Asymptomatic bacteriuria (ASB) is the presence of at least 105 colony-forming units per milliliter (CFU/mL) of one or two uropathogens in a culture of midstream urine collected from a patient with no symptoms or signs of urinary tract infection (UTI).1 Asymptomatic bacteriuria is common in people with abnormal genitourinary tract condition, and its prevalence varies among diverse populations and depends on sex, age, medical conditions (like diabetes mellitus or spinal cord injury), and the presence of functional or structural genitourinary abnormalities.2 ASB could progress to symptomatic UTI and has potential for renal damage in certain medical conditions.2
Sickle cell disease (SCD) patients are vulnerable to UTIs, often preceded by ASB due to their impaired immunity in addition to vaso-occlusive processes, which leads to the formation of alkaline and dilute urine which encourages the growth of bacteria.2,3 This infection may advance to renal damage as a result of several physiological and anatomical abnormalities.4 Therefore, early screening of SCD patients for ASB and treatment may be necessary if ASB indeed progresses to symptomatic UTI due to its potential to cause renal damage and the adverse effect of infections in these immuno-compromised patients.
The rising incidence of antimicrobial resistance among urinary pathogens has made it difficult to select appropriate treatment regimens for infections that are caused by multidrug-resistant urinary pathogens. In the last 10 years, there have been global reports of emerging antibiotic resistance, including in Nigeria, among uropathogens due to the production of extended-spectrum beta-lactamases (ESBL), carbapenemases, and New Delhi metallo-beta-lactamases.5–11 Infections that are caused by multidrug-resistant pathogens need timely and appropriate treatment. Therefore, regular monitoring of the diversity of agents of UTI and their susceptibility profile is imperative to limit the development of chronic kidney disease or permanent kidney dysfunction in this high-risk group. This study was conducted to determine the prevalence of ASB, antimicrobial susceptibility profile of isolates, extended-spectrum β-lactamase production, and the presence of blaSHV, blaCTX-M, and blaTEM genes in ESBL producing isolates.
Methods
We conducted a cross-sectional study that involved patients with sickle cell anemia (SS) and sickle cell hemoglobin-c (SC) disease routinely attending the sickle cell clinic of the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC) and Obafemi Awolowo University (OAU) Health Centre in Nigeria. Sampling was performed over six-months (July to December 2017), and 59 single voided midstream urine samples were aseptically collected consecutively from patients in the steady-state aged 16 years and above as they presented to the clinic. A control group of 116 apparently healthy individuals with hemoglobin AA genotype were also recruited from the students and staff of OAU. Those suspected to have conditions that can predispose them to UTIs and those with symptoms of UTI and on antibiotics within the preceding 14 days of sampling were excluded from the study. The patients' sociodemographic and clinical data were obtained using a proforma. We obtained the approval of the Ethics and Research Committees of OAUTHC and OAU Health Centre to conduct the study. Written informed consent was required to participate in the study. Midstream clean voided urine samples were collected from participants in sterile universal bottles and transported on ice to the laboratory for investigations within two hours of collection.
Urine specimens were examined under the microscope and tested with Combo 10 urine dipstick (DFI Co., Ltd, India) for urinalysis. The specimens (5 mL) were centrifuged at 2500 rpm for five minutes, and urine sediments were examined for casts, crystals, red blood cells, leukocytes, and bacteria.
We used semi-quantitative analysis. Well-mixed uncentrifuged urine specimens were cultured within two hours of collection on well dried Cysteine Lactose Electrolyte Deficient Medium (CLED) (HiMedia, India) and blood agar using a standard calibrated (0.01 mL) platinum wire loop. Each culture plate was read after 18–24 hours incubation at 37 ºC under aerobic conditions.12 Samples that yielded one isolate with a colony count ≥ 105 CFU/mL, or two uropathogens with one or both colonies count ≥ 105 CFU/mL were considered to have significant bacteriuria.1 Samples with more than two organisms were considered contaminated, while counts < 105 CFU/mL was not significant. Bacterial isolates were identified based on their macro-morphology, micro-morphology, Gram’s staining reaction, and biochemical characteristics. The Gram-negative isolates were characterized with MicrobactTM GNB 24E identification kit (Oxoid Ltd, Basingstoke, United Kingdom) and identified with MicrobactTM Computer Aided Identification Package, version 2.04 (Oxoid Ltd, Basingstoke, United Kingdom).
Bacterial sensitivity to 20 antibiotics was determined using the Kirby-Bauer disc diffusion method with commercial antimicrobial discs (Oxoid, England; MAST, England; Abtek biological Ltd, England and Himedia, India) following the guidelines of Clinical and Laboratory Standard Institute.13 The antibiotics used and their disc concentrations were as follows: nitrofurantoin (300 µg), norfloxacin (10 µg), gentamicin (10 µg), amoxicillin-clavulanate (30 µg), ceftriaxone (30 µg), cefotaxime (30 µg), sulfamethoxazole-trimethoprim (25 µg), chloramphenicol (30 µg), ciprofloxacin (5 µg), meropenem (10 µg), vancomycin (30 µg), ceftazidime (30 µg), penicillin (10 U), ofloxacin (5 µg), cefepime (30 µg), ampicillin (10 µg), tetracycline (30 µg), streptomycin (10 µg), erythromycin (15 µg), and cefoxitin (30 µg). Staphylococcus aureus ATCC25923 and Escherichia coli ATCC 25922 were used as reference strains for the test.
Ceftazidime (30 μg) and cefotaxime (30 μg) with and without clavulanic acid (10 μg) were used to confirm ESBL production by the combination disc method.14 An increase in the inhibition zone diameter of ≥ 5 mm in a third-generation cephalosporin disk combined with clavulanic acid, compared to the third-generation cephalosporin alone, indicated ESBL production.
Fresh bacterial isolates were grown for 24 hours in 4 mL of peptone broth (Oxoid, England). An aliquot (1 mL) of the culture was centrifuged at 10 000 rpm for two minutes. The pellet obtained was suspended in 100 µL of sterile distilled water and boiled for 15 minutes. The DNA suspension was used for polymerase chain reaction (PCR) amplification. All Gram-negative isolates that were phenotypically positive for ESBL production were screened by multiplex-PCR using primers specific for the detection of blaSHV, blaCTX-M, and blaTEM genes [Table 1].15 The conditions used for amplification reactions were: initial denaturation at 94 °C for three minutes followed by denaturation at 94 °C for 45 seconds, annealing at 60 °C for TEM, SHV and CTX-M and extension at 72 °C for one minute 35 times, and a terminal extension at 2 °C for three minutes. Each amplicon (10 μL) was electrophoresed on a 1.5% agarose gel in 1X Tris-Borate-EDTA (TBE) buffer. Ethidium bromide (0.5 μg/mL) was used to stain the gels for 10 minutes, and then destained in distilled water for 20 minutes, and viewed under ultraviolet light using a UVitec transilluminator (Avebury, Cambridge UK). The position of amplified products was estimated by the position of the 100bp molecular weight marker (Biolab, England). The ESBL genes were sequenced using a forward (M13F43) and reverse (M13R49) primer.
Statistical analysis was done using SPSS Statistics (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Proportions were compared using Mann-Whitney’s U and Fisher’s exact probability test. Inferences were made based on the computed prevalence ratios, their 95% confidence intervals, and p-values. Alpha level was set at p < 0.050.
Table 1: Primers used for sequencing of ESBL genes by PCR.
|
SHV |
SHV-F |
CGCCTGTGTATTATCTCCCT |
293 |
| |
SHV-R |
CGAGTAGTCCACCAGATCCT |
|
|
TEM |
TEM-F |
TTTCGTGTCGCCCTTATTCC |
403 |
| |
TEM-R |
ATCGTTGTCAGAAGTAAGTTGG |
|
|
CTX-M |
CTX-M-F |
CGCTGTTGTTAGGAAGTGTG |
874 |
ESBL: extended spectrum beta-lactamase PCR: polymerase chain reaction.
Results
We recruited 175 participants in the study, of which 59 were patients with SCD, while 116 were healthy controls with hemoglobin AA genotype. One of the case specimens was excluded due to contamination. Both groups were similar in sex distribution, mean age, and marital status but differed significantly in education level [Table 2].
Table 2: Demographic characteristics of the study participants.
|
Gender |
|
|
0.628* |
|
Male |
23 (39.7) |
51 (44.0) |
|
|
Female |
35 (60.3) |
65 (56.0) |
|
|
Mean age, mean ± SD, years |
25.0 ± 8.1 |
24.0 ± 4.0 |
0.195§ |
|
Age group, years |
|
|
0.005* |
|
≥ 30 |
15 (25.9) |
10 (9) |
|
|
< 30 |
43 (74.1) |
106 (91) |
|
|
Education level |
|
|
< 0.010* |
|
Secondary |
14 (24.1) |
0 (0.0) |
|
|
Tertiary |
44 (75.9) |
116 (100) |
|
|
Marital status |
|
|
0.183* |
|
Single |
52 (98.7) |
111 (95.7) |
|
*Fisher’s exact probability test
§Mann-Whitney U test
Mann-Whitney U (Z) = 2959.000
SCD: sickle cell disease; SD: standard deviation; HbAA: hemoglobin AA.
Five (8.6%) of the 58 patients with SCD and one (0.9%) of 116 controls had significant bacteriuria. All positive cases occurred in females in both groups [Table 3]. Primary outcome results indicate a significant difference in proportion of patients with ASB (n = 5/58; 8.6%) compared to 0.9% (n = 1/116) in the control group (p = 0.016). ASB was 10-times more prevalent among patients with SCD compared with individuals with normal hemoglobin (prevalence rate (PR) = 10.000, 95% confidence interval (CI): 1.196 – 83.626).
Two (13.3%) of 15 patients aged 30 years and above had ASB compared to 7.0% (3/43) of those below 30 years (PR = 1.911, 95% CI: 0.353–10.356, p = 0.596). Two (33.3%) of six married patients had ASB compared to 5.8% (3/52) of single patients (PR = 5.778, 95% CI: 1.194–27.968, p = 0.023). Two (4.5%) of 44 patients with a tertiary level of education had ASB compared to 21.4% of those (3/14) without tertiary education (PR = 4.714, 95% CI: 0.874–25.424, p = 0.085) [Table 4].
Both Gram-negative and Gram-positive organisms were isolated in equal proportion in the patients, with coagulase-negative staphylococci being predominant (n = 2, 33.3%). Staphylococcus saprophyticus (n = 1; 16.7%), Acinetobacter baumannii (n = 1, 16.7%) (both were isolated from a single specimen), Staphylococcus epidermidis (n = 1, 16.7%), Enterobacter cloacae (n = 1, 16.7%), Stenotrophomonas maltophilia (n = 1, 16.7%), and Corynebacterium sp. (n = 1; 16.7%) were isolated from SCD patients. While Acinetobacter baumannii was the only isolate from controls [Table 5].
All isolates were multidrug-resistant, with Enterobacter cloacae having the highest percentage resistance (n = 10/11; 90.9%). All isolates were susceptible to meropenem, and all were resistant to penicillin, ampicillin, ceftazidime, and tetracycline. More than 50.0% exhibited resistance to cefotaxime (85.7%), ceftriaxone (85.7%), streptomycin (71.4%), chloramphenicol (71.4%), erythromycin (57.1%), nitrofurantoin (57.1%), and trimethoprim-sulfamethoxazole (57.1%). In addition, all isolates exhibited the least resistance to ciprofloxacin (28.6%), norfloxacin (28.6%), ofloxacin (20.0%), and gentamicin (14.3%). Staphylococcus epidermidis was resistant to cefoxitin and both staphylococci isolates were resistant to cefepime but sensitive to vancomycin. The Gram-positive isolates were also susceptible to nitrofurantoin and erythromycin, while the Gram-negative isolates were resistant to both. Similarly, all Gram-positive isolates were resistant to trimethoprim-sulfamethoxazole, while the Gram-negative isolates (except Enterobacter cloacae) were susceptible to the antibiotic [Table 5].
Table 3: Prevalence of asymptomatic bacteriuria (ASB) in the study population.
|
Overall ASB prevalence |
5 (58) |
8.6 |
1 (116) |
0.9 |
|
ASB prevalence in males |
0 (23) |
0.0 |
0 (51) |
0.0 |
SCD: sickle cell disease; HbAA: hemoglobin AA.
Table 4: Prevalence of asymptomatic bacteriuria (ASB) in relation to gender, age, marital status, and educational level.
|
Gender |
|
|
|
- |
- |
0.146 |
|
Female |
5 (14.3) |
30 (85.7) |
35 (100) |
|
|
|
|
Male |
0 (0.0) |
23 (100) |
23 (100) |
|
|
|
|
Total |
5 (8.6) |
53 (91.4) |
58 (100) |
|
|
|
|
Age, years |
|
|
|
1.911 |
0.353–10.356 |
0.596 |
|
≥ 30 |
2 (13.3) |
13 (86.7) |
15 (100) |
|
|
|
|
< 30 |
3 (7.0) |
40 (93.0) |
43 (100) |
|
|
|
|
Total |
5 (8.6) |
53 (91.4) |
58 (100) |
|
|
|
|
Marital status |
|
|
|
5.778 |
1.194–27.968 |
0.023* |
|
Married |
2 (33.3) |
4 (66.7) |
6 (100) |
|
|
|
|
Single |
3 (5.8) |
49 (94.2) |
52 (100) |
|
|
|
|
Total |
5 (8.6) |
53 (91.4) |
58 (100) |
|
|
|
|
Education level |
|
|
|
4.714 |
0.874–25.424 |
0.085 |
|
Secondary |
3 (21.4) |
11 (78.6) |
14 (100) |
|
|
|
|
Tertiary |
2 (4.5) |
42 (95.5) |
44 (100) |
|
|
|
*Significance at p < 0.05.
PR: prevalence; CI: confidence interval.
Table 5: Resistance index, resistance pattern of MDR uropathogens, and ESBL genes present in the ESBL producing isolate.
|
Gram-positive isolates |
|
|
|
|
|
|
|
|
Staphylococcus saprophyticus |
19 |
0.47 |
12 |
5 |
None |
NA |
CTX, CAZ, CRO, FEP, PEN, AMP, STR, TET, STX. |
|
Staphylococcus epidermidis |
19 |
0.68 |
12 |
7 |
None |
NA |
CTX, CAZ, CRO, FEP, CEF, PEN, AMP, CIP, STR, TET, CHL, STX, NOR |
|
Corynebacterium sp. |
19 |
0.42 |
12 |
5 |
None |
NA |
CAZ, FEP, PEN, AMP, STR, TET, CHL, STX |
|
Gram-negative isolates |
|
|
|
|
|
|
|
|
Acinetobacter baumannii |
17 |
0.47 |
11 |
5 |
None |
NA |
CTX, CAZ, CRO, PEN, AMP, TET, F, ERY |
|
Stenotrophomonas maltophilia |
17 |
0.53 |
11 |
6 |
None |
NA |
CTX, CAZ, CRO, PEN, AMP, TET, F, CHL, ERY |
|
Enterobacter cloacae |
18 |
0.95 |
11 |
10 |
CTX-M, TEM, SHV |
CTX-M-15 |
CTX, CAZ, CRO, FEP, AMC, PEN, AMP, CIP, STR, TET, F, CHL, C, STX, ERY, OFL, NOR |
*from control.
MDR: multi-drug resistance; ESBL: extended-spectrum β-lactamase; NA: not applicable; MAR: multiple antibiotic-resistant; CTX: cefotaxime; CAZ: ceftazidime; CRO: ceftriaxone; FEP: cefepime; AMC: amoxicillin-clavulanic acid; PEN: penicillin; AMP: ampicillin; CIP: ciprofloxacin; STR: streptomycin; TET: tetracycline; F: nitrofurantoin; CHL: chloramphenicol; C: gentamicin; STX: trimethoprim-sulfamethoxazole; ERY: erythromycin; OFL: ofloxacin; NOR: norfloxacin.*Significance at p < 0.050.
ESBL genes (blaCTX-M, blaSHV, and blaTEM) were detected only in Enterobacter cloacae [Figure 1]. BLAST results for the forward and reverse sequences of the CTX-M gene showed significant alignment with Escherichia coli strain EP225c blaCTX-M-15 gene (97% alignment) and Escherichia coli strain U4755 blaCTX-M-15 gene (95% alignment), respectively. The CTX-M allele carried by the positive isolate is CTX-M-15. The nucleotide sequence of CTX-M15 from Enterobacter cloacae was deposited in GenBank under accession number MN988686.1.
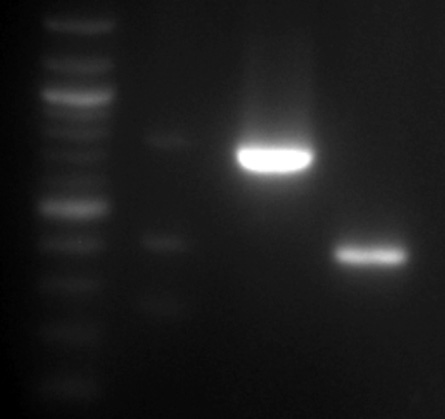
Figure 1: Polymerase chain reaction amplification of SHV (293bp), TEM (403bp), and CTX-M (874bp). Lane L: 100bp DNA-ladder, lane 1: Enterobacter cloacae (SHV, TEM and CTX-M), lane 2: Enterobacter cloacae (CTX-M), and Lane 3: Enterobacter cloacae (TEM).
Discussion
We observed a 10-fold increase in the prevalence of ASB among patients with SCD (8.6%) compared with healthy individuals with hemoglobin AA genotype (0.9%). The prevalence of 8.6% of ASB in SCD as observed in this study is similar to the prevalence of 4.0–17.2% reported in other studies on ASB in patients with SCD.2,3,16,17
ASB tends to be more prevalent among older female patients without tertiary education and is significantly higher among married individuals, most likely due to sexual activity. Gender and age have been reported as possible factors for ASB among children with SCD.16 The higher prevalence of bacteriuria in females are attributed to anatomical and physiological factors.2 Sexual intercourse and spermicide use, especially in conjunction with diaphragm use predispose young, healthy women to UTIs. ASB in pregnant women can lead to obstetric and neonatal complications and has high sensitivity and specificity to predict a future symptomatic UTI in non-pregnant females.18–20
Several reports have shown that Escherichia coli causes most ASB, but none were isolated in this study.21,22 There have been reports of the preponderance of coagulase-negative Staphylococci (CoNs) in bacteriuria, as observed in this study.23,24 A similar study from Ghana also reported a predominance of CoNs.3 The observation of polymicrobial bacteriuria (Staphylococcus saprophyticus and Acinetobacter baumannii) in our study could pose a serious therapeutic challenge, both isolates being multidrug-resistant and with varied susceptibility to trimethoprim-sulfamethoxazole and nitrofurantoin. The diversity of etiological agents isolated from the patients could be attributed to their impaired immunity. The isolation of opportunistic pathogens such as Acinetobacter baumannii, Stenotrophomonas maltophilia, and Enterobacter cloacae corroborates the impaired immune status of these patients as these organisms are implicated in infections in immunocompromised individuals.25,26 Acinetobacter baumannii, Stenotrophomonas maltophilia, and Corynebacterium sp. are rare causes of bacteriuria and have not been reported in ASB/UTI in patients with SCD in Nigeria. Few studies have shown the clinical significance of these organisms in UTI.27–29 Inferentially, these rare causative agents of ASB/UTI are present in this environment. Authors of a study from Nigeria similarly isolated Enterobacter agglomerans and Acinetobacter baumannii from urine samples from out-patient clinics and in-patient general wards of some tertiary care hospitals.30
The multiple antibiotic-resistant (MAR) index ranges of 0.42–0.95 observed in this study denote resistance to many antibiotics and suggests high-risk source where antibiotics are frequently and improperly used, leading to high selective pressure. The uropathogens showed 100% susceptibility to meropenem alone. However, gentamicin, augmentin, and quinolones were effective against most of the Gram-positive and Gram-negative isolates. Vancomycin, nitrofurantoin, and erythromycin were effective against the Gram-positive isolates, while trimethoprim-sulfamethoxazole was effective against most of the Gram-negative isolates. The cephalosporins, ampicillin, penicillin, streptomycin, and tetracycline would not be a therapeutic choice as the isolates were commonly resistant to these agents. While this observation is at variance with Olaitan31 who observed cotrimoxazole as the most effective antibiotic, it is in line with reports from within and outside Nigeria on the high resistance of urine isolates to older antibiotics.32–34 In a similar study, there was a reduction in the sensitivity of urine isolates to cephalosporins which the authors adduced to abuse or misuse of these antibiotics.33 Finding of the high sensitivity of quinolones (ciprofloxacin, ofloxacin, and norfloxacin) in our study agrees with previous findings.35–37 However, these antibiotics were not effective against Enterobacter cloacae. These antibiotics, alongside gentamicin and meropenem, offer good therapeutic options for the treatment of bacteriuria in this environment.
The resistance of Enterobacter cloacae to penicillins, penicillin-inhibitor, and cephalosporins could be attributed to the expression of blaSHV, blaTEM, and blaCTX-M genes, as indicated in this study. Five (83.3%) of the six isolates that were resistant to cephalosporins did not produce ESBL. Invariably, other mechanisms of resistance, which could include reduced expression or alteration of PBPs, permeability alterations and extrusion by efflux pumps were used by these isolates.37
There have been earlier reports of the three common ESBL types in E. cloacae in Nigeria.38,39 Enterobacter cloacae, that is associated with the production of CTX-M-15, has been isolated from the urine of a female patient diagnosed with UTI attending the clinic of a tertiary care hospital in Nigeria.39 At present, CTX-M is the most frequently detected type of ESBL globally with the blaCTX-M-15 allele considered to be predominant in many countries.40 A gene that encodes CTX-M has been found on different plasmids ranging from 7 to 430 KB in size, as well as on large conjugative plasmids, which carry resistant genes to antimicrobials like aminoglycosides, tetracycline, trimethoprim, and sulphonamide.41 It is therefore not surprising that the isolate was resistant to 11 out of the 12 tested classes of antibiotics.
Conclusion
The prevalence of ASB in SCD in this study was 8.6%. Rare agents of ASB besides those commonly reported were isolated. Multidrug-resistant uropathogens implicated in ASB in this cohort requires guided prescriptions of antibiotics. We posit a strong need to educate females in our cohort to reduce the magnitude of ASB. Antibiotic-resistant surveillance programs should be intensified to know current etiologies of UTI and their resistant patterns to routinely prescribed antibiotics for the treatment of infection caused by these pathogens. This will help to guide empiric prescriptions to prevent treatment failure and reduce drug resistance.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
We would like to thank Dr. O.A Owojuyigbe and Dr. D. Essien of the Department of Haematology and Blood Transfusion, OAUTHC, Ile-Ife, and Mr. Olarinde Olaniran of the Department of Medical Microbiology and Parasitology, OAU, Ile-Ife for their support.
references
- 1. Kass EH. Asymptomatic infections of the urinary tract. Trans assoc am physicians 1956;69:56-64.
- 2. Cumming V, Ali S, Forrester T, Roye-Green K, Reid M. Asymptomatic bacteriuria in sickle cell disease: a cross-sectional study. BMC Infect Dis 2006 Mar;6(1):46.
- 3. Donkor ES, Osei JA, Anim-Baidoo I, Darkwah S. Risk of asymptomatic bacteriuria among people with sickle cell disease in Accra, Ghana. Diseases 2017 Feb;5(1):4.
- 4. Gebreselassie S, Simmons MN, Montague DK. Genitourinary manifestations of sickle cell disease. Cleve Clin J Med 2015 Oct;82(10):679-683.
- 5. Shill MC, Huda NH, Moain FB, Karmakar UK. Prevalence of uropathogens in diabetic patients and their corresponding resistance pattern: results of a survey conducted at diagnostic centers in Dhaka, Bangladesh. Oman Med J 2010 Oct;25(4):282-285.
- 6. Khawcharoenporn T, Vasoo S, Singh K. Urinary tract infections due to multidrug-resistant enterobacteriaceae: prevalence and risk factors in a Chicago emergency department. Emerg Med Int 2013;2013:258517.
- 7. Giwa FJ, Ige O, Haruna D, Yaqub Y, Lamido T, Usman S. Extended - spectrum beta - lactamase production and antimicrobial susceptibility pattern of uropathogens in a tertiary hospital in northwestern Nigeria. Ann Trop Pathol. 2018;9:11-16.
- 8. Ajayi AB, Nwabuisi C, Aboyeji AP, Ajayi NS, Fowotade A, Fakeye OO. Asymptomatic bacteriuria in antenatal patients in Ilorin, Nigeria. Oman Med J 2012 Jan;27(1):31-35.
- 9. Ebrahim-Saraie HS, Nezhad NZ, Heidari H, Motamedifar A, Motamedifar M. Detection of antimicrobial susceptibility and integrons among extended-spectrum β-lactamase producing Uropathogenic Escherichia coli isolates in southwestern Iran. Oman Med J 2018 May;33(3):218-223.
- 10. Zorgani A, Almagatef A, Sufya N, Bashein A, Tubbal A. Detection of CTX-M-15 among Uropathogenic Escherichia coli isolated from five major hospitals in Tripoli, Libya. Oman Med J 2017 Jul;32(4):322-327.
- 11. Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis 2010 Sep;10(9):597-602.
- 12. Cheesbrough M. District Laboratory Practice in Tropical Countries Part II. 2nd ed. Cambridge University Press; 2006. p. 113, 319-329.
- 13. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing. 2017; In CLSI supplement M100: 27th ed. [cited 2018 December]. Available from: http://file.qums.ac.ir/repository/mmrc/clsi%202017.pdf.
- 14. Carter MW, Oakton KJ, Warner M, Livermore DM. Detection of extended-spectrum beta-lactamases in klebsiellae with the Oxoid combination disk method. J Clin Microbiol 2000 Nov;38(11):4228-4232.
- 15. Monstein HJ, Ostholm-Balkhed A, Nilsson MV, Nilsson M, Dornbusch K, Nilsson LE. Multiplex PCR amplification assay for the detection of blaSHV, blaTEM and blaCTX-M genes in Enterobacteriaceae. APMIS 2007 Dec;115(12):1400-1408.
- 16. Adegoke SA, Adegun PT. Asymptomatic bacteriuria in Nigerian children with sickle cell anemia. Indian J Nephrol 2013 Mar;23(2):103-107.
- 17. Akinbami A, Ajibola S, Bode-Shojobi I, Oshinaike O, Adediran A, Ojelabi O, et al. Prevalence of Asymptomatic Bacteriuria in HIV Infected Patients in a Tertiary Hospital in Lagos, Nigeria. World J AIDS 2013;3(2):105-110.
- 18. Farkash E, Weintraub AY, Sergienko R, Wiznitzer A, Zlotnik A, Sheiner E. Acute antepartum pyelonephritis in pregnancy: a critical analysis of risk factors and outcomes. Eur J Obstet Gynecol Reprod Biol 2012 May;162(1):24-27.
- 19. Gravett CA, Gravett MG, Martin ET, Bernson JD, Khan S, Boyle DS, et al. Serious and life-threatening pregnancy-related infections: opportunities to reduce the global burden. PLoS Med 2012;9(10):e1001324.
- 20. Mazor-Dray E, Levy A, Schlaeffer F, Sheiner E. Maternal urinary tract infection: is it independently associated with adverse pregnancy outcome? J Matern Fetal Neonatal Med 2009 Feb;22(2):124-128.
- 21. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol 2015 May;13(5):269-284.
- 22. Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am 2014 Mar;28(1):1-13.
- 23. Ako-Nai AK, Kassim OO, Adeniran MO, Taiwo O. A study of urinary tract infections at Ile-Ife, Nigeria. East Afr Med J 1993 Jan;70(1):10-14.
- 24. Aboderin AO, Ako-Nai AK, Zailani SB, Ajayi A, Adedosu AN. A study of asymptomatic bacteriuria in pregnancy in Ile-Ife. Southwestern Nigeria. Afr J Clin Exp Microbiol 2004;5(3):252-259.
- 25. Bissong ME, Fon PN, Tabe-Besong FO, Akenji TN. Asymptomatic bacteriuria in diabetes mellitus patients in Southwest Cameroon. Afr Health Sci 2013 Sep;13(3):661-666.
- 26. Obeng-Nkrumah N, Labi AK, Acquah ME, Donkor ES. Bloodstream infections in patients with malignancies: implications for antibiotic treatment in a Ghanaian tertiary setting. BMC Res Notes 2015 Dec;8(1):742.
- 27. Falagas ME, Kastoris AC, Vouloumanou EK, Dimopoulos G. Community-acquired Stenotrophomonas maltophilia infections: a systematic review. Eur J Clin Microbiol Infect Dis 2009 Jul;28(7):719-730.
- 28. Sobel JD, Kaye D. Urinary tract infections. In: Mandell GL, Bennett JE, eds. Principles and practice of infectious diseases, 8th ed. Philadelphia: Elsevier Saunders; 2014. p. 886-913.
- 29. Vartivarian SE, Papadakis KA, Anaissie EJ. Stenotrophomonas (Xanthomonas) maltophilia urinary tract infection. A disease that is usually severe and complicated. Arch Intern Med 1996 Feb;156(4):433-435.
- 30. Ochada N, Nasiru I, Thairu Y, Okanlowan M, Abdulakeem Y. Antimicrobial susceptibility pattern of urinary pathogens isolated from two tertiary hospitals in southwestern Nigeria. Afr J Clin Exp Microbiol 2015;16(1):12-22.
- 31. Olaitan J. Asymptomatic bacteriuria in female students population of a Nigerian university. Internet J Microbiol 2005;2(2):1-5.
- 32. Farrell DJ, Morrissey I, De Rubeis D, Robbins M, Felmingham D. A UK multicentre study of the antimicrobial susceptibility of bacterial pathogens causing urinary tract infection. J Infect 2003 Feb;46(2):94-100.
- 33. Mava Y, Bello M, Ambe JP, Zailani SB. Antimicrobial sensitivity pattern of organisms causing urinary tract infection in children with sickle cell anemia in Maiduguri, Nigeria. Niger J Clin Pract 2012 Oct-Dec;15(4):420-423.
- 34. Okafor HU, Ibe BC, Njoku–Obi AN, Okoro BA. Bacteriology of asymptomatic bacteriuria in pre-school children in Enugu. Orient J. Med. 2005;17(3):37-42.
- 35. Adeyemo AA, Gbadegesin RA, Onyemenem TN, Ekweozor CC. Urinary tract pathogens and antimicrobial sensitivity patterns in children in Ibadan, Nigeria. Ann Trop Paediatr 1994;14(4):271-274.
- 36. Ko KS, Lee MY, Song JH, Lee H, Jung DS, Jung SI, et al. Prevalence and characterization of extended-spectrum beta-lactamase-producing Enterobacteriaceae isolated in Korean hospitals. Diagn Microbiol Infect Dis 2008 Aug;61(4):453-459.
- 37. Beceiro A, Tomás M, Bou G. Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world? Clin Microbiol Rev 2013 Apr;26(2):185-230.
- 38. Aibinu IE, Ohaegbulam VC, Adenipekun EA, Ogunsola FT, Odugbemi TO, Mee BJ. Extended-spectrum beta-lactamase enzymes in clinical isolates of Enterobacter species from Lagos, Nigeria. J Clin Microbiol 2003 May;41(5):2197-2200.
- 39. Kasap M, Fashae K, Torol S, Kolayli, F, Budak F, Vahaboglu H. Characterization of ESBL (SHV-12) producing clinical isolate of Enterobacter aerogenes from a tertiary care hospital in Nigeria. Ann Clin Microbiol Antimicrob 2010; 9(1):1.
- 40. Bevan ER, Jones AM, Hawkey PM. Global epidemiology of CTX-M β-lactamases: temporal and geographical shifts in genotype. J Antimicrob Chemother 2017 Aug;72(8):2145-2155.
- 41. Naseer U, Sundsfjord A. The CTX-M conundrum: dissemination of plasmids and Escherichia coli clones. Microb Drug Resist 2011 Mar;17(1):83-97.