Acute pericarditis is an inflammation of the pericardium, characterized by chest pain, pericardial friction rub, and electrocardiography (ECG) changes. It is most commonly caused by viral infections. Graves’ disease is an autoimmune disorder that causes hyperactivity of the thyroid gland. There is evidence for correlation between these two entities.1–3 Possible mechanisms include autoimmune link, a direct metabolic impact from acute thyrotoxicosis, and antithyroid drugs (ATDs) induced pericarditis.
Case Report
A 28-year-old man presented to the emergency department (ED) with a four-day history of severe chest pain of a stabbing nature, localized to the left side. He also experienced palpitations, shortness of breath, and sweating. He had no previous symptoms of upper respiratory tract infection. The patient recalled a similar episode a month earlier when he was seen in a private hospital. After ECG, he was told that he had a rapid heart rate and was given some medications intravenously. The patient also revealed that during the previous three months, he had weight loss of about 12 kg, and experienced tremors, sweating, anxiety, diarrhea, and generalized weakness, which had rendered him unable to work.
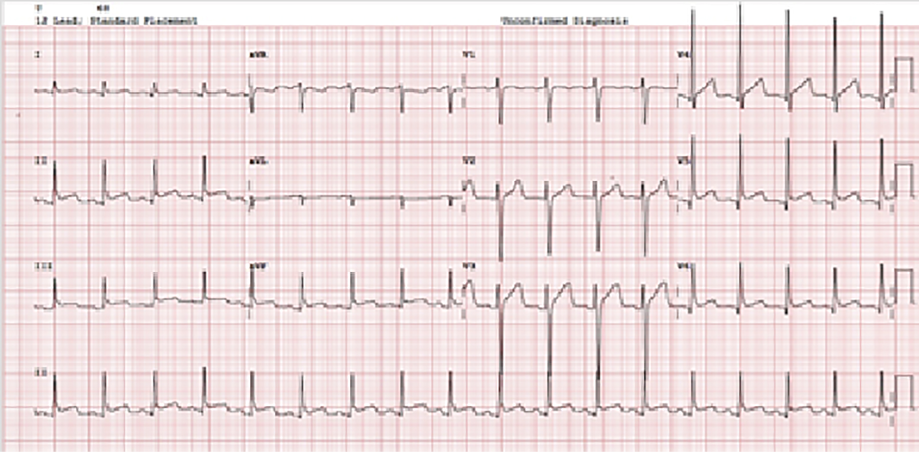
Figure 1: ECG on presentation, indicative of stage-1 acute pericarditis.
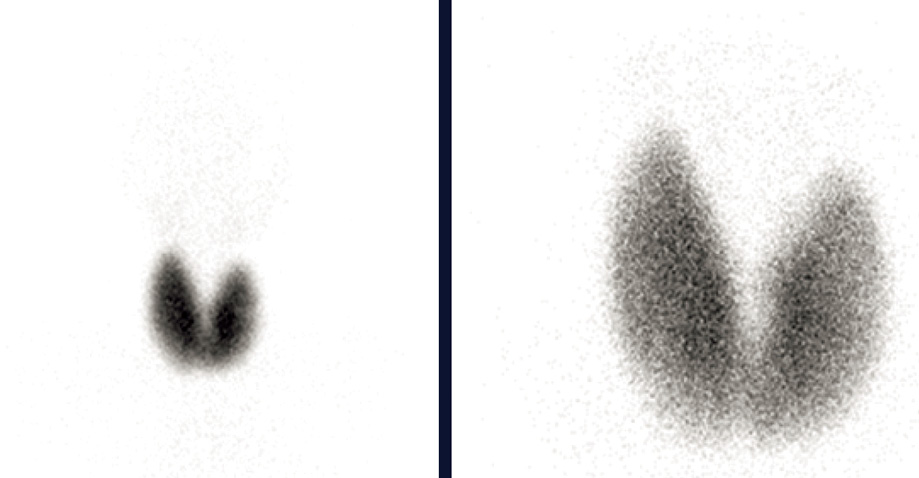
Figure 2: Tc-99m thyroid scintigraphy showing an enlarged thyroid gland with diffused increased uptake with suppression of the background, consistent with Grave’s disease
On examination in the ED, he had tachycardia (110 beats per minute) along with signs of pericardial rub with normal dual heart sounds. He was slim-built and did not have a palpable goiter. The ECG showed widespread concave ST segment elevation without reciprocal changes, a PR segment elevation in lead aVR, and PR depression in other leads. The clinical picture was highly consistent with stage-1 acute pericarditis [Figure 1].
The patient was admitted for evaluation. Laboratory investigations showed ESR 7 mm/hr and negative troponin level. Thyroid function test revealed free thyroxine (FT4) at 77.8 pmol/L (normal: 7.9–14.4) and thyroid-stimulating hormone (TSH) at 0.01 mIU/L (normal: 0.34–5.6). Echo did not find pericardial effusion, though the ejection fraction was 50%. Thyroid ultrasound showed increased vascularity with no nodules. A Tc-99 scan reported high total radiotracer uptake consistent with Graves’ disease [Figure 2]. The TSH receptor antibodies were positive.
The patient was started on propranolol (40 mg thrice a day), carbimazole (20 mg twice a day) along with a tapering dose of ibuprofen (800 mg thrice a day) and colchicine (500 mcg once a day). When seen in the clinic after a week, he showed a dramatically positive clinical response.
Discussion
Graves’ disease is an autoimmune condition characterized by high levels of FT4 and triiodothyronine, a diffuse goiter, and Graves’ opthalmopathy.4 Cardiovascular manifestations are common and include cardiac arrhythmias like atrial fibrillation, congestive cardiac failure, thyrotoxic cardiomyopathy, and pulmonary arterial hypertension.
Acute pericarditis is one of the most common pericardial syndromes seen in clinical practice. It is diagnosed based on the presence of any two of the following criteria: chest pain, pericardial friction rub, characteristic ECG changes (new widespread ST-elevation or PR depression), and pericardial effusion.5 Viral infections are the most common cause of pericarditis. Other causes include bacterial infections, tuberculosis, myocardial infarction, trauma, malignancy, and autoimmune diseases.
Several case reports have suggested an association between Graves’ disease and acute pericarditis, the earliest being in 1958.6 Some of these cases were similar to ours, where patients presented with typical clinical picture of acute pericarditis, to be found upon confirmatory testing to have thyrotoxicosis secondary to Graves’ disease.1,2,7 On the other hand, there were cases of acute pericarditis developing in patients who were already on treatment for confirmed Graves’ disease.3,8,9
Graves’ disease is associated with the presence of anti-TSH receptor antibodies and antithyroid peroxidase antibodies.8 Likewise, antinuclear antibodies have been detected in patients with idiopathic recurrent acute pericarditis.5 Autoimmune reaction is the most acceptable explanation for the association between Graves’ disease and pericarditis. Clarke et al,8 proposed that pericarditis in Graves’ disease may share the same autoimmune etiology as ophthalmomyopathy and dermopathy. An alternate explanation is direct metabolic impact from acute thyrotoxicosis leading to an alteration in pericardial fat metabolism.10 On the other hand, many case reports described pericarditis after initiation of antithyroid medication, raising the possibility of pericarditis being induced by antithyroid drugs. Indeed, there is significant evidence that propylthiouracil can cause pericarditis.9 Other antithyroid drugs such as iodine and carbimazole can also cause acute pericarditis.11
Pericardial involvement can manifest as mild pericarditis without effusion, cardiac tamponade,12 or even myopericarditis with or without hemo-dynamic instability.13
Conclusion
Despite absence of a solid evidence-based pathophysiological mechanism to explain the association between Graves’ disease and pericarditis, clinicians should be aware of this association. The management should include treatment of thyrotoxicosis and concurrent treatment of pericarditis.
Disclosure
The authors declared no conflicts of interest. Informed consent was given by the patient to publish this case report.
references
- 1. Tsai M-S, Yang C-W, Chi C-L, Hsieh C-C, Chen W-J, Huang C-H. Acute pericarditis: a rare complication of Graves’ thyrotoxicosis? Am J Emerg Med 2006 May;24(3):374-375.
- 2. Koo EH, Kim SM, Park SM, Park JW, Kim EK, Lee GY, et al. Acute recurrent pericarditis accompanied by graves’ disease. Korean Circ J 2012 Jun;42(6):419-422.
- 3. Sugar SJ. Pericarditis as a complication of thyrotoxicosis. Arch Intern Med 1981 Aug;141(9):1242.
- 4. Bartalena L. Graves’ orbitopathy: imperfect treatments for a rare disease. Eur Thyroid J 2013 Dec;2(4):259-269.
- 5. Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation 2005 Sep;112(13):2012-2016.
- 6. Treusch JV, Jaffe HL. Hyperthyroidism associated with presumptive acute pericarditis; a report of three cases. Calif Med 1958 Sep;89(3):217-221.
- 7. Gupta P, Chhabra L, Hiendlmayr B, Spodick DH. Thyrotoxic pericarditis: an underappreciated phenomenon. Int J Cardiol 2015 Nov;198:32-33.
- 8. Clarke NR, Banning AP, Gwilt DJ, Scott AR. Pericardial disease associated with Grave’s thyrotoxicosis. QJM 2002 Mar;95(3):188-189.
- 9. Colakovski H, Lorber DL. Propylthiouracil-induced perinuclear-staining antineutrophil cytoplasmic autoantibody-positive vasculitis in conjunction with pericarditis. Endocr Pract 2001 Jan-Feb;7(1):37-39.
- 10. Chhabra L, Spodick DH. A comment on thyrotoxic pericarditis. Int J Cardiol 2014 May;173(3):587.
- 11. Airel PS, Steele MB, Lin AH, Seidensticker DF, Shwayhat AF. Pericarditis, thymic hyperplasia, and Graves’ thyrotoxicosis: case report and review of the literature. Mil Med 2013 Jul;178(7):e865-e869.
- 12. Tourniaire J, Sassolas G, Touboul P, Lejeune H, Berger M. [Tamponade caused by subacute pericarditis in Basedow’s disease]. Presse Medicale Paris Fr 1983 Sep 17;12(32):1989-1990.
- 13. Kukla P, Bryniarski L, Bromblik A, Szczuka K, Kawecka-Jaszcz K. [Myopericarditis complicated with cardiogenic shock mimicking acute coronary syndrome with ST elevation in a patient with hyperthyroidism and diabetes mellitus]. Kardiol Pol 2008 Sep;66(9):982-986.