of a reliable diagnosis.
In such a time-sensitive diagnostic conundrum, point-of-care ultrasound transthoracic echocardiography (TTE) is a useful ED tool to assess for features suggestive of AASs. It is non-invasive and time efficient as it can be operated by the bedside. Although diagnostic sensitivity of TTE is suboptimal, it is very useful in assessing potential high-risk features or complications, such as pericardial effusion, and diagnosing potential differential conditions.5 A negative TTE, however, does not exclude AAS.5
In a single scan session, the newer triple rule-out CT protocol can depict the pulmonary arteries, thoracic aorta, and coronary arteries. It utilizes a dedicated contrast media administration regimen to simultaneously reveal pulmonary embolism, aortic dissection, and ACS.6 However, triple rule-out-CT requires a dedicated CT scanner and sophisticated contrast protocols which may not be always feasible or available in most EDs. Therefore, CT imaging with its attendant delays may be less suitable where urgent management decisions have to be made, such as whether to conduct immediate thrombolysis.
Conclusion
Misdiagnosing ST-elevation in patients with AASs as a sign of myocardial infarction and starting them on thrombolytic and anti-platelet therapy can potentially lead to devastating outcomes. Therefore, it is important for ED clinicians to be aware that proximal aortic dissections can also manifest with ST-elevations on the ECG owing to dissection of the coronary vessels.
Disclosure
The authors declared no conflicts of interest. Consent for publication was given by the patient’s next of kin.
references
- 1. Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J 2018 Mar;39(9):739-749.
- 2. European Society of Cardiology. Aortic diseases guidelines. ESC clinical practice guidelines. 2014 [cited 2023 Mar 15]. Available from: https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Aortic-Diseases.
- 3. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al; Writing Group Members; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and stroke statistics-2016 update: a report from the American heart association: a report from the American heart association. Circulation 2016 Jan;133(4):e38-e360.
- 4. Hirata K, Wake M, Kyushima M, Takahashi T, Nakazato J, Mototake H, et al. Electrocardiographic changes in patients with type A acute aortic dissection. Incidence, patterns and underlying mechanisms in 159 cases. J Cardiol 2010 Sep;56(2):147-153.
- 5. Meredith EL, Masani ND. Echocardiography in the emergency assessment of acute aortic syndromes. Eur J Echocardiogr 2009 Jan;10(1):i31-i39.
- 6. Halpern EJ. Triple-rule-out CT angiography for evaluation of acute chest pain and possible acute coronary syndrome. Radiology 2009 Aug;252(2):332-345.