|
An Emergency Medical Service (EMS) can be defined as “a comprehensive system which provides the arrangements of personnel, facilities and equipment for the effective, coordinated and timely delivery of health and safety services to victims of sudden illness or injury.”1 The aim of EMS focuses on providing timely care to victims of sudden and life-threatening injuries or emergencies in order to prevent needless mortality or long-term morbidity. The function of EMS can be simplified into four main components; accessing emergency care, care in the community, care en route, and care upon arrival to receiving care at the health care facility.2
Today’s global EMS has advanced so much that it contributes widely to the overall function of health care systems. The World Health Organization regards EMS systems as an integral part of any effective and functional health care system.3 It is the first point of contact for the majority of people to health care services during emergencies and life-threatening injuries and act as a gate-keeping step for accessing secondary and tertiary services. Emergency medical providers around the world have developed an extended role to deal with medical and trauma emergencies utilizing advanced clinical technology. In many countries where proper EMS system exists, providers can administer controlled medications such morphine and epinephrine, perform invasive procedures for instance, endotracheal intubation and placement of intravenous line, and make complex clinical judgment or even pronounce death.4,5 The rapid development of medical technology has also reformed the international EMS systems with the introduction of multifunctional compact monitoring systems making the task of monitoring patients manageable in an uncontrolled environment of pre-hospital settings.
Since 1970s, the mode of emergency health care delivery in pre-hospital environment evolved around two main models of EMS with distinct features. These are the Anglo-American and the Franco-German model. These categorical distinctions were obvious during the 1970s until the end of the 20th century. Today, most EMS systems around the world have varied compositions from each model.
The delivery of emergency medical services in pre-hospital settings can be categorized broadly into Franco-German or Anglo-American models according to the philosophy of pre-hospital care delivery. Another method of EMS classification is according to the level of care provided into Basic Life Support and Advanced Life Support according to the level of care provided.1
The Franco-German model of EMS delivery is based on the “stay and stabilize” philosophy.6 The motive of this model is to bring the hospital to patients. It is usually run by physicians and they have extensive scope of practice with very advanced technology. The model utilizes more of other methods of transportations alongside land ambulance such as helicopters and coastal ambulances.7 This model is usually a sub-set of the wider health care system. This philosophy is widely implemented in Europe in which emergency medicine is relatively a young field.8 Therefore in Europe, pre-hospital emergency care is almost always provided by emergency physicians. The attending emergency doctors in the field have the authority to make complex clinical judgment and treat patients in their homes or at the scene. This results in many EMS users being treated at the site of incident and less being transported to hospitals. The very few transported patients are usually directly admitted to hospital wards by the attending field emergency medicine physician bypassing the emergency department. Countries such as Germany, France, Greece, Malta and Austria have well-developed Franco-German EMS systems.9-13
In contrast to the Franco-German model, the Anglo-American model is based around “scoop and run” philosophy.7 The aim of this model is to rapidly bring patients to the hospital with less pre-hospital interventions. It is usually allied with public safety services such as police or fire departments rather than public health services and hospitals.14 Trained paramedics and Emergency Medical Technicians (EMTs) run the system with a clinical oversight. It relies heavily on land ambulance and less so on aero-medical evacuation or coastal ambulance. In countries following this model, emergency medicine is well-developed and generally recognized as a separate medical specialty. Almost all patients in the Anglo-American model are transported by EMS personnel to developed Emergency Departments rather than hospital wards. Countries which use this model of EMS delivery include the United States, Canada, New Zealand, Sultanate of Oman and Australia.14-18
Table 1: Comparison between Franco-German model and Anglo-American model.
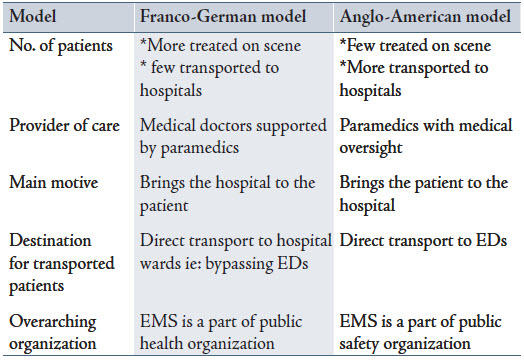
While both systems have the same principal mission when delivering emergency care for trauma and life-threatening illnesses. They differ when delivering non-life threatening care and scheduled transports of stable cases. The conventional European style uses primary care options other than transporting patients to Emergency Departments extensively more than the Anglo-American system. If to be transported, patients in Europe are usually escorted directly to a hospital floor where the attending field emergency physician believes condition will benefit more by direct admission unlike the American model where all admissions have to go through emergency department.5, 19-21
Many studies have attempted to compare the two systems in terms of outcome or cost-effectiveness. However, it seems that they are not really comparable because they tend to operate in different contexts with different types of demands to meet. Also, the lack of unified standards between the two models makes comparison an unjustifiable exercise. Thus, there is currently no evidence that one model is better than the other and studies continue to show conflicting conclusions.5,7,19, 22-24 Other than the issue of which model is best, there is the question of which organization in the community should provide EMS. Many have argued for a mixed model between health care organizations and public safety organizations but this approach has the potential for EMS not to be properly funded as it can be considered neither from a public safety system nor from a health care system.21 The bottom line is that, EMS should be provided by any community organization that is capable of delivering the best health care for the community regardless of its nature as a public safety or a public health.
In short, traditionally there are two models of EMS care delivery: Anglo-American which is based on “load and go” and Franco-German which is based on “delay and treat.” No model is better than the other and each community should decide on what suits them better according to their resources, targets and goals. However, patient outcomes should be the ultimate judging standard on which one is best.
Another way to classify emergency medical service systems is according to the level of service and scope of practice provided. These are usually classified as a Basic Life Support (BLS) level and Advanced Life Support (ALS) level.
Basic Life Support is tightly associated with the ‘load and go’ philosophy providing non-invasive basic interventions and rapid transport to definitive health care facility. Interventions are usually basic and include non-invasive cardiopulmonary resuscitation (CPR), fracture splinting, full immobilization and oxygen administration. On the other hand, the Advanced Life Support (ALS) fits more with the ‘stay and stabilize’ approach. It includes all the BLS procedures with the addition of invasive procedures such as endotracheal intubation, intravenous line placement, fluid replacement, needle-chest decompression and the administration of controlled and potent medications.25
The typical “all-Advanced Life Support” system operates as a one type fleet of ambulances managing urgent and non-urgent care of patients. All vehicles are staffed by ALS qualified personnel. This is in comparison to a tiered response system which utilizes both BLS and ALS crews, despatching ALS to the most severe of events only and BLS services are used for non-urgent and scheduled transports of stable patients. The tiered system has the advantage of freeing up ALS units for the acute care of seriously ill patients.25 Many studies have tried to advocate the efficacy of Advanced Life Support system over the Basic Life Support system. These studies suffer from multiple drawbacks such as small size populations and these studies are grossly confounded and biased.26 Furthermore, they tend to be descriptive studies rather than hypothesis testing studies. Some studies have gone further and claimed that ALS interventions in pre-hospital settings improves patient outcomes.27-30 This is only limited to trauma patients and is not yet established for medical emergencies. On the other hand, other studies have shown that a rapid transport of victims to a definitive health care facility rather than advanced interventions have major impact on patient outcomes.31-33 In short terms, it all comes down to the discretion of the attending provider to decide whether field interventions or rapid transport is the best measure on a case-by-case basis.
One might expect that it is advantageous to dispatch advanced level of care to all emergencies regardless of severity. This is a very ineffective approach to pre-hospital care as one study showed that only 85% of cases in the United States are within the scope of Basic Life Support care and require no advanced care.14 On the other hand, the disadvantage of the tiered system is the dilution effect which might lead to the loss of skills of personnel and less exposure to emergency events.25 The superiority of ALS over BLS has not been demonstrated and the World Health Organization warn about the trap of glamorous ALS skills appearing better than the simple BLS that a variety of people might benefit from.3 Thus, it is essential to determine the strengths and weaknesses of both levels of care and utilize the one that suits the local context most.
A new model of EMS delivery that has attracted attention recently is the Emergency Care Practitioner Scheme in the United Kingdom (UK). The UK, National Health Service has developed an Emergency Care Practitioner (ECP) scheme in a reaction to a change in primary health care provision in order to increase the percentage of patients treated in a community setting or at the scene of an incident.34 In the UK, 50% of patients transported by ambulance to emergency departments are discharged without any significant treatment or referral.35 Thus, the ECP scheme aims to reduce unnecessary ambulance transport to Emergency Departments.
The NHS defines an Emergency Care Practitioner as an allied healthcare professional who works to a medical model, with the attitude, skills, and knowledge base to deliver holistic care and treatment in the pre-hospital, primary care, and general practice environments, with a broadly defined level of autonomy.36 The scheme is designed to enhance and upgrade the skills of existing paramedics so that assessment and, where possible, treatment, can be provided in the community without transporting the patient to hospitals.
The scheme allows Emergency Care Practitioners to make autonomous clinical decisions within their scope of practice based on the concept of “chain of survival,”37 and allows paramedics to develop their careers outside the ambulance service in primary health care clinics and minor injury clinics.34The concept of the “chain of survival” has been developed from decades of research into out-of-hospital cardiac arrest. The survival from cardiac arrest is enhanced by performing a step wise sequence that has been shown to be effective in reducing mortality and improving survival. (Fig. 1)
This sequence includes: 1) early recognitions of signs, 2) prompt activation of emergency medical system, 3) prompt basic CPR, 4) defibrillation, 5) intubation, and 6) administration of medications. These chains have to be linked together and weakness in one chain will compromise the whole process. It is meant to act as a bridge between pre-hospital care and primary health care to achieve seamless, continuous and smooth transition of patient care. The scheme was first trialed in 2004 and continues to expand. The scheme’s effectiveness is yet to be fully evaluated but the preliminary results are encouraging.
Figure 1: Chain of Survival
One study showed that patient satisfaction is higher in clients receiving services by ECPs compared to traditional ambulance paramedics especially in two areas; “thoroughness of assessment” and “explaining what will happen next.”38 Many countries around the world such as Australia and New Zealand are contemplating about adopting this system into their existing pre-hospital care system especially in rural areas where the gap between primary health care and pre-hospital care is obvious and bridging the gap is a public demand.39, 40
Current international EMS systems have varied features and practices but they all resemble the main models of EMS systems in one way or another. The aim of international EMS systems is to adapt a model that meets the local needs and targets with diverse cultural, political and financial factors of each individual community. Advocating for a single system that fits all is a slippery approach to take in a rapidly changing world.
Oman has introduced the EMS system in 2004 under the auspices of the Royal Oman Police. It is based on the Anglo-American model and is designed to respond to trauma cases resulting from endemic Road Traffic Crashes (RTCs). Pre-hospital care is provided by all-Advanced Life Support trained Emergency Medical Technicians. The system is currently not tiered and has medical oversight from qualified doctors. Detailed description of the system is published elsewhere.18
As demographics of diseases in Oman change, so do the demands for emergency care. In recent years, there has been a dramatic increase in non-communicable diseases in the country such as diabetes mellitus and cardiovascular diseases.41 Hence, more medical emergencies are attended by Advanced Medical Emergency Technicians in Oman. Medical emergencies require a different approach than the classical trauma cases.18 Trauma outcomes are better managed by rapid transportation to definitive health care and less field interventions, while medical emergencies such as cardiac arrests benefit more from prompt field interventions and stabilization before transport. The EMS in Oman is growing rapidly and it has to adapt to the change in demands of emergency care in the Omani society. The concept of Emergency Practitioners in the community is attractive and worth contemplating in the Sultanate to reduce the burden of non-communicable disease on the Omani secondary and tertiary health care systems.
ACKNOWLEDGEMENTS
The author reported no conflict of interest and no funding was received on this work.
|