|
Abstract
Objectives: This study aims to explore the risk factors, profiles and neonatal outcomes of Cesarean sections among selected women in Oman.
Methods: In this hospital-based case-control study, a total of 500 participants (250 cases who had cesarean section and 250 controls who had spontaneous vaginal delivery), were randomly selected from four hospitals. Cases and controls were matched according to timing and place of delivery.
Results: The following predictors were found to be significantly associated with increased risk of cesarean section: a) advancing age (above the age of 25 years, OR=1.42; p=0.03), b) prior cesarean section (previous cesarean section=1, OR=22.71; p=0.001), c) increased body mass index (obesity, OR=2.11; p=0.07), d) extremes of neonatal birth weight (neonates birth weight <2.5 kg, OR=5.2; neonates birth weight >4.0 kg, OR=7.3; p<0.001), and e) prepregnancy diabetes (OR=9.3; p=0.04). On the contrary, increased parity and history of the use of birth spacing methods (OR=0.38; p=0.03) were associated with decreased risk of cesarean section.
Conclusion: The study calls for increasing awareness about clinical and public health majors that would lead to prevention of risk factors associated with increased risk of cesarean section such as maintaining normal BMI and prevention of gestational and type 2 diabetes mellitus.
Keywords: Obstetrics; Non-obstetrics; Cesarean.
Introduction
The number of women having babies born by cesarean section is rapidly growing in both the developed and developing countries.1 The World Health Organization states that 15% should be the maximum and that no region in the world is justified with having a cesarean rate greater than 10% to 15%.2 However, in 2004, the cesarean rate was about 20% in the United Kingdom as opposed to 23.7% in Canada between 2002 and 2003.3 In 2004, approximately 1.2 million women in the United States had a cesarean birth representing 29.1% of all births.4
Among the developing countries, Brazil has one of the highest rates of cesarean sections in the world, which reached a high peak of 36.4% in 1996.5 Population- and hospital-based cesarean section rates for the 18 Arab countries are as follows: Yemen, Mauritania, Sudan, and Algeria have population cesarean section rates below 5%; while Palestine, Oman, Morocco, Libya, Tunisia, Saudi Arabia, UAE, Egypt, Jordan, Kuwait, and Syria have cesarean rates ranging between 5% to 15%; and the three countries with rates above 15% are Lebanon, Qatar and Bahrain.1
The cesarean section rate in Oman has gradually increased over ten years from 9.7% in 2000 to 15.72% in 2009, according to the annual report of the Ministry of Health in Oman.6,7 The study objectives were to describe the epidemiology of cesarean section and to ascertain the main obstetric and non-obstetric risk factors of cesarean sections in Oman, as well as to measure the degree and extent of association between cesarean sections and the leading risk factors. This study also aims to determine the neonatal outcomes of cesarean section.
Methods
This case-control study was conducted during the period from January to March 2009. The study participants were randomly selected from the Obstetrics and Gynecology Departments of four hospitals, namely; Sultan Qaboos University Hospital, Royal Hospital, Khoula Hospital and Nizwa Regional Hospital. After determining the total sample size of 500 women, 250 women who had cesarean section in singleton pregnancies (cases) and 250 women with singleton spontaneous vaginal deliveries (control) for various indications were selected. In each Obstetrics and Gynecology Department of the four hospitals mentioned above, there was a box which contained all files of women who delivered through cesarean section and who delivered vaginally during the day of data collection. The cases and the controls were randomly selected from these boxes. The data was collected by obtaining information from the Maternal Health Card and through personal interview of the selected women. The data included personal information such as age, parity, height, weight, occupation, income and exposure to risk factors like diabetes mellitus, hypertension, anemia, fetal presentation, number of previous cesarean sections, birth spacing, spontaneous or induced labor, infertility treatment, and maternal exercises during pregnancy. The study was approved by the Medical Research and Ethics Committee at the College of Medicine and Health Sciences. In addition, a pre-visiting permission was obtained from each hospital to collect information from the Maternity Green Card and interview of the mothers. An informed consent was obtained from each participant.
Results
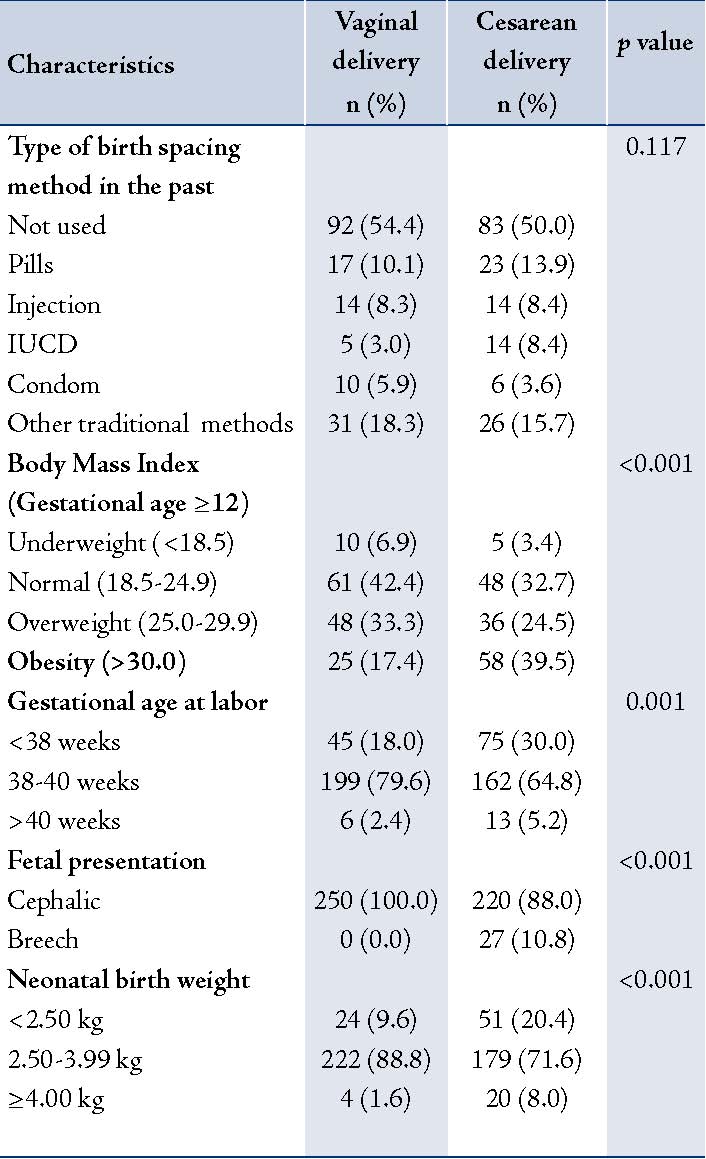
The results of univariate analysis of the study showed that among the demographic risk factors, advancing age and increasing family income were positively associated with the experience of delivery by cesarean section. Among the medical conditions that were observed to cause complications during pregnancy were pre-pregnancy, gestational diabetes and having one or more previous cesarean sections. These were positively associated with delivery by cesarean section. Among contraceptive methods used by women, only past use of IUCD method was positively associated with the indication of cesarean section. While among obstetric factors, obesity, gestational age of <38 weeks, breech presentation, and extremes of neonatal birth weight (<2.50 kg and ≥4.00 kg) were positively associated with cesarean section delivery. (Tables 1 and 2)
Table 1: Association between cesarean delivery and various sample characteristics based on univariate analysis.
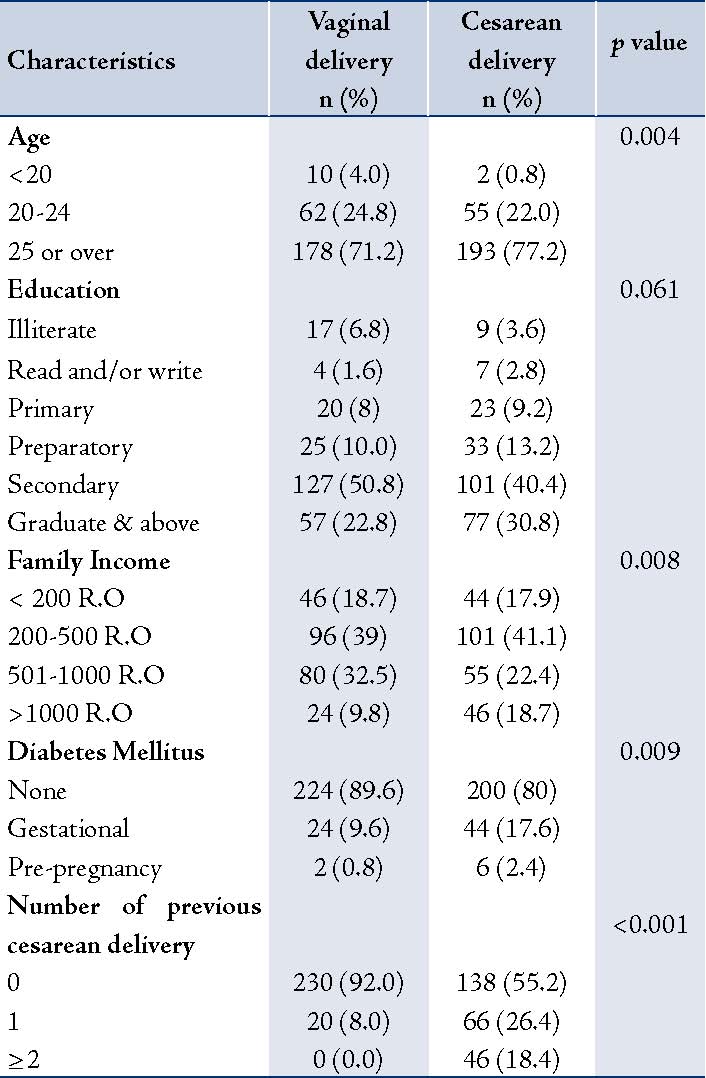
Table 2: Association between cesarean delivery and various sample characteristics based on univariate analysis.
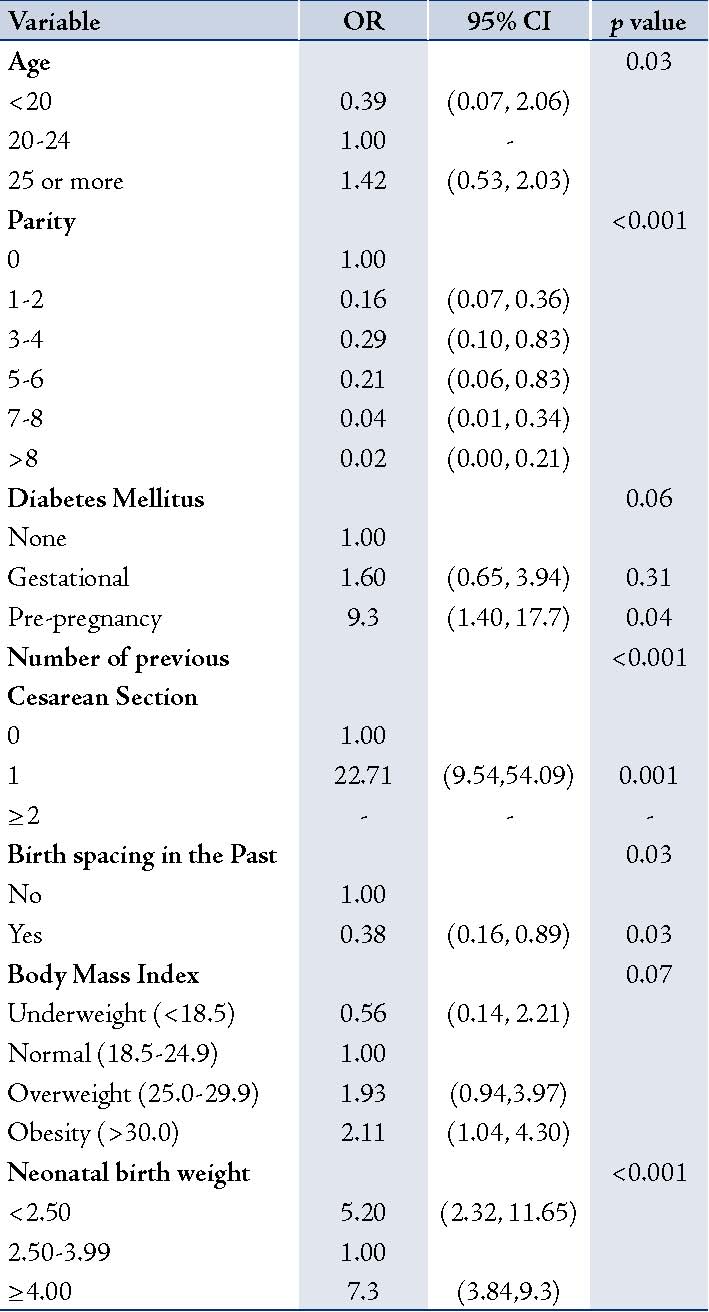
After multivariate logistic regression (backward step-wise) for all risk factors in the study, advance age (above 25 years of age, OR=1.42; p=0.03), pre-pregnancy diabetes (OR=9.3; p=0.04), having one or more previous cesarean section delivery (previous cesarean section=1, OR=22.71; p=0.001), increased body mass index (obesity OR=2.11; p=0.07) and extremes of neonates birth weight (neonates birth weight <2.5 kg, OR=5.2; or neonates birth weight >4.0 kg, OR=7.3; p<0.001) were important indicators of cesarean deliveries. Moreover, it was observed that increased parity and history of use of birth spacing methods (OR=0.38; p=0.03) were associated with decreased risk of cesarean section deliveries. (Table 3)
Table 3: Association between cesarean delivery and various sample characteristics based on multivariate analysis.
Discussion
Based on this study, the observation that advanced maternal age is associated with cesarean deliveries is in line with the findings of many other studies.5,8-14 The reason behind this association may be that older women are more likely to experience pregnancy complications such as diabetes, hypertension and pre-eclampsia.15
Decreased uterine contractility or a decreased number of oxytocin receptors in older women may result in less effective labor contractions according to Roberts et al.16 Obesity and breech presentation in older maternal age are other risk factors implicated in cesarean deliveries at advanced maternal age.17-19
A study conducted in China showed that the adjusted odds ratio for cesarean delivery was 4.46 times higher in women with university/college education compared to women who were illiterate or primary school educated (OR=4.46; 95% CI 2.89, 6.88).10 After adjustment for age and parity in the current study, the strength of association between cesarean deliveries and education decreased. Although it was observed that women having high family income were at an increased risk of experiencing cesarean deliveries compared to those with low family income, a finding similar to that reported in Brazilian study,5 the risk decreased when adjusted for confounding factors such as age and education.
Women with gestational and pre-pregnancy diabetes were more likely to experience cesarean deliveries compared to women free of diseases. This is consistent with the findings of a study conducted in England and the USA,8,19 which is likely due to macrosomia.20,21
A highly significant association was found between cesarean deliveries and the number of previous cesarean sections in this study. This finding is consistent with the findings of a study conducted in six countries (Bangladesh, Colombia, Dominican Republic, Egypt, Morocco and Vietnam) which all showed that previous cesarean section deliveries was the highest risk factor for subsequent cesarean in all countries.13 Women with previous cesarean section/s were at risk of uterine rupture and bleeding due to placenta previa during pregnancy.22 While women with more than one previous scar are rarely given a trial for vaginal delivery; hence, they almost always have a planned cesarean delivery. There was a significant association between cesarean deliveries and abnormal fetal presentations like breech or transverse lie, as it is obstetrically indicated.8,23,24
The association between cesarean section and obesity has previously been reported in the literature.19,25-27 Obesity is associated with pregnancy complications which include pre-eclampsia, diabetes and gestational hypertension.9,28,29 In addition, obesity is also associated with induced labor and delivery of a macrocosmic infant.25-27
Women who were preterm (<37 weeks gestation) and post term (>40 weeks) were more likely to experience cesarean delivery compared to women at 38-40 weeks gestation. Similar results were reported in a study conducted in England which showed that increasing gestational age was independently associated with a decreased risk of cesarean sections.8 Another study conducted in the USA found that the increase in cesarean sections in singleton preterm births was probably due to more breech presentations.30
A fetus weighing less than 2.5 kg or more than 4 kg would most likely need to be delivered via cesarean section compared to fetus weith normal neonatal birth weight. Patel et al. reported similar observations and similar results were found by another study indicating both large and small fetuses are mostly implicated in cesarean deliveries than infants with the average neonatal birth weight.31
Conclusion
Based on the above observations, the following are the suggested recommendations: First, the women aged >40 years should be counseled during antenatal care that they are at high risk of cesarean delivery. Second, women with gestational diabetes should follow strict dietary advice apart from exercise and medications during pregnancy to control macrosomia hence, the possibility of cesarean section. Moreover, women must be encouraged to deliver normally especially in their first pregnancy to avoid repeated cesarean sections. The study outcome encourages women to do regular exercise so as to maintain their weight as appropriately as possible and avoid obesity that can cause adverse effects on their health. The observed association of IUCD and cesarean section needs to be investigated in a larger study as this association may have happened by chance in the present study. The findings of this study highlight the importance of health education towards Omani women throughout the antenatal period. The messages of health promotion can be best addressed through specialized antenatal counseling clinics. Such specialized counseling clinics are not yet available in Oman and these services are being provided among the routine work at the antenatal care clinics.
Acknowledgements
The auuthors reported no conflict of interest and no funding was received in this work.
Reference
1. Rozzet J, Marwan K. Caesarean section rates in the Arab region: a cross-national study. Health Policy Plan. 2004;19(2):101-110.
2. Leone T, Padmadaas SS, Mathews Z. Community factors affecting rising caesarean section rates in developing countries: An analysis of six countries. Social Science & Medicine. 2008;67(8):1236-1246.
3. Leeb K, Baibergenova A, Wen E, Webster G, and Zelmer J. Are There Socio-Economic Differences in Caesarean Section Rates in Canada. Healthcare Policy/Politiques de Santé. 2005;1(1):48-54.
4. Fay Menacker, Eugene Declercq, Marian F. Macdorman. Cesarean Delivery: Background, Trends, and Epidemiology. Seminars in Perinatology. 2006;30(5):235-241.
5. Uiho A Gomes, Antonion AM silva, Heloisa Bettiol and Marco ABarbieri. Risk factors for increasing cesarean section rate in southeast Brazil: a comparison of two cohorts, 1978-1979 and 1994. International Journal of Epidemiology 1999;28:687-694.
6. Annual Health Report 2000, Directorate General of Planning. Ministry of Health. Sultanate of Oman: 2001. p.7-51
7. Annual Health Report 2009, Directorate General of Planning. Ministry of Health. Sultanate of Oman: 2010. p.7-35
8. Rosi R Patel, Time J Peters, Deirdre J Murphy. Prenatal risk factors for Caesarean section. Analyses of the ALSPAC cohort of 12 944 women in England. International Journal of Epidemiology. 2005;34(2):353-367.
9. Anne W. Read, Walter J. Prendiville, FRACOG, Vivienne P. Dawes, MBChB and Fiona J. Stanley. Cesarean Section and Operative Vaginal Delivery in Low-Risk Primiparous Women, Western Australia. Am J Public Health; 1994 January;84(1):37-42.
10. Shenglan Tang, Xiaoyan Li, Zhuochun Wu. Rising cesarean delivery rate in primiparous women in urban China: Evidence from three nationwide household health surveys. Am J Obstet Gynecol; 2006 March;195:1527-1532.
11. Kuang-Hung Hsua, Pei-Ju Liaob C, Chorng-Jer Hwanga. Factors affecting Taiwanese women’s choice of cesarean section. Social Science & Medicine; 2008;66:201-209.
12. Sabu S. Padmadasa, Suresh Kumar S.b, Sajini B. Nairc, Anitha Kumari K.R.b. Caesarean section delivery in Kerala, India: Evidence from a National Family Health Survey. Social Science & Medicine; 2000;51:511-521.
13. Tiziana Leone A, Sabu S, Padmadas B, Zoe Matthews B. Community factors affecting rising caesarean section rates in developing countries: An analysis of six countries. Social Science & Medicine; 2008;67:1236-1246.
14. Ilana F. Gareen, Hal Morgenstern, Sander Greenland, Deidre Spelliscy Gifford. Explaining the association of maternal age with Cesarean delivery for nulliparous and parous women. Journal of Clinical Epidemiology; 2003;56:1100-1110.
15. Samueloff A, Mor-Yosef S, Seidman DS, Rabinowitz R, Simon A, Schenker JG, Grand multiparity- a national survey. Isr J Med Sci; 1989 Nov;25(11):625-629.
16. C.L. Robertsa, U, C.S. Algerta, B. Peatd, D. Henderson-Smarta. Small fetal size: a risk factor for breech birth at term. International Journal of Gynecology & Obstetrics;1999;67:1-8.
17. Jensen DM, Damm P, Sorenson B, Mo lsted-Pedersen L, Westergaard JG, Ovesen P, et al. Pregnancy outcome and pre-pregnancy body mass index in 2459 glucose-tolerant Danish women. Am J Obstet Gynecol; 2003;189:239-44.
18. Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA; 2001;286:1195-200.
19. Shirley Hung, MPP, Donna Ruane Morrison, PhD, Leslie A. Whittington, PhD*,and Sara Beck Fein, PhD. Prepartum Work, Job Characteristics, and Risk of Cesarean Delivery. BIRTH; 2002;29(1):10-17.
20. Flamm BL, Quilligan EJ. Cesarean Section Guiding for appropriate utilization, 1st ed. New York: Spring Verlag; 1995. p.115.
21. Arash Hossein-Nezhad, Zhila Maghbooli, Ali-Reza Vassigh, Bagher Larijani*. Prevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian women. Taiwan J Obstet Gynecol; September 2007;46(3):236-242.
22. Rageth JC, Juzi C, Grossenbacher H. Delivery after previous cesarean: a risk evaluation. Swiss Working Group of Obstetric and Gynecologic Institutions. Obstet Gynecol; 1999;93:332-37.
23. Betul Bayir Talas, Sunduz Ozlem Altinkaya, Halit Talas1, Nuri Danisman, Tayfun Gungor. Predictive factors and short-term fetal outcomes of breech presentatiom: a case-control study. Taiwan J Obstet Gynecol; December 2008;47(4):402-407.
24. Phelan JP, Clark SL. Cesarean delivery, 1st ed. New York: Elsevier Science Publishing;1988. p. 99-107.
25. Jensen DM, Damm P, Sorenson B, Molsted-Pedersen L, Westergaard JG, Ovesen P, et al. Pregnancy outcome and prepregnancy body mass index in 2459 glucose-tolerant Danish women. Am J Obstet Gynecol; 2003;189:239-44.
26. Brost BC, Goldenberg RL, Mercer BM, Iams JD, Meis PJ, Moawad AH, et al. The Preterm Prediction Study: Association of cesarean delivery with increases in maternal weight and body mass index. Am J Obstet Gynecol; 1997;177(2): 333-41.
27. Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord; 2001;25:1175-82.
28. chlesselaman JJ, Paul D, Stolley MD. Case- Control Studies Design, conduct, analysis, 1st ed. New York: Oxford university press; 1982. p.1, 94
29. Ann Aschengrau, Georage R. Seage. Essential of epidemiology in public health. Boston: Jones and Bartett Publisher, Inc; 2003. p.222-225
30. Bettegowda VR, Dias T, Davidoff MJ, Damus K, Callaghan WM, Petrini JR. The relationship between cesarean delivery and gestational age among US singleton births. Clin Perinatol; 2008 Jun;35(2):309-23.
31. Poma PA. Correlation of birth weights with cesarean rates. Int J Gynaecol Obstet; 1999;65:117-23.
32. Oral E, Cada A, Gezer A, Kaleli S, Aydinli K, Öçer F. Perinatal and maternal outcomes of fetal macrosomia. Eur J Obstet Gynecol Reprod Biol; 2001;99:167-71.
|