Persistent Wheeze Following ACS
Kowthar Hassan
Hassan K. OMJ. 25, 143-144 (2010); doi:10.5001/omj.2010.40
From the Department of Medicine, Sultan Qaboos University Hospital, Muscat, Sultanate of Oman.
Received:29 Dec 2009
Accepted: 07 Feb 2010
Address correspondence and reprint request to: Dr. Kowthar Hassan, Department of Medicine, Sultan Qaboos University Hospital, Muscat, Sultanate of Oman.
E-mail: kowhassan@btinternet.com
A 70 year-old hypertensive diabetic female from Muscat with a past medical history of a stroke since 9 years ago and is on lisinopril, frusemide and insulin was presented to the emergency room (ER) with dyspnoea which developed three days earlier together with cough and fever. She had attended a local health centre where she was prescribed amoxycillin and erythromycin for community acquired pneumonia. The fever and cough resolved after one day of antibiotic administration but the dyspnoea persisted. Arterial blood gases (ABGs) taken in ER showed a pH of 7.18, PaCO2: 59.9 mmHg, PaO2: 77.1 mmHg and a HCO3 of 18 mmol/L. She was started on 60% oxygen.
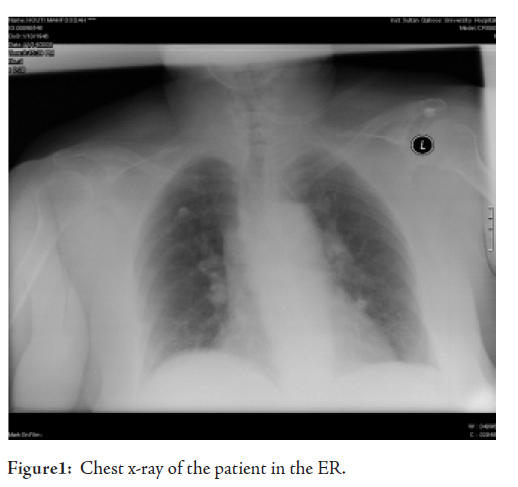
Her chest XR showed bibasal haziness assumed to be due to heart failure or community acquired pneumonia or a combination of both conditions since no BNP test was available to differentiate between the two conditions. In view of her previous CVA, her current dyspnoea and the CXR findings, a presumptive diagnosis of possible acute coronary syndrome (ACS) +/_ chest infection was made and she was started on co-amoxiclav, azithromycin, aspirin, clopidogrel, simvastatin, enoxaparin and beta blockers (BB). In addition, she received regular salbutamol nebulizers. Her ECG was not significant for ischaemia and her first troponin level was 0.15 which could have been due to slight renal impairment (creatinine 114). Indeed her second troponin was 0.13 mcg/L making the diagnois of ACS unlikely at this stage. Two hours later, her ABG were pH: 7.428, PaCO2: 36 mmHg, PaO2: 51.5 mmHg, HCO3: 24 mmol/L. The worsening PaO2 in spite of oxygen therapy was accompanied by a scattered wheeze.
The following day, the patient’s chest examination revealed inspiratory crepitations and a widespread wheeze. She desaturated to 84% on room air. An urgently requested spiral CT and D-dimers requested for a pulmonary embolism were normal. Ipratropium nebulizers and three times daily hydrocortisone 100mg were commenced but her condition remained unchanged and her oxygen saturation continued to drop to 85% within 10-15 min of stopping oxygen therapy. Immediately after nebulizer inhalation, her chest would be clear but a loud wheeze would return 10 minutes later.
What is the likely cause of her wheeze and desaturation?
a. pneumonia
b. heart failure
c. ACS
d. drug-induced
e. chronic bronchitis
d. drug-induced bronchospasm.
The cardiology consultant decided to stop her aspirin and BB in view of her continuing wheeze. Two days later, the patient was sitting comfortably on her bed not requiring oxygen or nebulizer therapy. It became obvious that either aspirin or her BB or both were responsible for her bronchospasm.
DISCUSSIONA number of drugs have been reported to induce bronchospasm.1, 2 Analysis of cases of drug-induced bronchospasm reported from 1986 to 1995 to the Swiss Drug Monitoring center showed that up to 186 of different drugs could induce bronchospam.2 Analgesics and non-steroidal anti-inflammatory agents (NSAIDs) were reported most frequently (24%), aspirin in 15.5% of cases, paracetamol in 8.9% and various drugs accounted for 6.8%.2
In this case, the drugs which were administered for possible ACS, not only confused the picture of the initial diagnosis, but also lead to a problem on their own merit. Drug-induced bronchospasm can be overlooked in cases where the initial problem is not very clear. It would appear that in this report, the patient did indeed start with community acquired pneumonia, but she soon afterwards sought medical help at the ER unit where the diagnosis was immediately obscured by the initiation of aspirin. Sodium cromoglycate has been shown to reverse bronchospasm induced by aspirin.3 Indeed in the study patient, the wheeze cleared immediately following the use of nebulizers but the wheezing recurred approximately 10 minute later. It may have been of some value to re-challenge her with aspirin and BB separately to determinate which drug was the culprit. This however, was not done as there was no necessity for a patient of her age. Instead, she was given clear information both verbally and written to avoid the above drugs, was started on diltiazem in place of BB and was discharged home.
ACKNOWLEDGEMENTS
The author reported no conflict of interest and no funding was received on this work.
REFERENCES
-
Barnes PJ: Drug-induced asthma; in Barnes PJ, Grunstein MM, Leff AR, Woolcock AJ (eds): Asthma. Philadelphia, Lippincott-Raven, 1997, pp 1245-1249. .
Jörg D. Leuppia, Pia Schnydera, Katharina Hartmannb, Walter H. Reinharta, Max Kuhna,b .Drug-Induced Bronchospasm: Analysis of 187 Spontaneously Reported Cases Respiration 2001;68:345-351.
-
A. Basomba1 , A. Romar , A. Peleaz , I. G. Villalmanzo A. Campos. The effect of sodium cromoglycate in preventing aspirin induced bronchospasm. Clinical & Experimental Allergy. Volume 6 Issue 3 : 269-275