|
Abstract
Fibromyalgia Syndrome (FMS) is a chronic condition causing pain, stiffness, and tenderness of the muscles, tendons, and joints. It is also characterized by restless sleep, tiredness, fatigue, anxiety, depression, and disturbances in bowel functions. The etiology of fibromyalgia remains unknown, but recent advances and discoveries have helped to unravel some of the mysteries of this disease. Research highlights some of the biochemical, metabolic, and immunoregulatory abnormalities associated with fibromyalgia. Management of FMS at the present time is very difficult as it has multiple etiological factors and psychological predispositions; however, a patient centered approach is essential to handle this problem.
Keywords: Fibromyalgia; Clinical features; Quality of life; Pathophysiology and management of fibromyalgia.
Introduction
Pain with its devastating and demoralizing effects remains a challenging problem for both patients and care givers.1 Fibromyalgia is one of the most common diseases affecting the muscles manifested with pain, stiffness, and tenderness of the muscles, tendons, and joints. The painful tissues involved are not accompanied by tissue inflammation.2,3 Therefore, despite potentially disabling body pain; patients with fibromyalgia do not develop tissue damage or deformity.4,5 The pain of fibromyalgia is generally widespread, involving both sides of the body. Pain usually affects the neck, buttocks, shoulders, arms, the upper back, and the chest. "Tender points" are localized tender areas of the body that can bring on widespread pain and muscle spasm when touched.6,7
FMS typically presents in young or middle-aged females as persistent widespread pain, stiffness, fatigue, disrupted unrefreshing sleep, and cognitive difficulties, often accompanied by multiple other unexplained symptoms, anxiety and/or depression, and functional impairment of daily living activities.8,9 There is an overall 6% to 15% prevalence rate in the United States with a five times greater incidence among women than men. In rheumatology clinics, the rate of new diagnosis is approximately 10% to 20%, whereas in non-specialized settings, the rate is 2.1% to 5.7%.10,11
Clinicians should be familiar with the signs and symptoms of fibromyalgia and diagnose the condition with minimum investigation.12 Since the symptoms of fibromyalgia wax and wane related to stresses,13 treatment (as with that of other chronic diseases) is an ongoing process rather than management of a single episode.
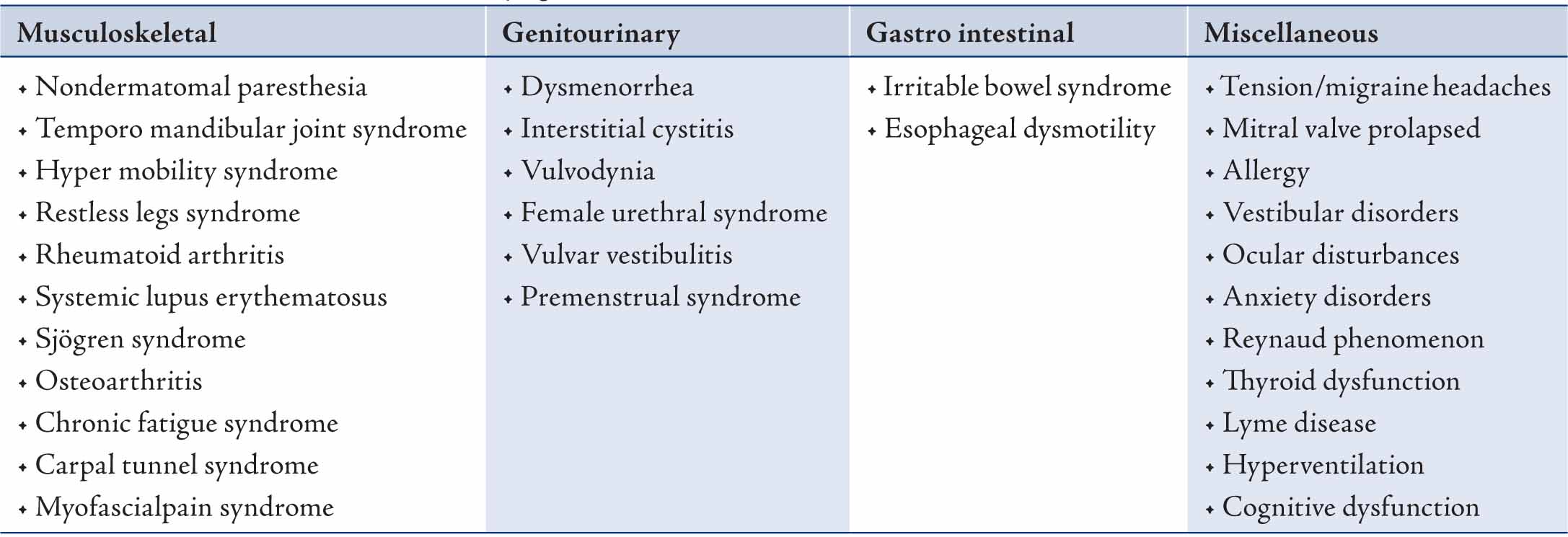
In terms of conditions associated with fibromyalgia; there are certain conditions associated with fibromyalgia.
Pathophysiology
Although the etiology remains unclear, characteristic alterations in the pattern of sleep and changes in neuroendocrine transmitters such as serotonin, substance P, growth hormone and cortisol suggest that regulation of the autonomic and neuro-endocrine system appears to be the basis of the syndrome. Fibromyalgia is not a life-threatening, deforming, or progressive disease. Anxiety and depression are the most common association.14 Aberrant pain processing, which can result in chronic pain, may be the result of several interplaying mechanisms. Central sensitization, blunting of inhibitory pain pathways and alterations in neurotransmitters lead to aberrant neuro-chemical processing of sensory signals in the CNS, thus lowering the threshold of pain and amplification of normal sensory signals causing constant pain.15,16
The frequent co-morbidity of fibromyalgia with mood disorders suggests a major role for the stress response and for neuroendocrine abnormalities. The hypothalamic pituitary axis (HPA) is a critical component of the stress-adaptation response.17 In FMS, stress adaptation response is disturbed leading to stress induce symptoms. Psychiatric co-morbidity has been associated with FMS and needs to be identified during the consultation process, as this requires special consideration during treatment.18
Table 1: Conditions associated with fibromyalgia. 17-19
Assessment of Fibromyalgia
Although fibromyalgia is the most common chronic widespread pain condition, it is often under diagnosed. The diagnosis of fibromyalgia has been shown to increase patient satisfaction and reduce healthcare utilization.
The assessment of Fibromyalgia is based on the criteria for the Classification of Fibromyalgia by the American College of Rheumatology, (ACR) 1990.19-21 The criterion involves:
• History of widespread pain has been present for at least three months.
• Pain in both sides of the body pain above and below the waist. Pain is considered widespread when all of the following are present:
• Pain in 11 of 18 tender point sites on digital palpation (both side of the body): Occiput (2),Low cervical (2),Trapezius (2), Supraspinatus (2), Second rib (2), Lateral epicondyle (2), Gluteal (2), Greater trochanter (2), Knee (2).
A tender point hurts only at the area where pressure (enough to cause the examiner's nail bed to blanch, or about 4 kg) is applied, and there is no referred pain. An instrument known as a dolorimeter can be used to apply exactly 4 kg of pressure over the tender points during the examination.22
New Diagnostic Criteria
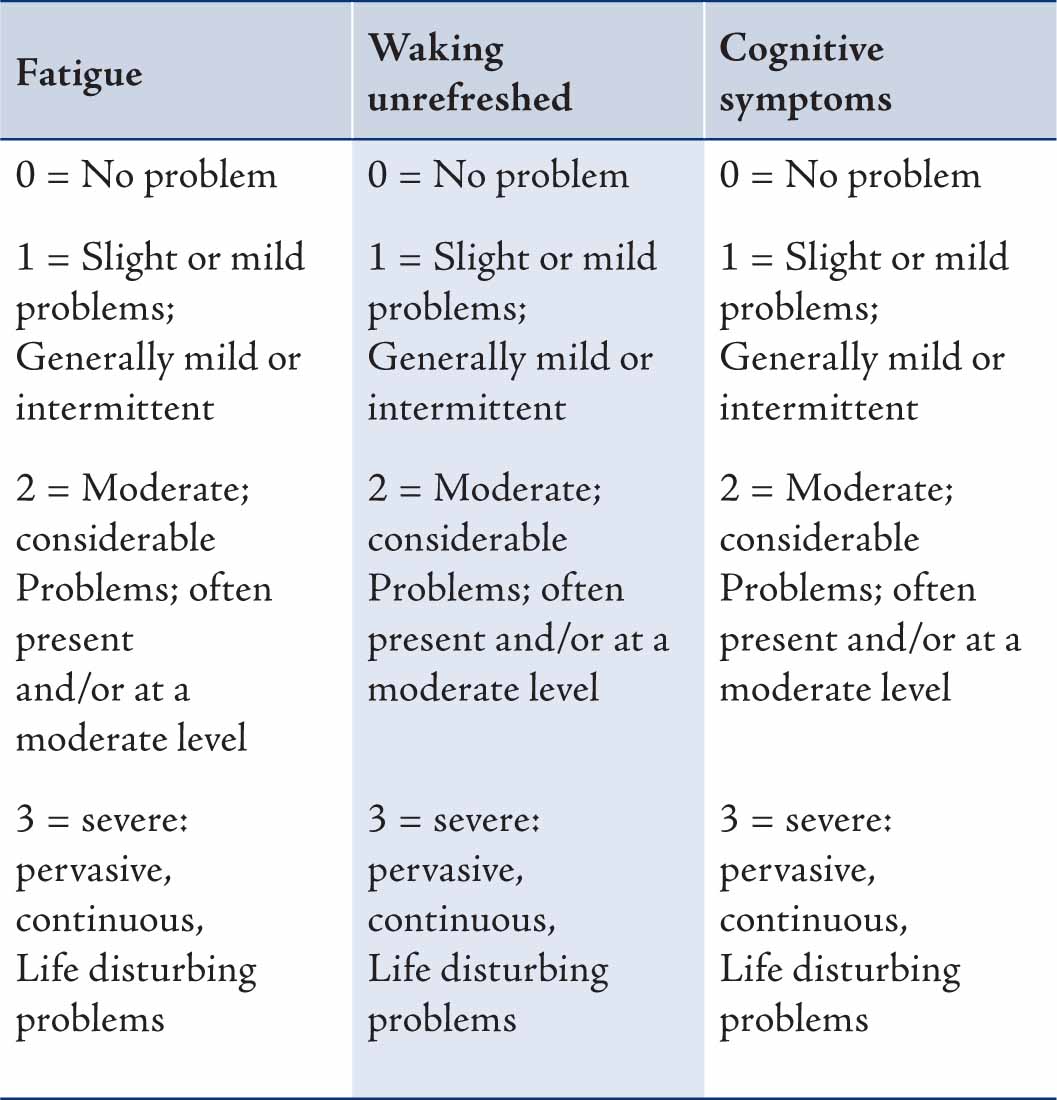
Recently, ACR is proposing a new set of diagnostic criteria for fibromyalgia that includes common symptoms such as fatigue, sleep disturbances, and cognitive problems, as well as pain (Table 2). The tender point test is being replaced with a widespread pain index and a symptom severity (SS) score. The new criteria appear in a one-page symptom checklist format that will hopefully be more suitable for use in the primary-care setting.23 A tender point evaluation is no longer required although a full physical exam is still recommended along with other diagnostic tests to identify causes for the patients' symptoms besides fibromyalgia. In place of the tender point count, patients (or their physician) may endorse 19 body regions in which pain has been experienced during the past week. One point is given for each area, so the score is between 0-19. This number is referred to as the Widespread Pain Index (WPI) and it is one of the two required scores needed for a doctor to make a diagnosis of fibromyalgia.
The second part of the score required to assess the diagnosis of fibromyalgia involves the evaluation of a person's symptoms. The patient ranks specific symptoms on a scale of 0-3. These symptoms include: Fatigue, Waking unrefreshed, Cognitive symptoms, Somatic (physical) symptoms in general (such as headache, weakness, bowel problems, nausea, dizziness, numbness/tingling, hair loss). The numbers assigned to each are added up, for a total of 0-12.
The diagnosis is based on both the WPI score and the SS score either:
• WPI of at least 7 and SS scale score of at least 5, OR
• WPI of 3-6 and SS scale score of at least 9.
Table 2: New ACR Diagnostic Criteria.
Laboratory Investigations
Laboratory testing, such as complete blood count, erythrocyte sedimentation rate, rheumatoid factor, antinuclear antibody, thyroid-stimulating hormone, T3, T4, creatinine phosphokinase, a serum muscle enzyme, vitamin D, ESR, CRP, renal function, and liver function tests are necessary to rule out other disorders. X-rays, blood tests, specialized scans such as nuclear medicine and CT scan muscle biopsy are normal in cases of fibromyalgia.
Management of Fibromyalgia
By the time many fibromyalgia patients reach the primary care setting or practice, they may have been seen by multiple healthcare providers. Patients are often frustrated or discouraged after receiving inadequate answers or diagnosis of their chronic ailments. Many are relieved to learn that there is an actual diagnosis and possible treatment options for their symptoms.24,25
Patients should participate in developing and initiating a care plan. Being a participant in their care will help the patient to assume control of their lives and focus on positive lifestyle changes rather than on chronic dysfunction. Patients must try to avoid exacerbating factors and limit anxiety and stress.26,27
A great majority of FMS patients can be managed well by Family Physicians in ambulatory care by managing stress, depression, pain and life style modification.28 CNS agents, antidepressants, muscle relaxants, or anticonvulsants are the most successful pharmacotherapies.
Therapeutic Measures in FMS
Medications have a limited role in FMS treatment to limit symptoms, so patients can participate in non-pharmacologic modalities that provide long-term disease management such as exercise, behavioral and education. Non pharmacologic therapies should be used when possible.29
Drugs
There are different pain medications which are useful in the management of FMS. Paracetamol, NSAIDs have been used but pain usually do not respond to them. Acetaminophen may ease the pain and stiffness caused by fibromyalgia. Besides analgesics, there are drugs used like antidepressant, anti convulsant, Dopamine agonist and Growth hormone.
Antidepressant Agents
Antidepressants have a long history in the treatment of chronic pain syndromes. The tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), or combinations of both, produce mild to moderate improvement in symptoms. Dosages should be gradually increased, not to exceed the recommended maximum for the drug. Even patients who are able to tolerate very small amounts of these medications may derive benefit from them. Antidepressants are most commonly used because of their effect on serotonin. Duloxetine, which is a Serotonin and Norepinephrine reuptake inhibitor is used successfully. Dopamine agonists (e.g., pramipexole), Sodium Oxybate and growth hormone therapy have recently been introduced for FMS.30,31
Life Style Modifications
Stress Management: Many patients with fibromyalgia have increased levels of stress and feelings of depression, anxiety, and frustration. Several treatment options are available such as cognitive behavioral therapy; including relaxation training, group therapy, and biofeedback, which are some of the useful options.32
Exercise: Physical activity can be taken in many ways, including activities such as walking, jogging or sports.33 Exercise is a way of responding to stress which allows the discharge of the energy the body is anticipating.34
Alternative Therapies: Chinese herbal medications, Chinese herbal tea, acupuncture, Tai-chi are the different modalities available but more research is required in these fields.35-38 It has also been suggested that acupuncture triggers the release of endorphins into the blood stream and are body's natural pain relievers.39
Conclusion
Fibromyalgia is a common rheumatologic syndrome characterized by heightened pain sensitivity, fatigue, sleep disturbance, and other symptoms as a result of dysregulation of neurophysiologic function. Many theories of etiology are under investigation. With the proper treatment coupled with a caring and well informed physician; patients with fibromyalgia should be able to improve function and reduce pain. A variety of neuro-modulatory agents are showing capability of beneficially affecting the symptom domains of patients with fibromyalgia. Treatment options currently exist to assist patients in relieving symptoms and preventing flare-ups. Prompt diagnosis and treatment of fibromyalgia patients may produce substantial improvement in quality of life.
Acknowledgements
The authors declare no conflict of interest and no funding was received for this work. All authors have contributed in conceptualization, and were involved in drafting the manuscript, critically revising it for important intellectual content and have given final approval of the version to be published.
|