A three-year-old girl with a two-week history of choking and cough was admitted to Sultan Qaboos University Hospital with worsening respiratory distress. Computed tomography revealed obstructive emphysema in the right lower lobe of her lung. Diagnostic bronchoscopy (using a rigid bronchoscope of 4 mm internal diameter) identified an impacted metal pen cap wrapped in granulation tissue located at the entrance to the right secondary intermediate bronchus. The granulation tissue hindered further passage of the bronchoscope. Multiple attempts to remove the foreign body (FB) with rigid FB grasping forceps failed due to the inability to negotiate it through the granulation tissue which began to bleed due to the repeated manipulations.

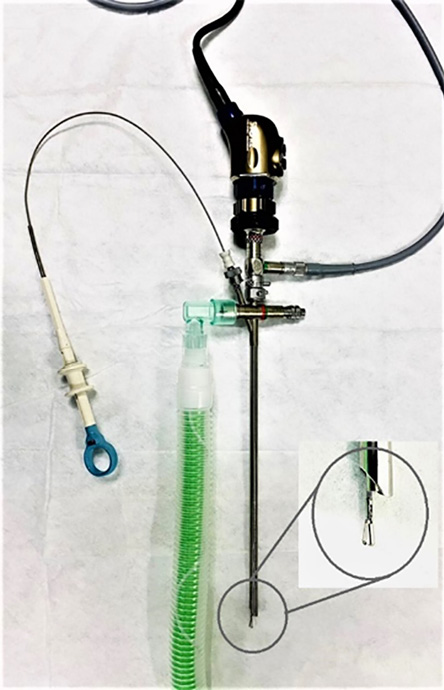 Figure 1: Rigid bronchoscope, telescope, camera, and flexible forceps assembly with the demonstration of flexible grasping forceps which runs into the rigid bronchoscope.
Figure 1: Rigid bronchoscope, telescope, camera, and flexible forceps assembly with the demonstration of flexible grasping forceps which runs into the rigid bronchoscope.

 Figure 2: The photograph demonstrates how the flexible wire forceps can grasp differently shaped objects in the bronchial airway.
Figure 2: The photograph demonstrates how the flexible wire forceps can grasp differently shaped objects in the bronchial airway.
As an alternative method, we introduced a flexible wire grasping forceps through the suction port of the rigid bronchoscope and telescope assembly [Figure 1] and positioned the scope as close to the FB as possible. The flexible wire negotiated easily through the lumen obscured by the granulation tissue and the metal pen cap was removed precisely. There was no oxygen saturation drop throughout the procedure. The postoperative period was uneventful.
It is instructive to compare our use of rigid bronchoscope with flexible wire forceps to the currently preferred method of flexible bronchoscopy to remove deeply embedded tracheobronchial FB in children. There are several reports of flexible bronchoscopy successfully removing FBs after rigid bronchoscopy failed.1–4
However, the main disadvantage of flexible bronchoscopy is the lack of simultaneous ventilation, which mandates the patient to be intubated. Another drawback is lower visibility. Our procedure avoided both these issues. The rigid bronchoscope offered simultaneous ventilation and an unobstructed view. By guiding the flexible grasping forceps through the rigid bronchoscope, it was possible to precisely grasp and remove the FB lodged in the distal bronchi without a drop in oxygen saturation during the entire procedure.5,6 Furthermore, this method avoided multiple insertions of bronchoscope, thus minimizing trauma to the delicate pediatric bronchus, especially vulnerable at secondary and tertiary bronchial levels [Figure 2].
We are sharing our experience as an alternative approach for the removal of FB in difficult-to-reach locations complicated by conditions such as granulation tissue, stenosis, etc. However, more reports of such cases are needed to standardize the technique with clearly defined indications.
Disclosure
The authors declared no conflicts of interest. Written consent was obtained from the patient.
references
1. Oliveira CF, Almeida JF, Troster EJ, Vaz FA. Complications of tracheobronchial foreign body aspiration in children: report of 5 cases and review of the literature. Rev Hosp Clin Fac Med Sao Paulo 2002 May-Jun;57(3):108-111.
2. Rodríguez H, Cuestas G, Botto H, Nieto M, Cocciaglia A, Passali D, et al. Complications in children from foreign bodies in the airway. Acta Otorrinolaringol Esp 2016 Mar-Apr;67(2):93-101.
3. Bain A, Barthos A, Hoffstein V, Batt J. Foreign-body aspiration in the adult: presentation and management. Can Respir J 2013 Nov-Dec;20(6):e98-e99.
4. Yazbeck-Karam VG, Aouad MT, Baraka AS. Laryngeal mask airway for ventilation during diagnostic and interventional fibreoptic bronchoscopy in children. Paediatr Anaesth 2003 Oct;13(8):691-694.
5. Seif MM, Huang H, Huang Z, Ning Y, Cheng Q, Jiang C, et al. Endobronchial removal of a metallic needle using a flexible diagnostic bronchoscope and biopsy forceps. A case report from Djibouti. Respir Med Case Rep 2019 Oct;28:100959.
6. Kashoob M, Al Washahi M, Tandon R. Aspiration pneumonia due to migration of fracture tracheostomy tube after 14 years of use. Oman Med J 2020 Apr;35(2):e113.