| |
Abstract
Objectives: To assess the knowledge of interns on standard precautions and post-exposure prophylaxis for HIV, and identify the gap between knowledge and practice relating to standard precautions, as well as determining the perceived barriers against adherence to standard precautions.
Methods: The study was conducted on 130 interns of 2010-11 batch from a government-run medical college in Kolkata, India. All participants completed a self-administered questionnaire with items relating to basic components of standard precautions and post-exposure prophylaxis for HIV. The questionnaire also included open ended questions relating to reasons for non-adherence to the practice of standard precautions along with additional space for specific comments, if any.
Results: Poor adherence in the use of personal protective equipment, hand washing, safe handling and disposal of needles and sharp objects were found to be among the practices for which the interns expressed correct knowledge. While the main reasons for non-adherence were found to be clumsiness in handling needles, wearing gloves, feeling uncomfortable when wearing aprons, impracticality of regular hand-washing and non-availability of equipment. Although the majority of the respondents (84.6%) expressed awareness of washing sites of injured with soap and water, approximately 32.3% did not know that antiseptics could cause more damage. Also, only 63.8% expressed awareness of reporting any incidence of occupational exposure, while knowledge on post-exposure prophylaxis regimens was generally found to be poor.
Conclusion: The considerable gap between knowledge and practice of standard precautions and inadequate knowledge of post-exposure prophylaxis emphasizes the need for continuous onsite training of interns with supportive supervision and monitoring of their activities.
Keywords: Standard Precautions; Adherence; Post-exposure prophylaxis; HIV.
Introduction
Standard Precautions (SP) include a group of infection prevention practices that apply to all patients, regardless of suspected or confirmed infection status, in any setting in which healthcare is delivered. These include hand hygiene, use of gloves, gown, mask, eye protection, or face shield, depending on the anticipated exposure; and safe injection practices.1
The types of exposure which may place healthcare personnel at risk of blood-borne infection may be a percutaneous injury (e.g., needle-stick or cut with a sharp instrument), contact with the mucous membranes of the eye or mouth, contact with non-intact skin (particularly when the exposed skin is chapped, abraded, or afflicted with dermatitis), or contact with intact skin when the duration of contact is prolonged (e.g., several minutes or more) with blood or other potentially infectious body fluids.2 In spite of the established "Standard Precautions", healthcare workers may experience accidental occupational exposure to HIV, and in order to minimize the risk of infection, clear guidelines for post-exposure-prophylaxis (PEP) are available.2
Interns at a very early stage of their professional career take maximum load of providing medical care in the in-patient and out-patient departments of any medical college across the world and more so in a developing country like India, and are thus at a great risk of occupational exposure to all kinds of blood borne pathogens including HIV. Earlier studies had shown poor knowledge and compliance of "Standard Precautions" among interns.3,4 It is thus essential to instill in them good infection control practices from the very beginning, before incorrect practice develops into a habit and to develop in them aware of PEP for prevention of HIV infection through occupational exposure.
The present study was thus conducted with the following objectives: 1) to assess the knowledge of the interns on standard precautions and post-exposure prophylaxis for HIV; 2) to identify the gap between knowledge and practice of standard precautions; and 3) to determine the perceived barriers against adherence to the standard precautions.
Methods
The study was conducted from September 2011 to November 2011 among all the 130 interns of the 2010-11 batch at Calcutta National Medical College and Hospital, Kolkata, West Bengal, India. Permission to conduct the study was obtained from the ethical committee of the medical college. A self-administered, pre-designed and semi-structured questionnaire was prepared by selecting relevant items from "Guidelines for HIV-infected adults and adolescents including post-exposure prophylaxis" published by National AIDS Control Organization, Government of India (2007),2 and modified according to the field experiences of the researchers. The questionnaire was then pre-tested among 10 post-graduate trainees from different clinical disciplines at the same hospital and further modifications were incorporated; however, reliability analysis was not performed. On the other hand, the assessment of knowledge of SP and PEP was done through a mixture of open and closed ended questions; questions assessing the practice of SP had the options such as "always practiced" and "not always practiced"; however, the Likert scale was not adopted, though it was considered that the self reporting nature of the responses may contradict the actual practice of SP. The questionnaire also included open ended questions regarding reasons for non-adherence to the practice of SP with an additional space for specific comments.
After obtaining informed consent from all the participants, they were asked to fill up this questionnaire within half an hour time. Since all the interns were not available at the same place and at the same time, the process was carried out at the in-patient wards of various departments at different time intervals. However, most of the interns by that time had worked in at least two major clinical disciplines.
The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 10 and were expressed in simple proportions. Adherence to the correct practice of different components of SP was assessed by analyzing the responses expressing the correct knowledge. The purpose was to determine whether or not correct knowledge had also been translated into correct practice. Since the number of correct responses relating to SP was different for its different components, the same statements were kept for presenting the data based on the practices involving those individual components for better understanding. Also, since the study participants, though belonging to different strata of the society but formed a homogeneous group who underwent the same kind of undergraduate training and working in the same environment during their internship, no statistical analysis was done on the basis of demographic variables.
Results
All the respondents expressed awareness of the blood contact route of transmission of HIV, Hepatitis B and C infections. The majority of correct knowledge was observed to be relating to the use of gloves and aprons, but knowledge relating to the use of goggles was found to be poor (54.6%). Moreover, most of participants conveyed knowledge of the following; importance of hand-washing, risk of bending or recapping used needles, and safe disposal of sharp instruments. (Table 1)
Table 1: Knowledge of the respondents regarding Standard Precautions. (n = 130)
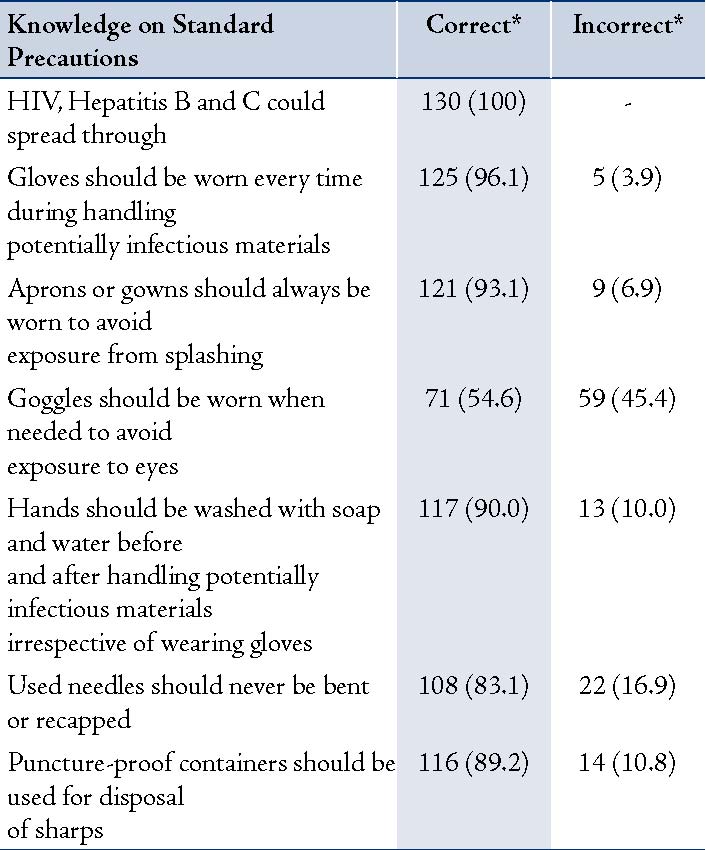
* Figures in parentheses indicate percentage
Among the components for which correct knowledge was expressed, practice of always using gloves, aprons/gowns and goggles was reported by only 62.4%, 56.2% and 22.5% of the respondents, respectively. The practice of hand-washing was poor (54.7%) among the participants who had correct knowledge of it; and only 66.3% of respondents who were aware of the policy to never bend or recap used needles adhered to its correct practice. Also, only 49.1% of the participants with the correct knowledge of safe disposal of sharp instruments reported to use puncture-proof containers for this purpose (Table 2). The main reasons for non-compliance to the correct practice of SP were as follows: a) inconvenience in handling needles and sharps when wearing gloves and often no time to wear gloves during rush hours; b) feeling uncomfortable to wear aprons in tropical climate; c) unavailability of goggles for regular use; d) regular hand-washing not feasible due to huge workload; e) non-availability of functioning hub-cutter and puncture-proof containers for safe handling and disposal of needles and sharps. (Table 2)
So far as the knowledge regarding immediate post-exposure prophylaxis to prevent transmission of HIV infection was concerned, 70.0% of the respondents were aware of the risk of putting fingers in the mouth to suck blood following a needle stick injury, and a majority (84.6%) of the respondents knew that the exposed area should be washed with soap and water. In addition, 67.7% knew that the application of antiseptics may cause more damage to the exposed tissues and 65.4% knew what to do following exposure to eyes and mouth. However, only 63.8% of the respondents were actually aware of the fact that any incidence of occupational exposure must be reported to the superior officer on-duty; and only 69.2% expressed the correct knowledge of basic PEP regimen and even fewer could correctly name the drugs included in the expanded regimen. It was also observed that 66.1% of the respondents knew exactly where PEP drugs were and with whom they can be obtained at the hospital. Furthermore, 68.5% were expressed awareness of the best time of initiation of PEP drugs, while only 46.9% conveyed the correct knowledge about the duration of the regimens. (Table 3)
Table 2: Practice of Standard Precautions among the respondents having correct knowledge and main reasons for non-adherence.
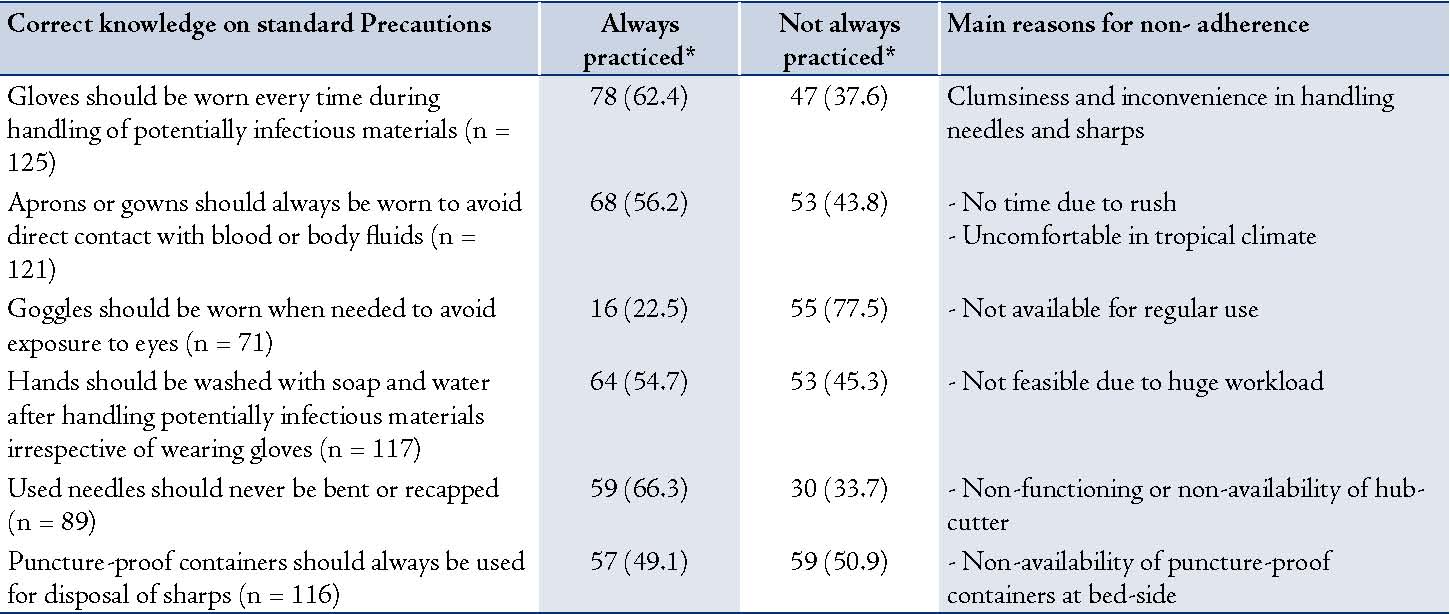
* Figures in parentheses indicate percentage
Table 3: Awareness among the respondents regarding post-exposure prophylaxis for HIV. (n = 130)
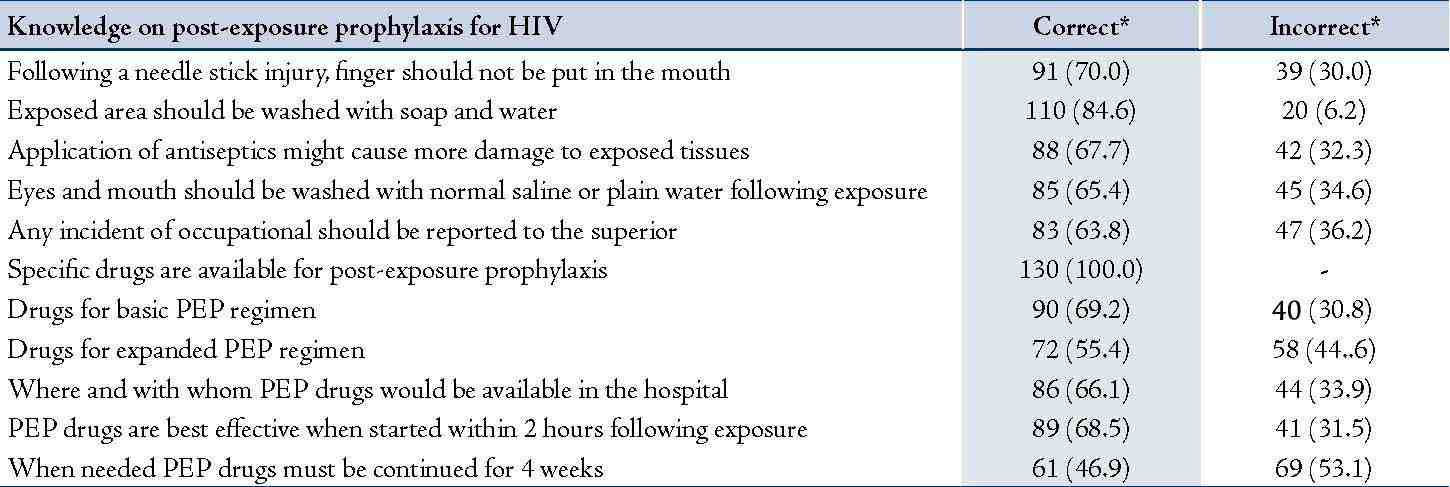
* Figures in parentheses indicate percentage
Discussion
The present study focused on investigating how far the correct knowledge of "Standard Precautions" is translated into correct practice in practical settings. The study subjects during their undergraduate course attended theoretical classes relating to important blood-borne infections, preventive actions and post-exposure prophylaxis and were also given practical demonstrations on different components of standard precautions and bio-medical waste disposal in a hospital setting. However, the results of this study revealed poor adherence to the main components of SP, like using personal protective equipment, hand washing, safe handling and disposal of needles and sharps, even among the interns who expressed correct knowledge of these policies. The main reasons for non-adherence to the correct practices of SP were reported to be; clumsiness in handling needles and sharps when wearing gloves and lack of time during rush hours, feeling uncomfortable to wearing aprons, the lack of availability of goggles for regular use, the infeasibility of regular hand-washing due to huge workload, and the lack of available functioning hub-cutter and puncture-proof containers.
Comments like "It is easy to do a venepuncture with bare hands rather than wearing gloves", "Aprons are quite unbearable in this tropical heat", "In such busy wards, hand washing on every instance is just not feasible", "There is no hub-cutter available at the bed side, so I bend the needle before disposing it off" and other more or less similar remarks further highlighted the main reasons for non-compliance. A study conducted in a tertiary care hospital in Delhi, India, showed that in spite of having adequate knowledge, adherence to practices of universal precautions remained poor among most interns except wearing gloves. While 90% of the respondents reported to follow correct disposal of needles and sharps, only 60% of the respondents never recapped or bent needles after use. The perceived impediments against the use personal protective equipment (PPE) were given as follows; too busy to use PPE, colleagues do not use them, and discomfort in PPE use.5 Time constraints, inconvenience, unavailability of equipment and presumption that the patient was not infected, were the reasons for non-compliance reported in another study from Chandigarh, India.6 Jawaid et al. in their study conducted in Karachi, Pakistan, found poor adherence to the regular use of PPE, and the reasons reported by the respondents were; unavailability of protective modalities and regular use of PPE being impractical and time consuming.7 Also, in a similar study conducted in Indonesia, Sari et al. reported poor adherence to SP in spite of high level of knowledge among the respondents.8 While a study from Saudi Arabia depicted poor knowledge on universal precautions and poor adherence to the guidelines.9
In the present study, while it was found that even though the majority of the respondents were aware of washing the site of injury with soap and water, around one-third of were unaware of the fact that the application of antiseptic could cause more damage to the already injured tissues. Many of the respondents also had no knowledge of the immediate measures undertake following exposure to eyes or mouth; and the lack of knowledge about reporting any incidence of occupational exposure was noted among many respondents, which was a great concern. In fact, a great number of them expressed no knowledge of where to look for PEP drugs in the hospital. In terms of knowledge of basic and expanded PEP regimens, the best time of initiation of the drugs and the duration of the regimens was found to be far lower than satisfactory.
In a similar study conducted in Mangalore, India, it was reported that only 23.5% knew the first aid measures following exposure and approximately 57.6% expressed knowledge relating to the application of antiseptics to the injured site; however, poor knowledge was observed with respect to the time of initiation of PEP, PEP drug regimens and their duration; while very few of the respondents actually knew where the drugs were available at the hospital and whom to first contact following any incidence of occupational exposure.10 While in a earlier study by Chogle et al. around 78% of the respondents correctly stated that washing the site of injury with soap and water was the initial measure, but less than a third knew whom to contact immediately after a needle stick injury; and although 64% expressed the correct knowledge on the time of initiation of PEP, none knew exactly which drugs to use. Furthermore, only 6% knew the correct duration of post-exposure prophylaxis.11 Another survey conducted by Siwach et al. in Chandigarh, revealed that 70% of the respondents were unaware of the availability of post-exposure prophylaxis, and most of them were unsure of the timings for its administration.12
In a hospital-based study in London, Chen et al. reported that although most junior doctors heard of PEP, only a minority could name the drugs recommended in national guidelines and a significant proportion could not name any.13 Another study from South Africa showed that around 67% of the respondents were not aware when PEP should be started, while nearly 76% did not know the drugs used for PEP and 81% did not know its correct duration.14
In the end, the researchers would emphasize the fact that the decision to start PEP following a needle prick depends a lot on the HIV status of the source, who often tends to hide their sero-status out of fear of stigma and discrimination, and might not show willingness to undergo HIV testing. Enwereji EE et al.15 identified stigma and discrimination as the main problems for HIV testing in their study. They also reported the limited use of universal prevention measures health workers adopted during health services., and they also found limited knowledge of benefits of people living with HIV/AIDS (PLWHA) disclosing their sero-status to healthcare professionals.15 They suggested that in order improve the healthcare seeking behavior of PLWHA, it is imperative for not only junior doctors, but all healthcare professionals to maintain a cordial relationship with the former.15
The present study has its own limitations, to begin with; the study assessed the self reported compliance of practice of "Standard Precautions", while the actual practice may be even lower. The results of this study could not be extrapolated to other groups of healthcare workers because they had not been included in the study. However, this study has to some extent been able to assess the training needs of the interns who are going to be the future consultants. Similar studies on different groups of healthcare workers are needed to determine whether knowledge and practice differ in different groups and the data from such studies will provide an opportunity to test the reliability of the questionnaire used in the present study.
Conclusion
Among medical interns who had just left the classroom, adequate knowledge of SP and PEP was supposed to be expressed with high level of compliance to the practice of SP. In sharp contrast to these expectations, the present study revealed a wide gap between knowledge and practice of "Standard Precautions" and inadequate knowledge of post-exposure prophylaxis for HIV. This indicates the need for continuous onsite training of interns and supportive supervision and monitoring of their activities related to biological waste handling. Moreover, adequate supply of equipment like hub-cutter and puncture proof containers is imperative to ensure adherence to the practice of proper disposal of needles and sharps instruments.
Acknowledgements
The authors are grateful to Dr. Salil Kumar Bhattacharya, Professor and Head, Dept of Community Medicine, Calcutta National Medical College, Kolkata, West Bengal, India, for his valuable input in manuscript preparation. The authors declare the research was self-funded and there are no competing interests in conducting this research or in the publication of this work.
References
1. Siegel JD, Rhinehart E, Jackson M, Chiarello L; The Healthcare Infection Control Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Setting. Available at: http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf. Accessed: Nov 10 2011.
2. Govt. of India 2007. Ministry of Health & Family Welfare. Antiretroviral therapy guidelines for HIV-infected adults and adolescents including post-exposure prophylaxis. National AIDS Control Organization. Available at: http://nacoonline.org/upload/Policies&Guidelines/1.Antiretroviral Therapy for HIV- Infected Adults and Adolescents for Post-exposure.pdf. Accessed: 10 Nov 2011.
3. Leon MP, Rivera A, Chinchilla A. Occupational accidents and knowledge about universal precautions in medical interns of Costa Rica. Antivir Ther 2003;8(Suppl. 1):S517-S8.
4. Hammond JS, Eckes JM, Gomez GA, Cunningham DN. HIV, trauma, and infection control: universal precautions are universally ignored. J Trauma 1990 May;30(5):555-558, discussion 558-561.
5. Kotwal A, Taneja DK. Health care workers and universal precautions: perceptions and determinants of non-compliance. Indian J Community Med 2010 Oct;35(4):526-528.
6. Dhaliwal B, Saha PK, Goel P, Huria A. Universal Precautions against HIV and other Blood-Borne Pathogens - Knowledge, Attitude and Compliance among health professionals in Obstetrics and Gynecology. NJOG 2011;6(1):13-16.
7. Jawaid M, Iqbal M, Shahbaz S. Compliance with standard precautions: A long way ahead. Iran J Public Health 2009;38(1):85-88.
8. Sari SYI, Ibrahim K, Haroen H, Afriandi1 I, Sunjaya1 DK, Hinduan ZR, et al. Knowledge, attitude and perceived adherence with universal precautions among health care workers in the obstetrics and gynaecology department of an Indonesian teaching hospital. Int J Infect Control 2011; v7: i4
9. Alam M. Knowledge, attitude and practices among health care workers on needle-stick injuries. Ann Saudi Med 2002 Sep-Nov;22(5-6):396-399.
10. Viswanathan S, Jain R, Adhikari MP, Jain A. Awareness of post – exposure prophylaxis guidelines against occupational exposure to HIV among post graduate residents at Mangalore, India. Int. J. Med. Public Health 2011;1(2):51-56.
11. Chogle NL, Chogle MN, Divatia JV, Dasgupta D. Awareness of post-exposure prophylaxis guidelines against occupational exposure to HIV in a Mumbai hospital. Natl Med J India 2002 Mar-Apr;15(2):69-72.
12. Siwach V, Dahiya D, Rao Ch UM, Dhanda R, Sharma A, Minz M. Resident doctors, bloodborne pathogens and universal precautions: are we sitting on a volcano? Natl Med J India 2001 May-Jun;14(3):179.
13. Chen MY, Fox EF, Rogers CA. Post-exposure prophylaxis for human immunodeficiency virus: knowledge and experience of junior doctors. Sex Transm Infect 2001 Dec;77(6):444-445.
14. Kermode M. Unsafe injections in low-income country health settings: need for injection safety promotion to prevent the spread of blood-borne viruses. Health Promot Int 2004 Mar;19(1):95-103.
15. Enwereji EE, Enwereji KO. Assessing factors that affect childbirth choices of people living positively with HIV/AIDS in Abia state of Nigeria. Oman Med J 2010 Apr;25(2):91-99.
|
|