|
Abstract
Objectives: Acute drug overdosing is an important cause of organ dysfunction and metabolic derangements and the patients often require intensive care. This study aims to determine the clinical pattern of severe drug overdose as well as the factors influencing the duration of intensive care.
Methods: The clinical characteristics and course of consecutive adult patients admitted with a diagnosis of acute drug poisoning in the ICU of a tertiary hospital in Oman from January 2007 to December 2008 were reviewed retrospectively from the electronic case records.
Results: Acute drug poisoning (n=29) constituted 3.9% of admissions to the ICU. Mean age was 29.38±7.9 years. They were brought in by their relatives (72%) or the state services (24%). Accidental poisoning was noted in 21 patients (72%) and suicidal overdosing in 6 (21%). The commonest drug was an opioid (65.5%). Glasgow Coma Scale score of ≤8 was recorded in 18 (62.1%). Sixty two percent of patients required mechanical ventilation. The prominent complications were hypotension in 9 (31%), pulmonary in 19 (65.5%), hepatic in 18 (62.1%) and renal in 12 (41.4%) patients. The major electrolytes abnormalities were low bicarbonate in 11 (37.9%), hyponatremia in 5 (17.2%) and hypokalemia in 4 (13.8%). Patients stayed in the ICU for 1 to 20 days (median-2 days). Factors associated with a longer ICU stay included hypotension upon arrival (p=0.048) and the need for mechanical ventilation on the first (p=0.001) and second (p=0.001) days of hospitalization. There was no mortality.
Conclusion: Early and prompt intensive medical therapy in acute drug poisoning can favorably influence the outcome. In addition, the presence of hypotension and requirement of mechanical ventilation on the first two days of hospitalization were responsible for prolonged ICU stay.
Keywords: Drug overdose, intensive care, opiates, Oman.
Introduction
Drug overdose continues to be the most common cause of acute poisoning all over the world.1 An estimated 2 to 5 million poisonings and drug overdoses occur annually in the United States of America. In Oman, an average annual rate of poisoning of 1.8/1000 Accident & Emergency Department (A&E) visits has been recorded for the study period from 1996 to 1999.2 Intentional or accidental drug overdose results in significant morbidity and mortality and tremendously adds to the health care expenditure. However, there is a lack of information on the impact of this important public health problem on the provision of intensive care.3, 4
The treatment and complications of drug poisoning in the ICU vary according to the nature of drug consumed, individual drug dose, the use of other drugs or alcohol and the patient population.5 In a study of 86 patients with acute drug poisoning, 23% required mechanical ventilation between 1-12 days with fatal outcome in 5.8% cases.6 In another report of 50 patients, 34% required mechanical ventilation and 4% required dialysis.7 Aspiration pneumonitis, cardiac and neurological impairment are the other potential complications of drug overdose.4, 8, 9
From a therapeutic perspective, the identification of a drug-related illness is important not only to improve the provision of appropriate acute medical care but also to allow early and prompt psychiatric referral to prevent recurrence.10 The aim of this study is to describe the clinical and epidemiological features, the course, complications and the care received in the ICU for adult patients with severe acute poisoning and illicit drug use in a tertiary care hospital in Oman.
Methods
Data of the consecutive adult patients who were admitted to the ICU in Sultan Qaboos University Hospital, Oman over a two year period from January 2007 to December 2008 for management of non-alcohol drug-related poisoning were retrospectively analyzed. The study was approved by the ethics committee of the Sultan Qaboos University. The cases admitted to the ICU with a diagnosis of drug overdose were retrieved from the electronic patient database of the hospital. Cases were identified if the admitting diagnosis was a confirmed drug overdose within the 12 hours prior to admission, or if blood or urine testing demonstrated the presence of non-prescribed drugs or inappropriately high levels of prescribed medications. Cases where the discharge diagnosis was suspected drug overdose after exclusion of other possible differentials were also identified, reviewed and were included. Cases were excluded if the admission was solely related to alcohol ingestion. The following information from the identified cases was extracted from the electronic patient records (EPR) and reviewed by two independent observers. Patient’s demographic data collected were age, sex, occupation, address and the details about any underlying medical problems including psychiatric illness. Clinical parameters included blood pressure, heart rate, Glasgow Coma Scale (GCS) score, presence of respiratory, neurological or gastrointestinal symptoms (if recorded) and the details about the immediate management in the emergency room. Initial basic laboratory investigations results, the drug levels (if available) and the ECG abnormalities (if present) were also noted. The lengths of hospital stay, intensive care interventions, metabolic and organ-specific complications, requirement of respiratory or cardiovascular support, dialysis and psychiatry consultation were then documented.
The data were tabulated and analyzed using the statistical package for social sciences program (SPSS, PC Version 16.0). Chi Square test or Fischer’s exact test was used to identify the factors influencing ICU stay.
Results
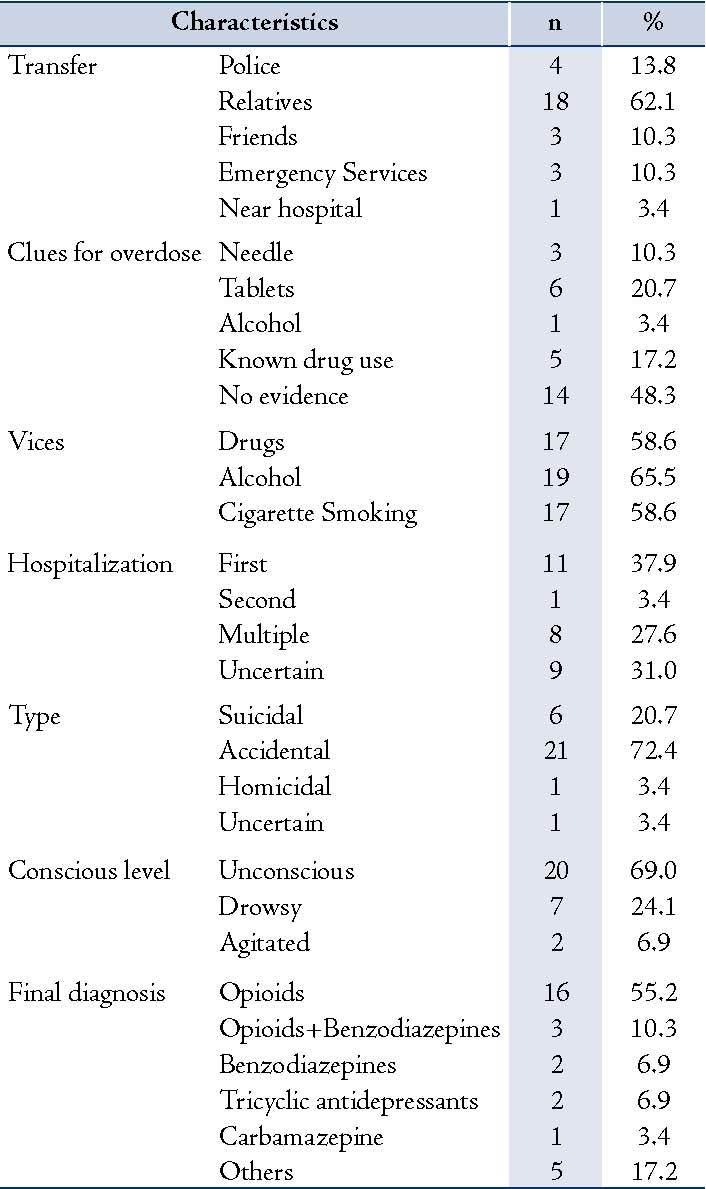
Twenty nine patients with drug overdose were admitted to the ICU during the study period, accounting for 3.86% of overall admissions in the same period. Table 1 shows the demographic and clinical details of the subjects. Majority of our patients were males (89.7%) and the mean age of the patients was 29.38±7.9 years. There was no significant difference in age between males and females in our cohort of patients.
Most of the patients were brought in by relatives or friends (72.4%) while the rest, 7 (24.1%) patients were transported by the state services. There was some evidence suggesting drug abuse as a possible cause of the clinical problem in 51.7% of patients (Table 1). Later, history of drug abuse was obtained in 17 (58.6%), alcohol abuse in 19 (65.5%) and smoking in 17 (58.6%) patients. The initial suspicion of the drug abuse was proved correct in almost all cases with opioid being the commonest drug (65.5%) (Table 1). Three patients took both opioids and benzodiazepines together. Among the five patients grouped under other drug category, one consumed a cocktail of nonsteroidal anti-inflammatory drugs, one took an antipsychotic drug (risperidone) and in three cases, no drugs were clearly identified.
At presentation, all except two patients were found to be either unconscious or drowsy. GCS was ≤8 in 18 (62.1%). Eighteen subjects (62.1%) were intubated, while one patient received non invasive ventilation (NIV). The reasons for intubation were altered conscious level in 15 (51.7%), evidence of fatigue in 2 (6.9%) and respiratory arrest in 1 (3.4%). In the A&E, naloxone, flumazenil, thiamine and antibiotics were administered in 19 (65.5%), 3 (10.3%), 5 (17.2%) and 19 (65.5%) patients respectively.
In 11 subjects (37.9%), the present hospitalization was the first admission for drug overdose, while 8 (27.6%) were admitted more than twice. During hospitalization, although the mean systolic BP was 116.3±22.4, nine (31.0%) had hypotension and needed ionotropic support. Of the 18 patients intubated in the A&E, 5 patients were extubated on the same day and only 10 (34.5%) were still on a ventilator by the second day. This was achieved with the use of NIV in those 5 patients. NIV was continued in only 2 patients on the following day. Respiratory complications were noted in 19 (65.5%), hepatic in 18 (62.1%), cardiac in 15 (51.7%), and renal in 12 (41.4%). Coagulation abnormalities were noted in 4 (13.8%). Chest radiographs showed unilateral infiltrates in 7 (24.1%) and bilateral infiltrates in 12 (41.4%). These were considered as aspiration pneumonia in 12 (41.4%) and as ARDS in 3 (10.4%). The major electrolytes abnormalities on admission were low bicarbonate in 11 (37.9%), hyponatremia in 5 (17.2%) and hypokalemia in 4 (13.8%).
Table 1: Characteristics of patients admitted to the ICU with suspected drug overdose and the final diagnosis (n=29).
Patients stayed in the ICU for 1 to 20 days (median: 2 days) and in the general medical ward for another 1 to 28 days (median: 3 days). Reasons for a longer stay in ICU (longer than the median period of 2 days) were analyzed (Table 2). Hypotension on arrival (p=0.048) and the requirement of mechanical ventilation on either day one (p=0.001) or day two (p=0.001) were the factors associated with longer ICU stay (Table 2). The drugs involved, GCS on admission or the presence of pulmonary infiltrates did not influence the duration of stay. But those two patients who remained in the ICU for more than a week (8 and 21 days respectively) had developed ARDS. Fortunately, there were no deaths and most of them were discharged in a stable state. In-patient psychiatric consultation was obtained in 22 (75.9%) patients.
Table 2: Factors influencing the duration of stay beyond the median period of 2 days in patients admitted to the ICU with suspected drug overdose (n=29).
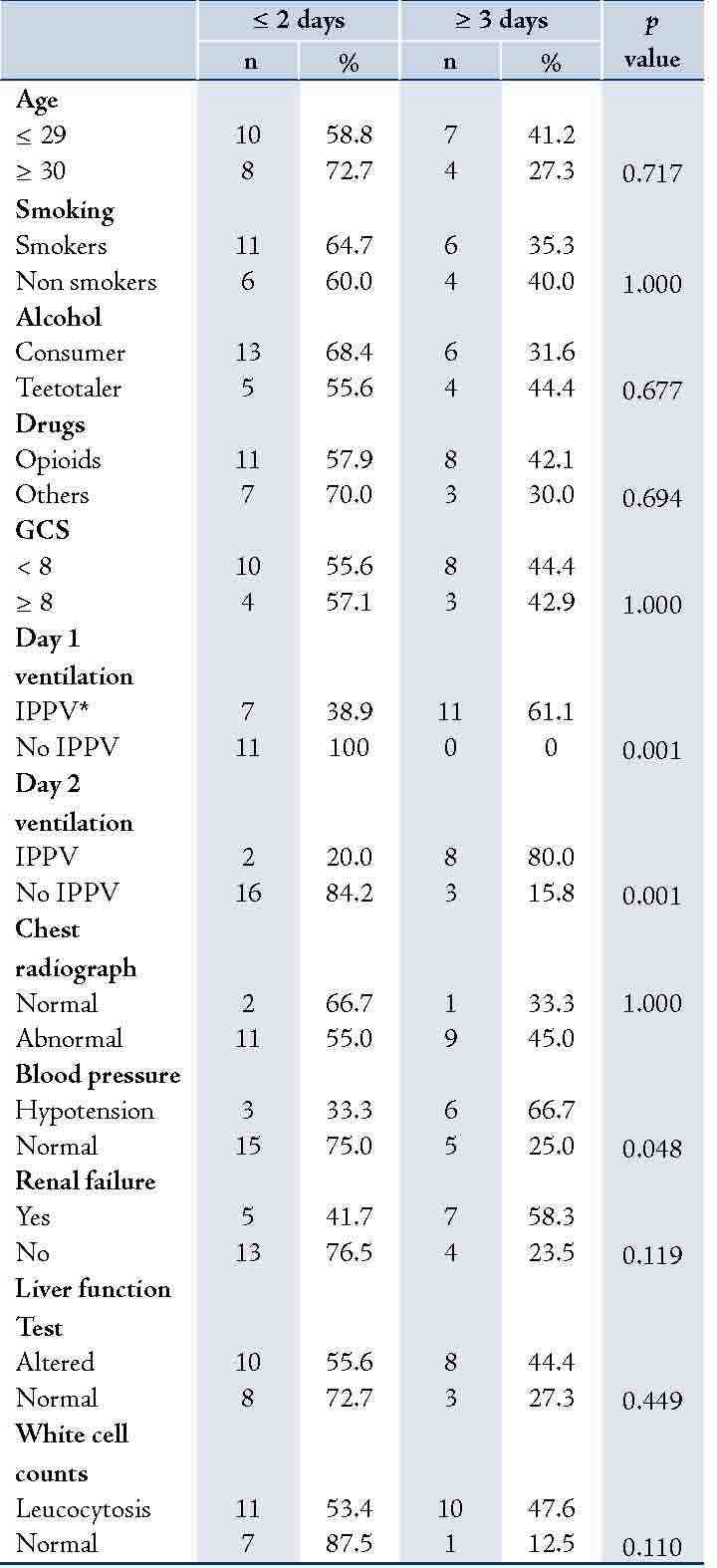
*Intermittent Positive Pressure Ventilation
Discussion
Opioids were the main drugs abused by the patients who needed ICU care. Accidental overdose of these drugs in those who had been already abusing them was the commonest mode of poisoning. Prompt care in ICU resulted in a shorter stay and virtually no mortality. We observed that the need for mechanical ventilation on the first two days and the presence of hypotension led to a longer time for recovery.
The pattern and nature of drug overdose vary geographically. In an earlier report from Oman, a significantly high frequency of poisoning by animal and traditional remedies with less frequent abuse of psychoactive drugs were observed in adults.2 These two studies cannot be compared as the present study focused only on those patients admitted to the ICU. However, the pattern of drug abuse seems to be changing in Oman and closely matches the scenario in the developed countries such as Australia, where the common drugs abused in the order of frequency were benzodiazepines, followed by opioids and tricyclic antidepressants.11 The Drug Abuse Warning Network in the USA estimates 162,137 heroin-related emergency department visits and 37,007 unspecified opiate-related emergency department visits in 2004.12 From a trans-cultural perspective, the pattern in another Gulf country, Saudi Arabia reveals a striking difference. The most common agents were the prescribed medications.13 Interestingly in the Southeast Anatolian region of Turkey, intentional self-poisonings with pesticide was common, especially among young, unmarried females.14
The primary concerns with overdose are a bit different with each class of drugs. Illicit opioid use, especially parenteral, contributes to premature mortality and disability in young adults in both developed and developing countries. Fatal overdoses and HIV/AIDS resulting from the sharing of needles are the major concerns.15 Benzodiazepines cause central nervous system depression but complications and the lethal outcome are rare.16 Impaired consciousness, acidosis, seizures, and cardio toxicity are associated with severe toxicity with antidepressants, particularly the tricyclic antidepressants.16, 17 The incidence of self poisoning by anti epileptic drugs has increased in the recent years in USA and these patients often need more critical care management and psychiatric intervention.18, 19
Most of our patients were young adults aged less than 40 years. More than 70% of the patients were brought to the hospital by their family members. Regarding the mode of poisoning, intentional drug overdose is reported to be a relatively uncommon reason for hospital admission in Saudi Arabia.13 A similar trend, accidental overdose, was seen in our patients as well. But a study from a less affluent Asian nation, Nepal, found that almost all poisoning were due to suicidal attempts.20 This suggests that cultural and socio-economic factors might play a role in the mode of poisoning. Nearly 21% of our patients provided a history of drug abuse or use of alcohol. The prevalence of concurrent and simultaneous use of alcohol and drugs varies by the type of drug used and drinking patterns and most abusers consume alcohol mostly for boosting, balancing, counteracting, or sustaining the effects of the other drug.21, 22
The majority of our patients were brought in a state of drowsiness or other levels of altered consciousness. Cretikos and Parr reported that 18% of their patients required mechanical ventilation, 18% inotropic support and 6% dialysis.11 On the contrary, 62.1% of our patients needed intubation and 31% needed ionotropes. Many factors like late presentation, larger doses leading to severe respiratory depression, opiates and the high standard of care may have influenced this. A lesser frequency (23% and 34%, respectively) of requirement of mechanical ventilation was also observed in other studies.6, 7 Fortunately, most of our patients had a short ICU and hospital stay. Factors associated with a longer stay (longer than the median of 2 days) were requirement of mechanical ventilation on days 1 and 2 and hemodynamic compromise on arrival. The drugs involved, GCS on admission or the presence of pulmonary infiltrates did not influence this outcome.
Chest radiographs were abnormal in a significant number of our patients. The cause of the infiltrate was mostly attributed to and managed as aspiration pneumonia in this setting. Christ et al. reported that clinically relevant aspiration pneumonia was a frequent complication in an unselected cohort of consecutive overdose patients admitted to the ICU.23 Moreover, they found that aspiration was associated with an increased length of stay in the ICU and a higher incidence of cardiac arrest. Unlike this report, the presence of either unilateral or bilateral chest radiographic infiltrates did not influence the length of ICU stay in our patients. At the same time, those two patients who remained in the ICU for more than a week had ARDS and multi organ dysfunction including renal failure. The remarkable recovery and survival in these patients suggested that application of suitable treatment protocols in an intensive care setting could favorably influence the clinical outcome even in the setting of multi organ dysfunction.
With a retrospective study design, we had difficulty in obtaining full clinical details in some of the patients, especially in the absence of standard documentation and charting of information. Other limitations are probably a small sample size and a lack of laboratory confirmation of opioid over dosage. Furthermore, the pattern and the agents of poisoning may vary from region to region and with time in the same region, so the findings of this study could not be readily generalized to other neighboring countries. It is likely that the patients with complications other than cardio-respiratory impairment, although a small number, would have influenced the data analysis.
Conclusion
In acute drug poisoning, a high index of clinical suspicion and an early and prompt intensive medical therapy could improve the patient outcome. Abuse of more than one agent, especially opioids along with alcohol, by our patients implies the easy accessibility of poly-substances in the vicinity and the user’s intention of achieving high levels of intoxication. This pattern of illicit poisoning warrants the development of suitable preventive measures. In particular, there is an imminent need to create awareness in the society to identify the circumstances leading to illicit drug use among the youth.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Litovitz TL, Klein-Schwartz W, Rodgers GC Jr, Cobaugh DJ, Youniss J, Omslaer JC, et al. 2001 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med 2002 September;20(5):391-452.
2. Hanssens Y, Deleu D, Taqi A. Etiologic and demographic characteristics of poisoning: a prospective hospital-based study in Oman. J Toxicol Clin Toxicol 2001;39(4):371-380.
3. Henderson A, Wright M, Pond SM. Experience with 732 acute overdose patients admitted to an intensive care unit over six years. Med J Aust 1993 January 4;158(1):28-30.
4. Wilson KC, Saukkonen JJ. Acute respiratory failure from abused substances. J Intensive Care Med 2004 July;19(4):183-193.
5. Buxton JA, Skutezky T, Tu AW, Waheed B, Wallace A, Mak S. The context of illicit drug overdose deaths in British Columbia, 2006. Harm Reduct J 2009;6:9.
6. Cengiz M, Baysal Z, Ganidagli S, Altindag A. Characteristics of poisoning cases in adult intensive care unit in Sanliurfa, Turkey. Saudi Med J 2006 April;27(4):497-502.
7. Tay SY, Tai DY, Seow E, Wang YT. Patients admitted to an intensive care unit for poisoning. Ann Acad Med Singapore 1998 May;27(3):347-352.
8. Isbister GK, Downes F, Sibbritt D, Dawson AH, Whyte IM. Aspiration pneumonitis in an overdose population: frequency, predictors, and outcomes. Crit Care Med 2004 January;32(1):88-93.
9. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 2001 March 1;344(9):665-671.
10. Jenkins DH. Substance abuse and withdrawal in the intensive care unit. Contemporary issues. Surg Clin North Am 2000 June;80(3):1033-1053.
11. Cretikos MA, Parr MJ. Drug related admissions to intensive care: the role of illicit drugs and self poisoning. Crit Care Resusc 2003 December;5(4):253-257.
12. Substance abuse and mental health services administration, Office of the applied studies. Rockville,MD; 2006. Report No.: DAWN Series,D-28, DHHS Publication No.(SMA) 06-4143.
13. Al-Jahdali H, Al-Johani A, Al-Hakawi A, Arabi Y, Ahmed QA, Altowirky J, et al. Pattern and risk factors for intentional drug overdose in Saudi Arabia. Can J Psychiatry 2004 May;49(5):331-334.
14. Guloglu C, Kara IH. Acute poisoning cases admitted to a university hospital emergency department in Diyarbakir, Turkey. Hum Exp Toxicol 2005 February;24(2):49-54.
15. Hall W, Doran C, Degenhardt L, Shepard D. Illicit Opiate Abuse. In: Jamison DT, Breman JG, Measharm AR, Alleyne G, Claeson M, Evans DB et al., editors. Disease Control Priorities in Developing Countries. 2nd edition. 2nd edition ed. Washington (DC): World Bank; 2006. p. 907-931.
16. Bosch TM, van der Werf TS, Uges DR, Ligtenberg JJ, Fijen JW, Tulleken JE, et al. Antidepressants self-poisoning and ICU admissions in a university hospital in The Netherlands. Pharm World Sci 2000 June;22(3):92-95.
17. Caravati EM, Bossart PJ. Demographic and electrocardiographic factors associated with severe tricyclic antidepressant toxicity. J Toxicol Clin Toxicol 1991;29(1):31-43.
18. Bronstein AC, Spyker DA, Cantilena LR, Jr., Green J, Rumack BH, Heard SE. 2006 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS). Clin Toxicol (Phila) 2007 December;45(8):815-917.
19. Nixon AC, Doak MW, Crozier H, Crooks DP, Waring WS. Patterns of antiepileptic drug overdose differ between men and women: admissions to the Edinburgh Poisons Unit, 2000-2007. QJM 2009 January;102(1):51-56.
20. Singh DP, Aacharya RP. Pattern of poisoning cases in Bir hospital. Journal of Institute of Medicine 2006;28(1):3-6.
21. Carroll JF, Malloy FE, Kenrick FM. Alcohol by drug-dependent persons: a literature review and evaluation. Am J Drug Alcohol Abuse 1977;4(3):293-315.
22. Midanik LT, Tam TW, Weisner C. Concurrent and simultaneous drug and alcohol use: results of the 2000 National Alcohol Survey. Drug Alcohol Depend 2007 September 6;90(1):72-80.
23. Christ A, Arranto CA, Schindler C, Klima T, Hunziker PR, Siegemund M, et al. Incidence, risk factors, and outcome of aspiration pneumonitis in ICU overdose patients. Intensive Care Med 2006 September;32(9):1423-1427.
|