|
Introduction
From the clinical point of view left ventricular remodeling is a dynamic process, starting in the acute phase of myocardial infarction (MI) with infarct expansion-that is, rearrangement of wall structure leading to myocardial thinning and lengthening, and progressing to left ventricular dilation and hypertrophy, the development of infarct expansion commonly precedes myocardial rupture and denotes a worsened prognosis.1
Left ventricular infarct expansion in the early phase of acute myocardial infarction is produced by myocardial structural changes such as myocyte necrosis, slippage, or rupture, and reduction in the intercellular space,2 which result in infarct segment lengthening and wall thining.3
A follow-up echocardiogram is excellent for identifying infarct expansion in patients with a large myocardial infarction as well as subsequent left ventricular remodeling characterized by progressive chamber dilation and further deterioration in global function.4 Contrast-enhanced magnetic resonance imaging (Ce-MRI) is an accepted gold standard for noninvasive accurate and reproducible assessment of left ventricular (LV) mass and function. Ce-MRI with gadolinium-based contrast injection offers high spatial resolution and can reliably identify the site and the extent of the infarction.5,6 Infarct expansion has drastic effects not only on the infarct zone, but also on the remote, viable contractile muscles.7
The aim of this study was to determine the incidence of early left ventricular infarct expansion within five days after first anterior ST-segment elevation myocardial infarction (STEMI) and the effect of early thrombolytic therapy on the incidence of early infarct expansion compared with late thrombolytic therapy.
Methods
A prospective review of myocardial infarction series of cases was carried out during the period from July 2007 through to September 2009. The study included 101 patients, 75 males (74.3%) and 26 females (25.74%), with first attack of anterior STEMI, who had been admitted to the Coronary Care Unit (CCU) of Hawler Teaching Hospital (Erbil-Iraq) within the first 12 hours of pain onset of acute MI who were included in the study. The mean age (±SD) was 61.07±10.78 years, ranging from 40-80 years. The patients had been referred from Emergency Department and from the Private Clinics to the CCU, from inside Erbil and from the surrounding villages and towns.
Diagnosis of acute, evoloving, or recent STEMI was based on
the following criteria:8 Typical rise and /or fall of troponin with at least one of the following: a) Ischemic symptoms and, and b)ECG
changes reading.
Transthoracic two-dimensional and Color Doppler Echocardiography had been performed (after administration of thrombolytic therapy) for all those patients within 5 days of admission to the CCU using Philips EnVisor (version 1-A, 2003).
The echocardiographic diagnosis of early left ventricular infarct expansion was made when a regional area of akinesia or dyskinesia was diagnosed or noticed that had abnormal geometry in both diastole and systole.9 During recording, particular care was taken to obtain all possible views and to optimize depth and gain settings in order to minimize the possibility of false positive or false negative readings. Ejection fraction was determined from apical and four-chamber views using the Simpson’s biplane formula.10
The patients who presented with the following were excluded from the study: a) Left sbundle branch block, b) patients with poor echocardiographic windows, c) patients with previous history of heart failure, d) previous history of the following conditions: ischemic heart disease, valvular heart disease, e) patients who died in the early phase of acute anterior myocardial infarction before echocardiographic examination, and f) patients with relative or absolute contraindication to thrombolytic therapy.11 History of diabetes mellitus, hypertension, smoking, alcohol consumption and in-hospital mortality were also recorded. Body mass index (BMI) was taken for all patients which is equal to weight of the patient/ height(m)2 of the patient. Obesity was defined as BMI ≥30.12
All patients received alteplase (tissue Plasminogen Activator) dose given over 90 minutes (bolus dose 15 mg, followed by 0.7 mg/kg body weight, but not exceeding 50 mg over 30 minutes and then 0.5 mg /kg body weight not exceeding 35 mg over 60 minutes).13 As thrombolytic therapy is most effective when given within the first 3 hours of onset of pain of acute myocardial infarction,14 we have classified our patients with acute anterior STEMI into 2 groups: those who received thrombolytic therapy (alteplase) ≤3 hours from the onset of pain of acute anterior STEMI as group I, and those patients who received thrombolytic therapy (alteplase) >3-12 hours from the onset of pain of AMI as group II.
Drug treatment at hospital was documented as anticoagulant, glyceryltrinitrate, beta blocker, angiotensin converting enzyme inhibiter, aspirin and clopidogrel.
Data were analyzed using the Statistical Package for Social Sciences (SPSS, version 15). Chi square test was used to test the association between different variables. Logistic regression analysis was carried out in order to adjust for the effect of confounders, and to estimate the odds ratio. A “p” value of ≤0.05 was considered as statistically significant.15
Results
The total study group consisted of 101 patients with first acute anterior STEMI. Seventy-five males (74.3%) and 26 females (25.74%) who had been admitted to the CCU in Erbil Teaching Hospital were enrolled in the study. The mean age (±SD) was 61±10.78 years ranging from 40-80 years. Left ventricular infarct expansion (Figs. 1 & 2) was detected within 5 days of admission to the CCU in 18 patients (17.8%).
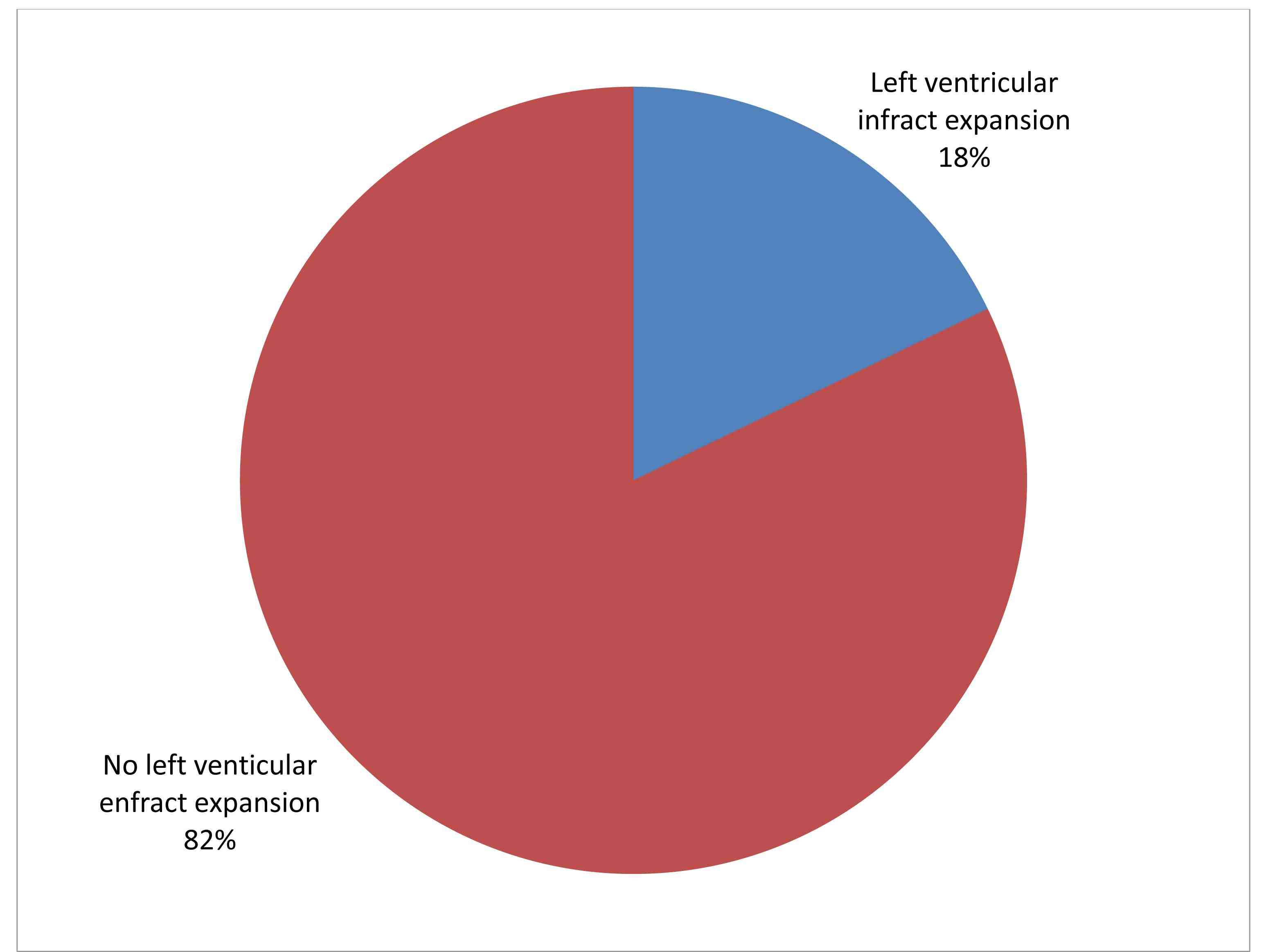
Figure 1: Incidence of early left ventricular infarct expansion in patients with acute anterior STEMI.

Figure 2: Apical four-chamber view recorded 36 hours after anterior-ST-segment elevation myocardial infarction. Note early left ventricular infarct expansion. (AP A N=Left ventricular infarct expansion) [From Erbil (Hawler) Teaching Hospital Echocardiographic Department].
No significant difference was noted in the incidence of early left ventricular infarct expansion between males (18.67%) and females (15.38%; p=0.7). (Table 1)
Table 1: Incidence of early left ventricular infarct expansion by sex and age.
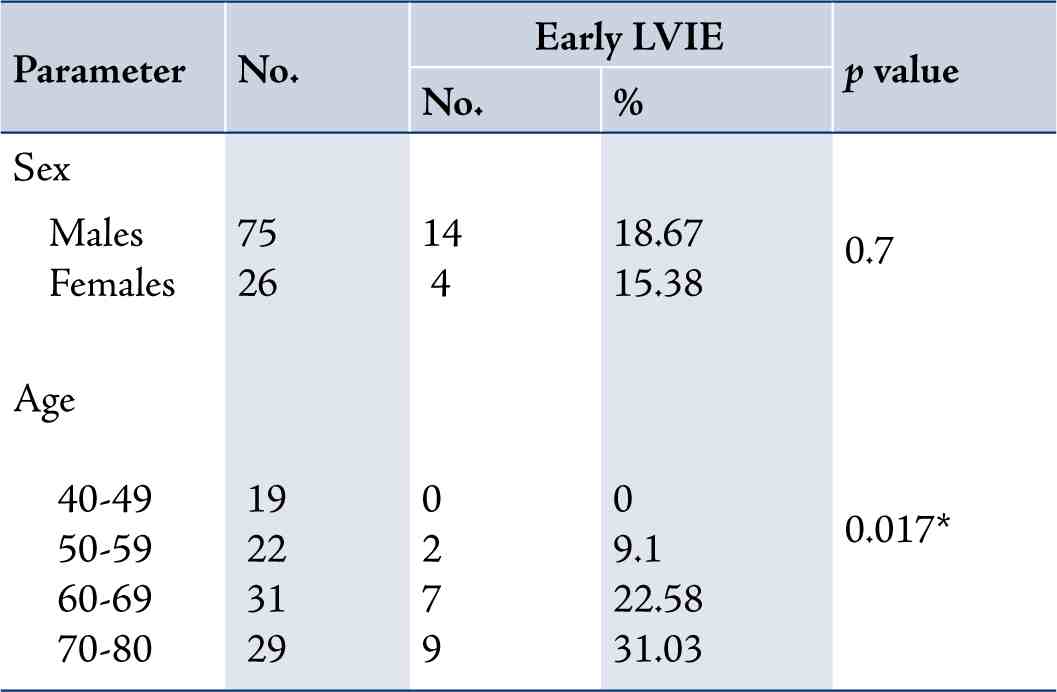
LVIE=left ventricular infarct expansion.
*= By fisher exact test
The incidence of early left ventricular infarct expansion start to increase with age, with the highest incidence between 70-80 years and no incidence of early infarct expansion was recorded between the ages of 40-49 years, as shown in Table 1.
Patients with acute anterior STEMI who received early thrombolytic therapy (alteplase) ≤3 hours of onset of pain (group I) had a significantly lower incidence of early left ventricular infarct expansion (8.16%) compared with acute anterior STEMI who received thrombolytic therapy (alteplase) >3-12 hours (group II) (26.92%; p=0.014). (Table 2)
Table 2: Comparison of early left ventricular function diagnosed by 2-D echocardiography between group I versus group II.
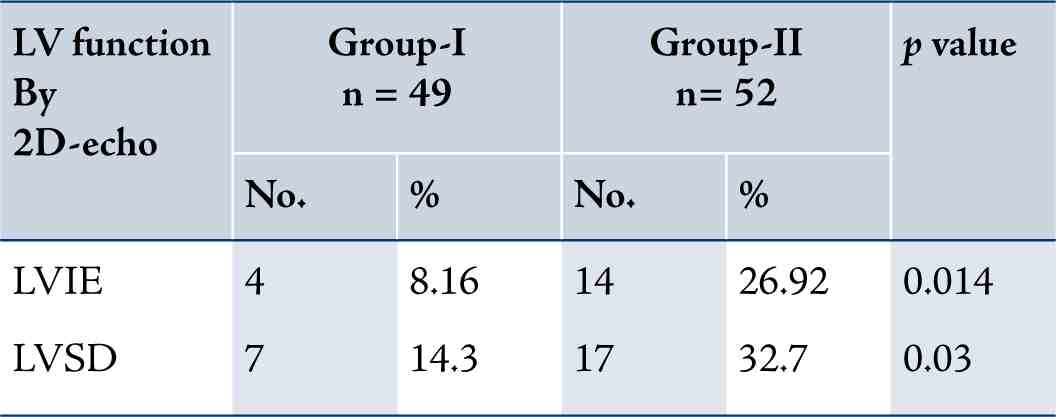
LVIE=Left ventricular infarct expansion
LVSD = left ventricular systolic dysfunction
Group I patients had a statistically significant lower incidence of left ventricular systolic dysfunction (7 patients; 14.3%) compared with group-II (17 patient; 32.7%; p=0.03), (Table 2). While patients with acute anterior STEMI with early left ventricular infarct expansion had a statistically significant higher rate of LVSD (17 patients; 94.4%) compared with patients without early left ventricular infarct expansion (7 patients; 8.4%; p=0.001). (Table 3)
Table 3: Comparison of left ventricular systolic dysfunction between those patients with early infarct expansion and those without early infarct expansion.
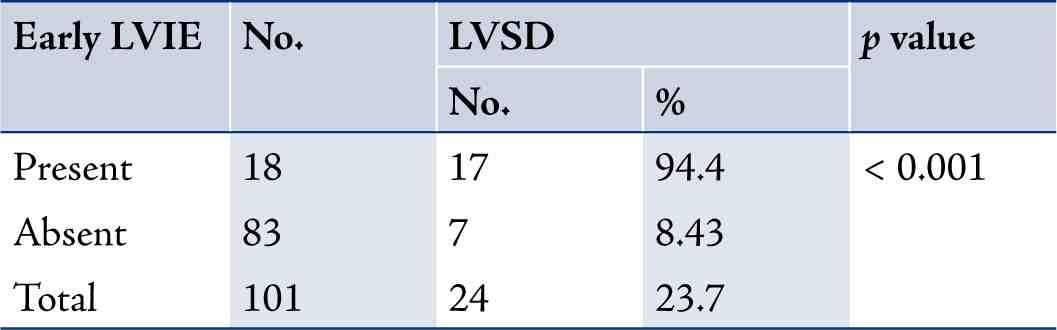
LVIE=left ventricular infarct expansion
There were no statistically significant differences in the prevalence of previous hypertension, diabetes mellitus, smoking, obesity and family history of ischemic heart disease in patients with early left ventricular infarct expansion compared with those patients without early left ventricular infarct expansion. (Table 4)
Table 4: Comparison of risk factors for IHD between those with and without early left ventricular infarct expansion.
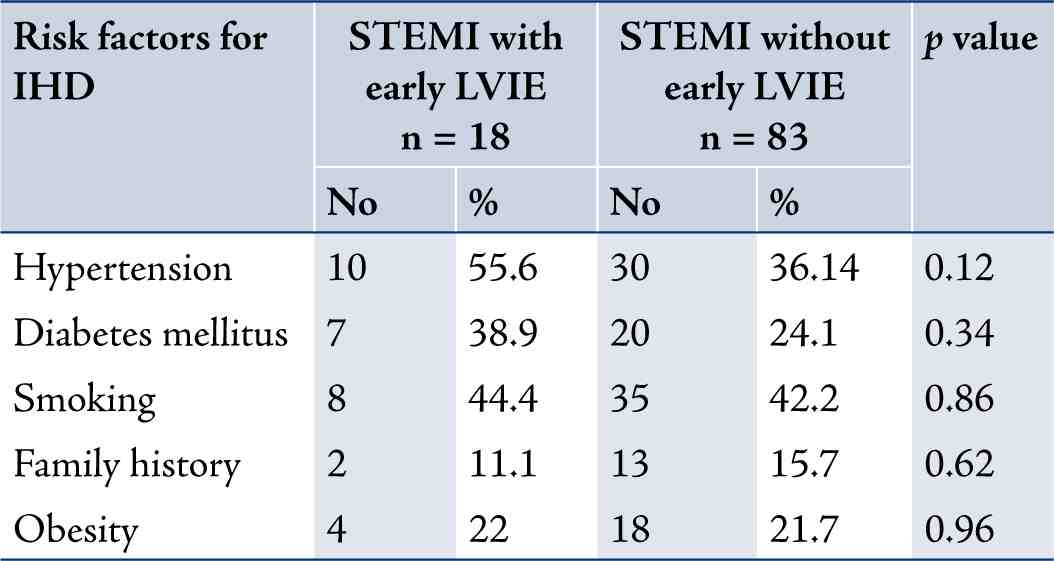
IHD=ischemic heart disease
STEMI=ST-segment elevation myocardial infarction
LVIE=left ventricular infarct expansion
Table 5: SPSS output for binary logistic regression analysis between early left ventricular infarct expansion as the dependent variable
and different covariates.
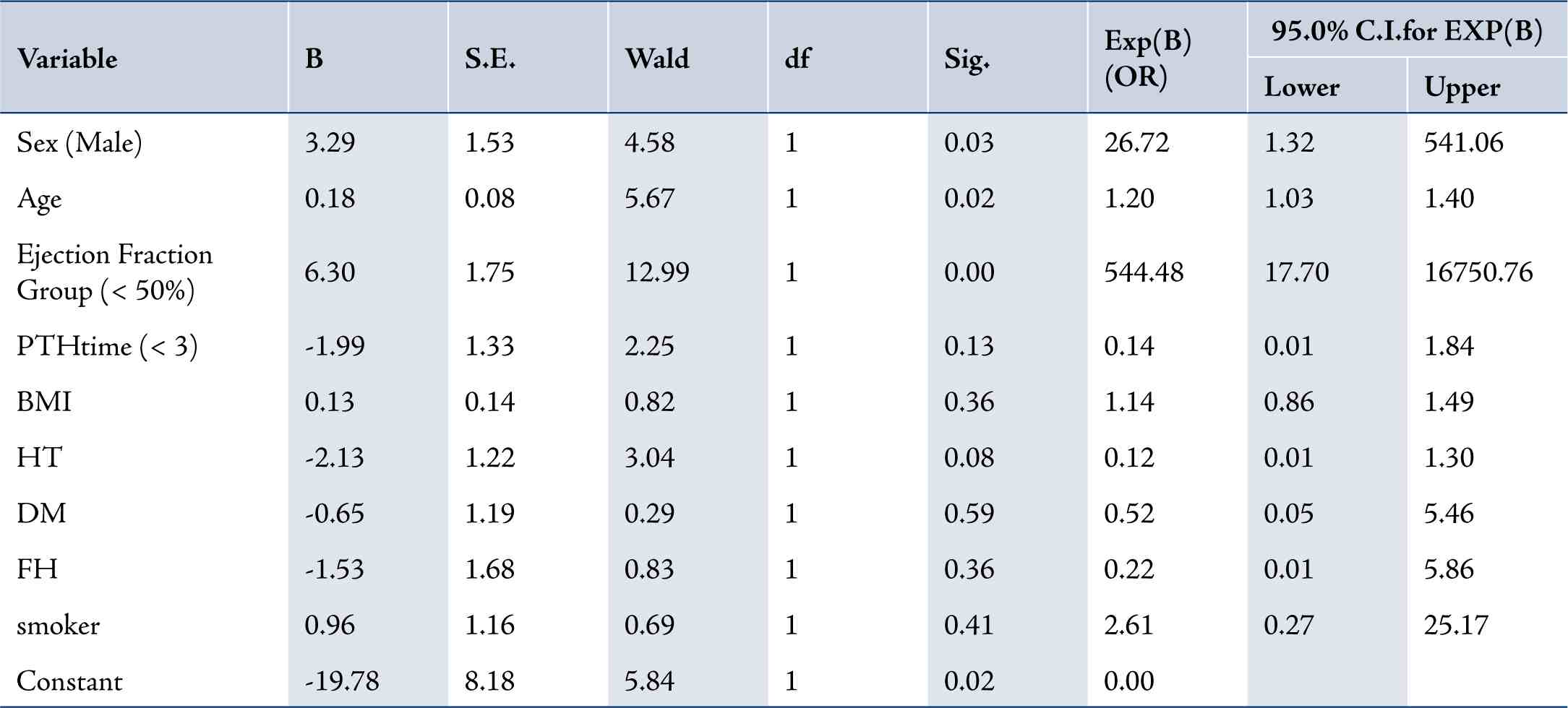
PTH=time from the onset of pain of MI till thrombolytic therapy; BMI=body mass index; HT=hypertension; DM=diabetes mellitus; FH=family history of ischemic heart disease.
Patients with ejection fraction <50% had 544 fold (Odds ratio) more risk of developing early left ventricular infarct expansion than patients with ejection fraction ≥50% (Table 5). The same table also shows that the male sex and older age are at higher risk of developing infarct expansion (p<0.05).
There was a significant difference in the prevalence of inhospital mortality between patients with acute anterior STEMI who developed early left ventricular infarct expansion (2 patient; 11.1%) compared to patients with acute STEMI without early left ventricular infarct expansion (1 patient; 1.2%; p=0.025). (Table 6)
Table 6: Comparison of in-hospital mortality between patients with early left ventricular infarct expansion and patients without early left ventricular infarct expansion.
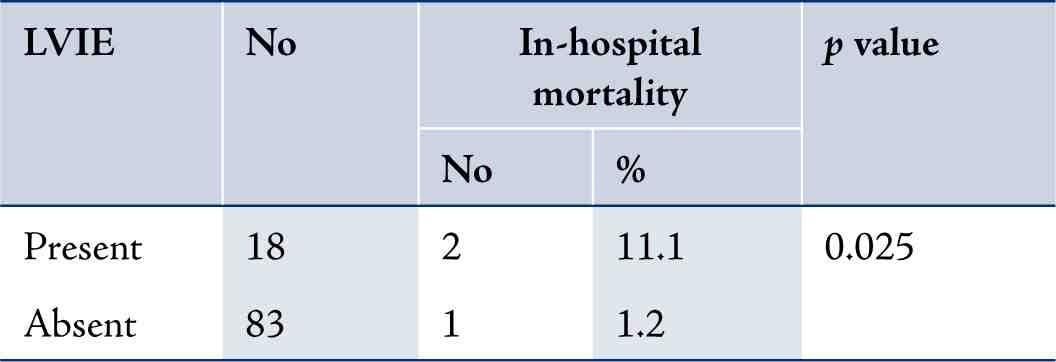
LVIE=left ventricular infarct expansion
Discussion
In our study, despite the use of thrombolytic therapy, the total incidence of early left ventricular infarct expansion reached 17.4%, but the early use of thrombolytic therapy ≤3 hours of onset of pain of acute myocardial infarction (group I) was associated with a significantly lower rate of early left ventricular infarct expansion. The angiographic substudy in GUSTO I reported that patients who received the accelerated t-PA regimen had significantly less depression of regional wall motion in the ischemic zone.16 katristis et al.17 found in their study that timely reperfusion of jeopardized myocardium represents the most effective way of restoring the balance between myocardial oxygen supply and demand, when fibrinolysis is administered, the extent of protection appears to be related directly to the rapidity with which reperfusion is implemented after the onset of coronary occlusion. Our findings are in parallel with the results of these two studies.
Group I patients had a statistically significant lower incidence (14.3%) of early left ventricular systolic dysfunction compared with group II (32.7%; p=0.03). Our results were similar to Schoming et al study who found that the improvement in global left ventricular function is related to the time of fibrinolytic treatment, with greatest improvement occurring with earliest therapy.18 The beneficial effect of reperfusion therapy for acute myocardial infarction is thought to be due to myocardial salvage, which results in improved left ventricular function and better survival.19,20
There was no statistically significant difference in the prevalence of previous diabetes mellitus in patients with early left ventricular infarct expansion compared with those without early left ventricular infarct expansion. Dini et al. concluded in their study that non insulin dependant diabetes mellitus seems to influence left ventricular remodeling associated with postinfarct total or subtotal coronary occlusion in a positive way.21 Insulin is a coronary vasodilator that plays an important role in cardiac signaling; it is possible that direct vascular effects or impaired signaling may potentiate left ventricular dysfunction in diabetic patients with acute myocardial infarction,22 nevertheless we recognize that the question of the effect of diabetes mellitus on early left ventricular infarct expansion needs to be tested in other large data based studies.
There was no significant difference in the prevalence of hypertension, smoking, obesity and family history of ischemic heart disease between patients with early infarct expansion compared with patients without early left ventricular infarct expansion. The authors did not come across a study conducted to evaluate the effect of hypertension, smoking, obesity and family history on the incidence of early left ventricular infarct expansion in patients with acute myocardial infarction.
However, there was a significant difference in the prevalence of in-hospital mortality between those patients with acute anterior STEMI who developed early left ventricular infarct expansion compared with patients with acute STEMI without left ventricular infarct expansion. Early studies have suggested a short -term in-hospital mortality rate as high as 40% for patients with early infarct expansion.9 The lower mortality rate in our patients may be explained by the low number of patients in the study.
Limitations of the study include the possibility that left ventricular infarct expansion may be manifested as a complication of old silent ischemia or old silent STEMI. Another limitation is the unavailability of contrast-enhanced magnetic resonance imaging in Erbil Teaching Hospital for more accurate assessment of the site and the extent of LV early infarct expansion in early phase of STEMI.
Conclusion
There was a high incidence of early left ventricular infarct expansion in patients with acute anterior STEMI despite the use of thrombolytic therapy, but that incidence can be greatly decreased by earliest reperfusion therapy within the first 3 hours of onset of symptoms of acute anterior myocardial infarction, and the earliest reperfusion therapy can preserve left ventricular systolic function and decrease in-hospital mortality compared with late reperfusion therapy.
Acknowledgments
The authors reported no conflict of interest. The authors would like to express my sincerest gratitude to the Nursing Staff working in
the Coronary Care Unit & Echocardiography Department of Erbil Teaching Hospital.
References
1. Visser CA, Kan G, Meltzer RS, Koolen JJ, Dunning AJ. Incidence, timing and prognostic value of left ventricular aneurysm formation after myocardial infarction: a prospective, serial echocardiographic study of 158 patients. Am J Cardiol 1986 Apr;57(10):729-732.
2. Weisman HF, Bush DE, Mannisi JA, Weisfeldt ML, Healy B. Cellular mechanisms of myocardial infarct expansion. Circulation 1988 Jul;78(1):186-201.
3. Golia G, Rossi A, Anselmi M, Prioli MA, Caraffi G, Marino P, et al. Opposite effects of the remodeling of infarcted and non-infarcted myocardium on left ventricular function early after infarction in humans. An echocardiographic study in patients examined before and after myocardial infarction. Int J Cardiol 1997 Jun;60(1):81-90.
4. Erlebacher JA, Weiss JL, Weisfeldt ML, Bulkley BH. Early dilation of the infarcted segment in acute transmural myocardial infarction: role of infarct expansion in acute left ventricular enlargement. J Am Coll Cardiol 1984 Aug;4(2):201-208.
5. Mahrholdt H, Wagner A, Judd RM, Sechtem U. Assessment of myocardial viability by cardiovascular magnetic resonance imaging. Eur Heart J 2002 Apr;23(8):602-619.
6. Kühl HP, Beek AM, van der Weerdt AP, Hofman MB, Visser CA, Lammertsma AA, et al. Myocardial viability in chronic ischemic heart
disease: comparison of contrast-enhanced magnetic resonance imaging with (18)F-fluorodeoxyglucose positron emission tomography. J Am Coll Cardiol 2003 Apr;41(8):1341-1348.
7. McKay RG, Pfeffer MA, Pasternak RC, Markis JE, Come PC, Nakao S, et al. Left ventricular remodeling after myocardial infarction: a corollary to infarct expansion. Circulation 1986 Oct;74(4):693-702.
8. Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction.Circulation 116:2634,2007.
9. Feigenbaum H, Armstrong WF, Ryan T. Coronary Artery Disease. Feigenbaum’s Echocardiography, 6th Edition,Lippincott Williams and Wilkins Company,2005.p. 437-487.
10. Ramdas G, Pravin MS. Assessment of left ventricular function. Imaging in Cardiovascular Disease.1st edition. Lippincott Williams &
Willkins.2000,p.23-41.
11. Antman EM, Braunwald E. ST-Elevation Myocardial Infarction:Management. In: Zipes DP, Libby P, Bonow RO, Braunwald E.(eds) Braunwald’s Heart Disease, 8th Edition.ELSEVIER SAUNDERS.USA,2008. p.1167-1226.
12. Bloomfiel P, Bradbury A, Grubb NR. Obesity, presenting problems of altered energy balance. Enviromental and nutritional factors in disease. In Davidson’s Principles and Practice of Medicine. 20th Edition. Churchill Livngstone, London,2006.p.111-112
13. Anderson JL. Fibrinolytic therapy of ST elevation myocardial infarction. In: Goldman L and Ausiello D,(eds). Cecil Textbook of Medicine.23rd Edition. USA.SAUNDERS ELSEVIER.2007.p.508.
14. Gersh BJ, Stone GW, White HD, Holmes DR Jr. Pharmacological facilitation of primary percutaneous coronary intervention for acute
myocardial infarction: is the slope of the curve the shape of the future? JAMA 2005 Feb;293(8):979-986.
15. Dawson B, Trapp RG. Basic & clinical biostatistics.Fourth ed.USA.Lange Medical Books/McGraw-Hill.2004.
16. The GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med 1993 Nov;329(22):1615-1622.
17. Katritsis D, Karvouni E, Webb-Peploe MM. Reperfusion in acute myocardial infarction: current concepts. Prog Cardiovasc Dis 2003 May-Jun;45(6):481-492.
18. Schömig A, Ndrepepa G, Mehilli J, Schwaiger M, Schühlen H, Nekolla S, et al. Therapy-dependent influence of time-to-treatment interval on myocardial salvage in patients with acute myocardial infarction treated with coronary artery stenting or thrombolysis. Circulation 2003 Sep;108(9):1084-1088.
19. Braunwald E. Myocardial reperfusion, limitation of infarct size, reduction of left ventricular dysfunction, and improved survival. Should the paradigm be expanded? Circulation 1989 Feb;79(2):441-444.
20. Califf RM, Topol EJ, Gersh BJ. From myocardial salvage to patient salvage in acute myocardial infarction: the role of reperfusion therapy. J Am Coll Cardiol 1989 Nov;14(5):1382-1388.
21. Dini FL, Volterrani C, Azzarelli A, Lanciani A, Lunardi M, Bernardi D, et al. Left ventricular size and function in patients with noninsulin-dependent diabetes and postinfarction total or subtotal coronary occlusions. Angiology 1998 Dec;49(12):967-973.
22. Taegtmeyer H, McNulty P, Young ME. Adaptation and maladaptation of the heart in diabetes: Part I: general concepts. Circulation 2002 Apr;105(14):1727-1733.
|