|
Abstract
Objective: Cesarean rates in recent decades have been increasing and a number of studies have shown that cesarean increases maternal morbidities. The aim of this study is to compare the quality of life after cesarean and vaginal delivery.
Methods: This prospective study was carried out on 356 pregnant women visiting urban health centers in Shahroud City, Northeast Iran, in 2011. The subjects completed the quality of life questionnaire in the third trimester of pregnancy and at 8 weeks postpartum.
Results: In primiparas, the mean global QOL scores for the cesarean and vaginal delivery groups were 67.65 ± 12.7 and 72.12 ± 11.8, respectively. Also, the scores for the physical, psychological and social domains of QOL as well as the global score of QOL were higher in the vaginal delivery group than the cesarean group (p<0.05). In the case of primiparas, multiple regression analysis revealed that after adjusting for education, desirability of pregnancy and the General Health Questionnaire score, the delivery type remained as a predictor of the scores for the physical (R2=1.7%; B=-3.826; p=0.031; CI [-7.301, -.350]) and social (R2=2.5%; B=-5.708; p=0.017; CI [-10.392, -1.023]) domains of QOL and the global QOL score (R2=2.6%; B=-4.065; p=0.006; CI [-6.964, -1.164]). While multiparas, there was no relationship between QOL and type of delivery.
Conclusion: In this sample of low-risk women, cesarean negatively affected the QOL of primiparas. More studies with larger sample sizes should be conducted to examine the effects of cesarean on QOL in both primiparas and multiparas within a shorter period after delivery.
Keywords: Quality of Life; Cesarean; Pregnant women; Postpartum period.
Introduction
With the declining maternal mortality rates and general improvement in pregnancy outcomes in recent decades, the aims of maternity care in developed countries have now expanded to areas beyond the mere detection and management of risk factors which threaten the outcome of pregnancy. One of the components of this broadened view of maternity care has been the adoption of enhancement in quality of life (QOL) as one of the aims of prenatal and postnatal care.1 As a result, many studies have been undertaken to investigate the effects of pregnancy and delivery outcomes on maternal QOL.2
According to World Health Organization (WHO) recommendations, the reasonable rate for cesarean is 5-15% of all deliveries performed. Rates more than 15% are considered inappropriate and unnecessary and do not produce better health outcomes.3 In most countries, and in developing countries in particular, it has been continuously rising and has gone well beyond the WHO recommendations, without being accompanied by any decline in maternal mortality or morbidity rates.4 The same trend has been affecting Iran in recent decades. Another study in 1999 reported cesarean rates of 14.9-39.2% in 6 teaching hospitals and 87.4% and 78.5% in 2 private hospitals in Tehran.5 Overall, the rate of cesareans in Iran increased from 35.4% of deliveries in 1999 to 42.3% in 2003.6
A number of studies on cesareans have reported increased risk of maternal morbidities such as; hysterectomy, hemorrhage, infection, thrombosis and postpartum depression.7 Also, results of some studies indicate that symptoms such as fatigue, headache, lack of sleep, anemia, urinary infection and other conditions needing treatment in the first 8 weeks after delivery are higher in women who delivered by cesarean section than those who underwent vaginal delivery (VD).8,9 It is evident that the experience of pain and fatigue can negatively affect QOL after birth.10 Despite the extent of postnatal morbidity, there are only a limited number of studies comparing quality of life of new mothers after different modes of delivery and even studies on ante-and postnatal quality of life in general are rare.1 In a study in Iran comparing the quality of life of women after VD and cesarean at two weeks postpartum, the cesarean group had lower scores for the mental and physical subscales of QOL compared with the vaginal delivery group.11 However, the above studies did not consider factors such as parity or age which can affect QOL. Also, they did not compare the QOL between the two groups in the antenatal period to ensure that the groups are equal, which would be of value in case there was no difference in QOL between the two groups in postpartum period. Considering the WHO’s emphasis on abandoning a merely "mechanistic model of medicine",12 and its initiative in developing WHOQOL-BREF instrument,13 it is surprising to find only a small number studies based on the quality of life during pregnancy or postpartum using this instrument. Therefore, the present prospective study attempts to investigate and compare quality of life between women having either cesarean or vaginal deliveries using WHOQOL-BREF instrument. Also, we divided the women into groups according to parity in order to examine how the mode of delivery affects the QOL in primiparas and multiparas.
Methods
This study is part of a longitudinal study, which was started in May, 2011 in 10 urban health centers affiliated with Shahroud University of Medical Sciences, Iran. Ethics Committee of Shahroud University of Medical Sciences approved the study protocol (Approval No. 900.02). A total of 370 women who attended Shahroud health centers for prenatal care and met the inclusion criteria were selected using non-probability sampling method of which 356 were accepted to participate in the study and gave informed consent and 340 were followed up until 8 weeks postpartum. The inclusion criteria were; gestational age more than 28 weeks, delivering a live and healthy baby and absence of major psychological and medical problems (e.g., depression, disabilities and drug intake). The exclusion criteria were; infant death during 8 weeks postpartum and acute stressful events during the course of study (e.g., lose of a family member or divorce). After explaining the aims of the study and obtaining written consent from participants, they were given instructions on how to complete the WHOQOL-BREF questionnaire. To preserve participant anonymity, all the questionnaires were given to participants in an envelope to cover the questionnaire after completing it. Midwives at the health centers were responsible for distributing and gathering questionnaires. The sample size for this study was calculated to be 312 based on the results of a previous study in Iran,11 in which the mean values of global QOL score as measured by WHOQOL-BREF between cesarean and vaginal delivery were 76.56±14.04 and 77.83±14.36, respectively.
An interview form consisting of personal (age, education level, employment status, family income, housing type) and obstetrical information (parity, desirability of pregnancy, infant birth weight, infant feeding method, pregnancy complications, mode of delivery), as well as postpartum morbidities including sore nipples, cracked nipples, breast engorgement, breast infection, feeling very tired, feeling tense and overwhelmed, and low sexual desire was completed during the third trimester of pregnancy and at the first postpartum visit. Information related to the cause and the nature of cesarean (elective versus emergency) was gathered by searching the women’s medical records at the two hospitals.
The participants completed the WHOQOL-BREF questionnaire in the third trimester of pregnancy and at 8 weeks postpartum. The WHOQOL-BREF was developed by the World Health Organization as a shortened version of the WHOQOL-100 instrument. It contains 26 questions. Two questions are based on the individual’s overall perception of quality of life and health and 24 questions concern four subscales: Physical, Psychological, Social Relationships and Environment.13 The items are rated on a 5-point Likert scale. The raw subscale scores converted to a 0-100 scale. Higher scores mean a better quality of life. The validity and reliability of Iranian translation of WHOQOL-BREF was investigated in a previous study which indicated that all its domains met the minimum reliability standards (Cronbach's alpha and intra-class correlation >0.7), except for social relationships (alpha = 0.55). It also reported that it discriminated well between subgroups of the study samples differing in their health status and demonstrated statistically significant correlation with the Iranian version of the SF-36.14 The validity of the questionnaire among women in the postpartum period has also been supported.15
The GHQ28 has been regularly used for screening various groups including women in ante-and postnatal periods.16 The GHQ contains 28 questions in four domains: somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression. Each domain has seven items, which have a 4-point scoring system from zero to three based on a 4-point Likert scale. The validity and reliability of the Persian version of GHQ has been confirmed in previous studies. The cut-off point in Iran has been calculated at 24.17,18
Statistical analysis was performed using SPSS 12 (SPSS Inc., Chicago, IL, USA). Chi-square and t-test were done to compare women’s characteristics between the two groups, Mann-Whitney-u test was performed to compare the QOL scores between the two groups in the ante-and postnatal periods. Univariate regression analyses were performed to examine the relationship between QOL scores and other variables. Multiple regression analysis was used to examine the relationship between QOL scores and delivery mode. All variables listed in Table 4, which were related to the QOL score with p<0.25 in both primiparas and multiparas, were further put into a multiple regression analysis to examine the relationship between the QOL score and thype of delivery after adjusting for the variables that remained in the equations.19 The internal consistency of the questionnaire was examined using Alpha Cronbach coefficient. The significance level of tests was set at 0.05.
Results
Shahroud is a small city in northeast of Iran. It has 10 public health centers and 2 public hospitals, one is a general hospital and the other a maternity hospital in which all the participants in the study gave birth. The characteristics of the women in the cesarean and VD groups are compared in Table 1. Mean age of women was 26.17±4.42 with age ranging from 15 to 42 years. Median monthly income of the household was 4 million RLS.
The median years of education was 12 ranging from 4-21. The mode of delivery for 53% of the sample was cesarean. Also, 42% of the cesareans were done on multiparas of whom 29.7% were repeat cesareans. Elective and emergency cesareans comprised 32% and 10% of all cesareans, respectively. In addition, 58% of cesareans were done on primiparous women of whom 32% and 26% were elective and emergency cesareans respectively. All cases were lower segment cesarean sections.
The values of Alpha Cronbach coefficient for the whole WHOQOL-BREF questionnaire in the antenatal and postpartum periods were, respectively: 0.92 and 0.93. While the comparison of two groups showed that there was no significant difference between the two groups in all variables except in women’s age (p=0.005), family income (p=0.007), pregnancy complications (p=.005), and mothers’ rehospitalization in early postpartum (p=0,043). Women of the cesarean group were older, had higher family income, pregnancy complications and rehospitalization in early postpartum. Also, we found that cesarean affected QOL of primiparas and multiparas differently.
We checked some morbidities in the postpartum period. There were no significant differences between the two groups with regard to sore nipples (p=0.131), cracked nipples (p=0.942), breast engorgement (p=0.988), breast infection (p=0.071), feeling very tired (p=0.698), feeling tense and overwhelmed (p=0.970), and low sexual desire (p=0.057). GHQ28 was used to investigate the ante-and postpartum psychological state of the women. There was no difference between the two groups with regard to the presence of ante-and postpartum psychological problems.
Table 2 shows the scores obtained by the two groups in all the subscales of the WHOQOL-BREF in the ante- and postnatal period. Analyzing all the items of the questionnaire individually showed that the scores obtained by the two groups for all questions were not significantly different, except for the scores obtained by the vaginal delivery group for Q11 which belongs to the psychological domain (Are you able to accept your bodily appearance?) and Q21 from the social relationship domain, (How satisfied are you with your sex life?), which were significantly higher (p=0.037).
In Table 3, the cesarean and vaginal delivery groups were classified according to parity and their scores in the four QOL domains in postnatal period were compared.
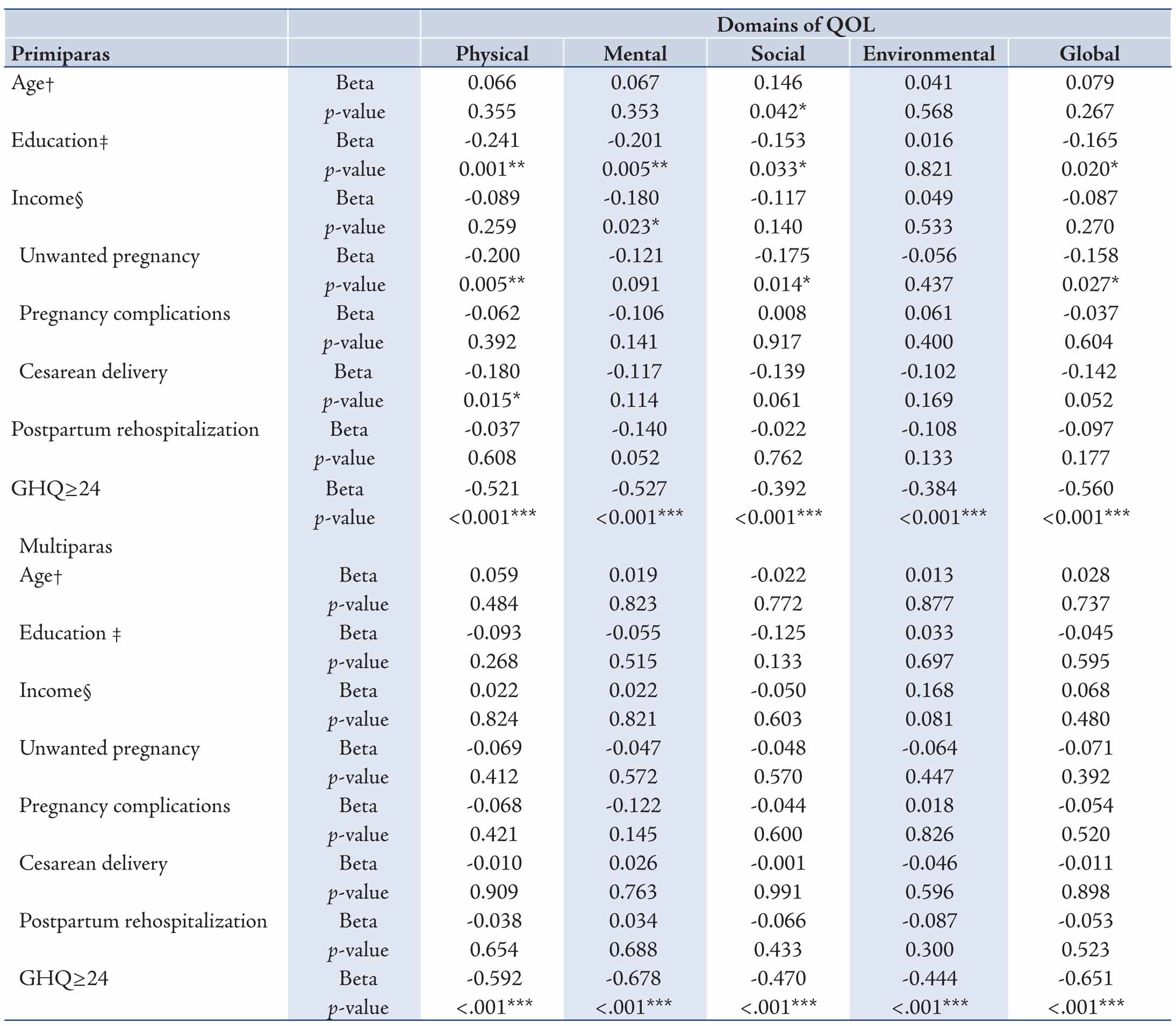
The results of the univariate regression analyses of QOL global and domain scores in the postpartum on some variables are presented in table 4. In multiparas, there was no relationship between the QOL and type of delivery. Also, we could not detect any significant relationship between the QOL and other variables in this group, except for the postnatal GHQ28 score. In primiparas, multiple regression analysis revealed that after adjusting for education, desirability of pregnancy, the GHQ28 score, and the type of delivery (vaginal delivery=0; cesarean=1) remained as a predictor of the score for the physical domain of QOL (R2=1.7%; B= -3.826; p=0.031; CI [-7.301, -0.350]). In addition, after adjusting for the GHQ28 score, the type of delivery remained as a predictor of the score for the social domain of QOL (R2=2.5%; B=-5.708; p=0.017; CI [-10.392, -1.023]). Finally, after adjusting for desirability of pregnancy and the GHQ28 score, the type of delivery remained as a predictor of the global QOL score (R2=2.6%; B=-4.065; p=0.006; CI [-6.964, -1.164]). In each domain, other variables which were associated with QOL with p<0.25 were excluded from the equations.
Table 1: Sociodemographic characteristics of the women in the two groups.
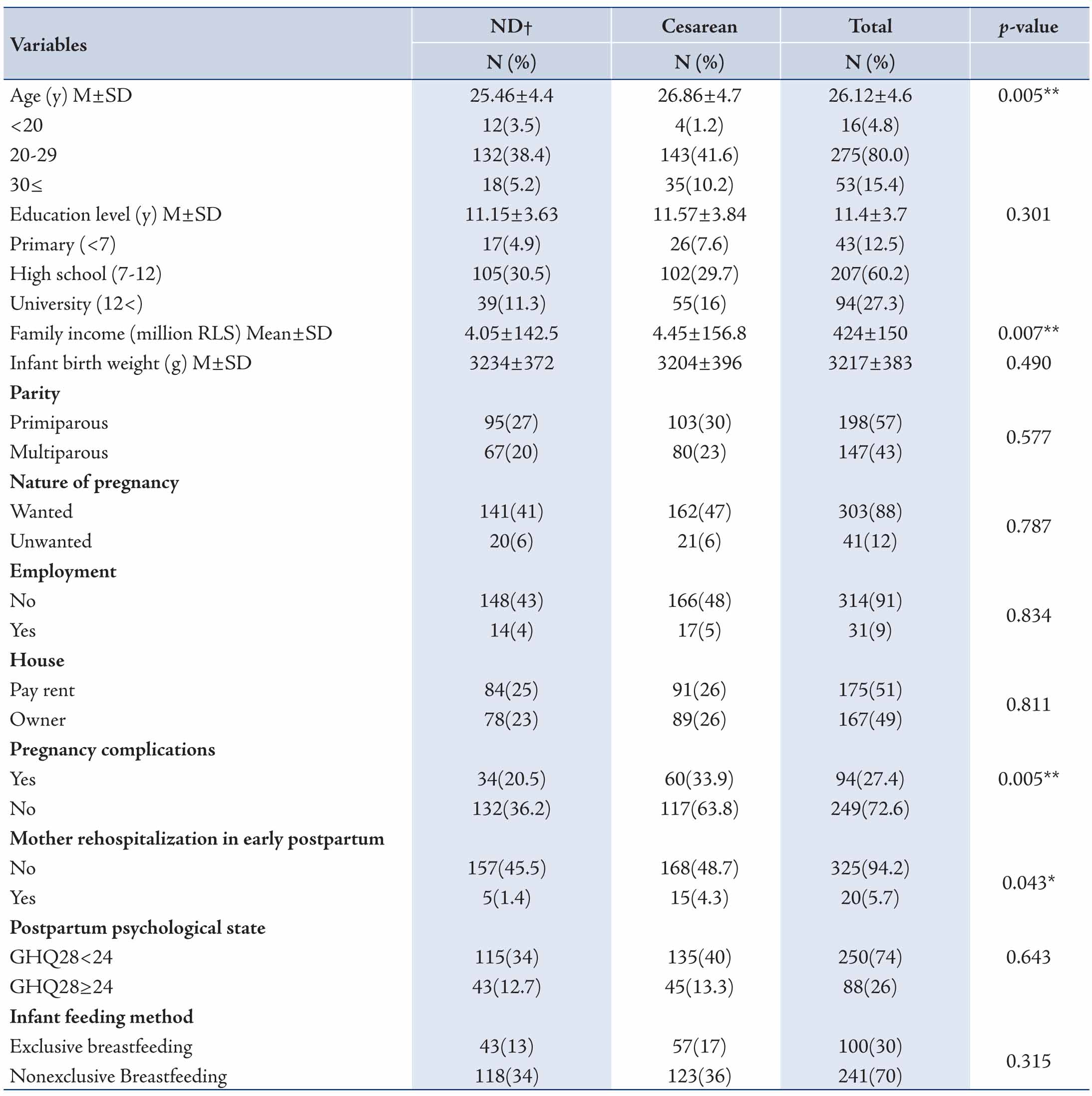
Table 2: Means and standard deviations of QOL in the third trimester of pregnancy and postpartum based on delivery mode.
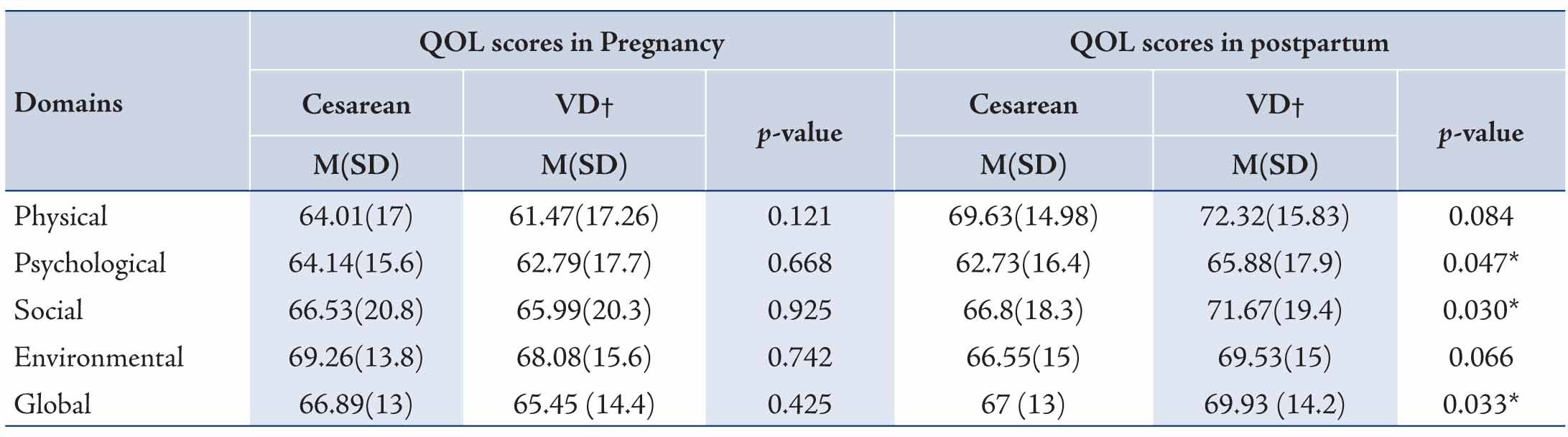
Table 3: Comparison of the scores between the cesarean and vaginal delivery groups in QOL domains in postnatal period based on parity.
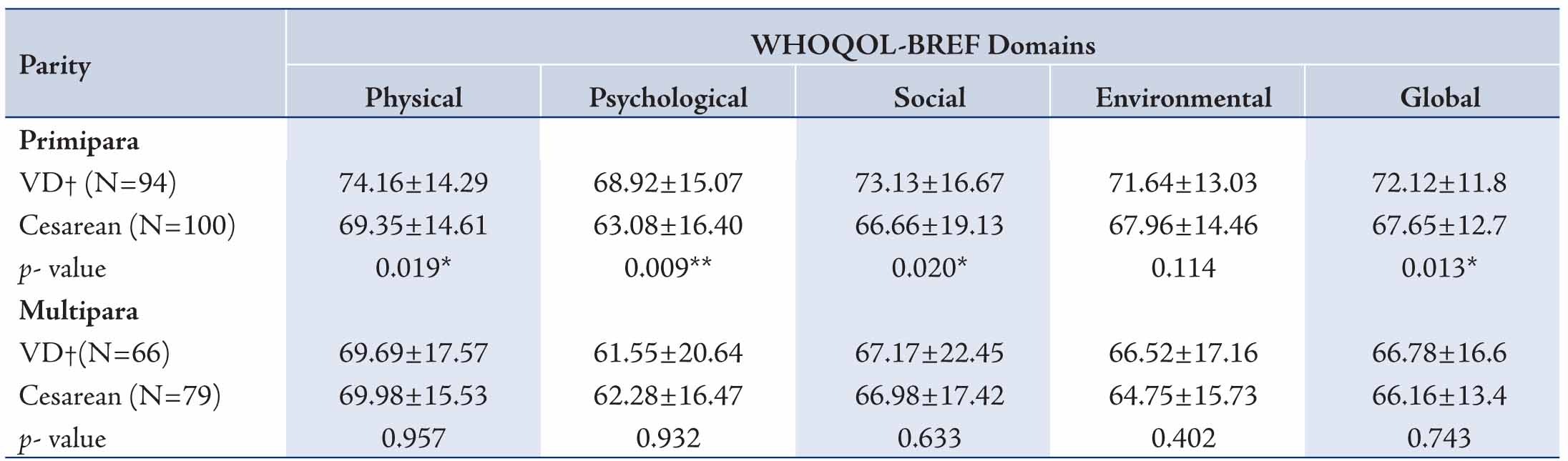
Table 4: Univariate regression analyses of QOL global and domain scores in the postpartum on some variables.
Discussion
The WHOQOL-BREF was used in the present study to compare QOL in the ante- and postnatal periods in women with caesarean and VD. Results of the present study indicate that in primiparous women, physical and social domain scores as well as the global score of QOL are negatively influenced by cesarean. In contrast, cesarean did not affect the QOL of multiparous women. An explanation may be provided by considering the fact that in our study 42% of cesareans were done on multiparous women of whom 30% were repeat cesareans and 10% were emergency cesareans. These percentages strongly suggest that 90% of cesareans in multiparas are planned cesareans which are executed prior to labor while the primiparous were more likely to have emergency cesareans (26%), performed during labor by necessity, due to maternal or fetal indications. As a result, 26% of primiparous women who had no prior birth experience, experienced stress and pain during the course of vaginal delivery and eventually gave birth by cesarean. Results of one study indicated that the average period to reach full physical recovery was 3 weeks after VD, 6 weeks after elective cesarean, and >6 weeks after emergency cesarean.20 Also, it is likely that the difference in the quality of life between the VD and cesarean groups in both primiparas and multiparas would have been more pronounced at some point closer to childbirth, such as two weeks postpartum. Additionally, the low percentage of multiparous women who underwent emergency cesarean may be responsible for the fact that we did not find any significant difference between the cesarean and vaginal delivery groups in their case.
In our study, the VD group was more satisfied with their sexual lives and bodily appearance in the postnatal period. Results of a systematic review on postpartum sexual function outcomes reported that short-term postpartum sexual problems are highly prevalent, ranging from 22% to 86%. Some of the studies have found no differences in sexual function between women with cesarean and those with VD.21
According to other studies at two and eight weeks postpartum, women with VD exhibited higher scores in the psychological domain of QOL than women with cesarean, but there were no significant differences in the social domain of QOL between the two groups at either two or eight weeks postpartum.11,22 In a study in Iran, the VD group had significantly better scores in the vitality and mental health subscales of the Short Form Health Survey (SF-36) at two months postpartum.23 But results of a review showed that there was no evidence indicating delivery by caesarean increased the risk of postpartum depression.24
We found that women in the VD group had less rehospitalization in early postpartum than the cesarean group. A study that compared sleep and fatigue in mothers during early postpartum reported less hospitalization and more total sleep time in the vaginal birth group than the caesarean group.25 Also, women in the cesarean group were older, had higher family incomes and had more complications during pregnancy. These findings are in line with the findings of an Omani study.26
The finding of the present study contributes to our understanding of the relationship between the mode of delivery and QOL and the role of parity in this relationship. Considering the high rate of cesarean (53%) in two public hospitals in a small city like Shahroud, it is clear that the problem calls for a comprehensive approach. Hopefully, the findings of the present study may be of help to healthcare policy makers in devising policies to control the cesarean rate in Shahroud. We examined the QOL of women at 8 weeks postpartum, we recommend that further studies be designed to examine the QOL of women within a shorter period of time after delivery such as 2 or 4 weeks postpartum and with samples containing higher number of women with emergency cesarean.
This study used the WHOQOL-BREF to evaluate the quality of life, an instrument which is not specifically designed for pregnant women. However, a previous study comparing The Mother-Generated Index (MGI) with the WHOQOL-BREF has reported a strong correlation between the two questionnaires.27
Since our sample consisted of all pregnant women attending Shahroud health centers, and considering the fact that antenatal care coverage of at least once and at least four times have been reported for 98% and 94% of women, respectively in Iran in 2006-2010,28 the study sample is representative. However, any generalization of the findings of this study must take into account the limitations posed by its sample size. The sample size of the study is not sufficient to conclude that cesarean does not affect the QOL of multiparas. It is possible that a study with a sample containing a higher number of multiparas with emergency cesarean would lead to different results. Also, considering the various variables which affect the QOL, our results might have been different in the case primiparas too.
Conclusion
In this sample of low risk women, cesarean affected the physical and social domain scores, as well as the global score of QOL of primiparas negatively. In view of the wide range of variables which might influence the QOL, more studies with higher sample sizes should be done to examine the effects of cesarean on QOL of both primiparas and multiparas within a shorter period of time after delivery.
Acknowledgements
The study was resulted from a PhD thesis, which was approved by review board of Shahroud University of Medical Sciences (Approval No. 9004) and was conducted with the financial help of research committee of Shahroud University of Medical Sciences. The authors wish to thank all midwives and participants who made this study possible.
References
1. Symon A. A review of mothers’ prenatal and postnatal quality of life. Health Qual Life Outcomes 2003;1:38.
2. Couto ER, Couto E, Vian B, Gregório Z, Nomura ML, Zaccaria R, et al. Quality of life, depression and anxiety among pregnant women with previous adverse pregnancy outcomes. Sao Paulo Med J 2009 Jul;127(4):185-189.
3. Appropriate technology for birth. Lancet 1985 Aug;2(8452):436-437.
4. McCourt C, Weaver J, Statham H, Beake S, Gamble J, Creedy DK. Elective cesarean section and decision making: a critical review of the literature. Birth 2007 Mar;34(1):65-79.
5. Garmaroudi G, et al. Caesarean section and related factors in Tehran, Iran. Payesh 2002;1:45-49. in Persia.
6. Ahmad-Nia S, Delavar B, Eini-Zinab H, Kazemipour S, Mehryar AH, Naghavi M. Caesarean section in the Islamic Republic of Iran: prevalence and some sociodemographic correlates. East Mediterr Health J 2009 Nov-Dec;15(6):1389-1398.
7. Villar J, Carroli G, Zavaleta N, Donner A, Wojdyla D, Faundes A, et al; World Health Organization 2005 Global Survey on Maternal and Perinatal Health Research Group. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ 2007 Nov;335(7628):1025.
8. Borders N. After the afterbirth: a critical review of postpartum health relative to method of delivery. J Midwifery Womens Health 2006 Jul-Aug;51(4):242-248.
9. Thompson JF, Roberts CL, Currie M, Ellwood DA. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth 2002 Jun;29(2):83-94.
10. Scolt J, Gibbs R. karlan B, Hakey A. Danforth,s obstetrics and gynecology. Philadelphia, Lippincott Williams and Wilkins, 2003.
11. Abedian Z, et al. Evaluation of Relationship between Delivery Mode and Postpartum Quality of Life. Obstetrics, Gynaecology and infertility. 2010, 13:47-53 (in Persia).
12. WHO definition of Health, World Health Organization. 1984 [cited 2012 Aug 2]; Available from: www.who.int/about/definition/en/print.html
13. World health organization: programme on mental health. WHOQOL- BREF - introduction, administration, scoring and generic version of the assessment. Geneva, World health organization, 1996 [cited 2012 July 25]; Available from: www.who.int/mental_health/media/en/76.pdf
14. Nedjat S, Montazeri A, Holakouie K, Mohammad K, Majdzadeh R. Psychometric properties of the Iranian interview-administered version of the World Health Organization’s Quality of Life Questionnaire (WHOQOL-BREF): a population-based study. BMC Health Serv Res 2008;8:61.
15. Webster J, Nicholas C, Velacott C, Cridland N, Fawcett L. Validation of the WHOQOL-BREF among women following childbirth. Aust N Z J Obstet Gynaecol 2010 Apr;50(2):132-137.
16. Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Arch Womens Ment Health 2005 Sep;8(3):141-153.
17. Ebrahimi A, Molavi H, Moosavi G, Bornamanesh A, Yaghobi M. Psychometric Properties and Factor Structure of General Health Questionnaire 28 (GHQ-28) in Iranian Psychiatric Patients. Journal of Research in Behavioural Sciences 2007;5:5-11. in Persia.
18. Noorbala AA, Mohammad K, Bagheri Yazdi SA, et al. Validation of GHQ-28 in Iran. Hakim Magazine 1999;5:101-110.
19. Hosmer D, Lemeshow S. Applied Logistic Regression, New York, John Wiley Inter science publications, 1989.
20. Jansen AJ, Duvekot JJ, Hop WC, Essink-Bot ML, Beckers EA, Karsdorp VH, et al. New insights into fatigue and health-related quality of life after delivery. Acta Obstet Gynecol Scand 2007;86(5):579-584.
21. Hicks TL, Goodall SF, Quattrone EM, Lydon-Rochelle MT. Postpartum sexual functioning and method of delivery: summary of the evidence. J Midwifery Womens Health 2004 Sep-Oct;49(5):430-436.
22. Nikpour M, et al. comparison of quality of life in women after vaginal delivery and cesarean section. J Babol Univ Med Sci 2011;13:44-50. in persia.
23. Torkan B, Parsay S, Lamyian M, Kazemnejad A, Montazeri A. Postnatal quality of life in women after normal vaginal delivery and caesarean section. BMC Pregnancy Childbirth 2009;9:4.
24. Carter FA, Frampton CM, Mulder RT. Cesarean section and postpartum depression: a review of the evidence examining the link. Psychosom Med 2006 Mar-Apr;68(2):321-330.
25. Lee SY, Lee KA. Early postpartum sleep and fatigue for mothers after cesarean delivery compared with vaginal delivery: an exploratory study. J Perinat Neonatal Nurs 2007 Apr-Jun;21(2):109-113.
26. Al Busaidi I, Al-Farsi Y, Ganguly S, Gowri V. Obstetric and non-obstetric risk factors for cesarean section in oman. Oman Med J 2012 Nov;27(6):478-481.
27. Zubaran C, Foresti K, Schumacher MV, Muller LC, Amoretti AL. An assessment of maternal quality of life in the postpartum period in southern Brazil: a comparison of two questionnaires. Clinics (Sao Paulo) 2009;64(8):751-756.
28. UNICEF. Iran, Islamic Republic of - Statistics. 2011 [Cited 2012 Oct 4]; Available from: www.unicef.org/infobycountry/iran_statistics.html
|