Labor is a phenomenon that exists in many creatures and unlike other acute and chronic pain, the pain of labor does not correlate with any disease or pathology.1 Labor pain has been reported as the severest pain in humans. Known complications of pain are tension and anxiety, prolonged labor, and abnormal fetal heart rate, the incidence of cesarean delivery, neonate’s low Apgar score, and even long-term mental disorders.2-4 One of the most pressing concerns and fears for pregnant women is the pain of labor, which leads to an increase in the number of cesarean sections.5 Pain relief in labor is an important issue in obstetric care, however, as yet, there is no standard and accepted technique for the relief of that pain without side effects.4,6,7 Generally, there are two options for pain relief during labor, these use either pharmacological or non-pharmacological methods. Pharmacological methods have adverse side effects for the mother and fetus, whereas non-pharmacological methods are free from side effects.6,8
An example of a non-pharmacological method is acupressure, which is a traditional Chinese medicine where acupuncture points are stimulated by hands, fingers, thumbs, or small beads.9,10 This method acts according to the gate control theory where burning, massaging, and scratching can stimulate the large fibers responsible for transmitting nerve impulses to the spinal cord. A sustained stimulation can keep the gates of pain transmission closed, which may result in decreased pain.6 On the other hand, the stimulation of acupressure points using heat, needles, or pressure causes the release of endorphins.11
Acupressure is a non-invasive method which is used to augment labor, provide pain relief, and shorten delivery time.6 It increases the intensity of uterine contractions (based on Montevideo unit) without affecting the duration and intervals of uterine contractions and, eventually, reduces the duration of delivery.12 A variety of acupoints are useful in childbirth to induce and manage labor, and shorten delivery time, including LI4.6 Hugo point (LI4), or Large Intestine 4, is one of the 14 main meridians on the body and studies have shown that the stimulation of this point plays a key role in reduction of labor pain.7 Some studies have examined the effects of ice massage on LI4 and found that labor pain decreases.7,13 There are limited studies of this method, since non-pharmacological methods are not commonly used in Iran. We sought to evaluate the effectiveness of LI4 acupressure on labor pain and duration.
Methods
A single-blinded, randomized, control trial was carried out over a seven-month period, between October 2011 and April 2012, at Dr. Shariati University Hospital in Bandar Abbas, Iran. The trial was approved by the Ethics Committee of Hormozgan University of Medical Sciences (HUMS), Iran.
Singleton pregnant women at a gestational age of 37–42 weeks, cephalic presentation, 4–5 cm cervical dilatation with spontaneous onset of labor, and with no history of previous high-risk pregnancy, cesarean section, cephalopelvic disproportion, or narcotic use within the past eight hours were included in the study. Patients were excluded from the trial if they needed an emergency cesarean section, labor augmentation using oxytocin or pharmacological pain relief, or if they chose to withdraw.
Following selection, participants were given information about the study, and asked to give written consent. The subjects were randomly assigned to one of three groups: an acupressure group (acupressure on point L14), a touching group (touching point LI4 in order to eliminate any psychological effects caused by the presence of a researcher), or the control group (using no form of pain relief). Participants were kept in quiet rooms with similar conditions, and treated with routine care (including the use of a simple saline infusion, made immobile and lying in a lateral position). Selection of the sample size was according to similar studies where at least 35 participants were needed in each group. Figure 1 shows the method of participant allocation.
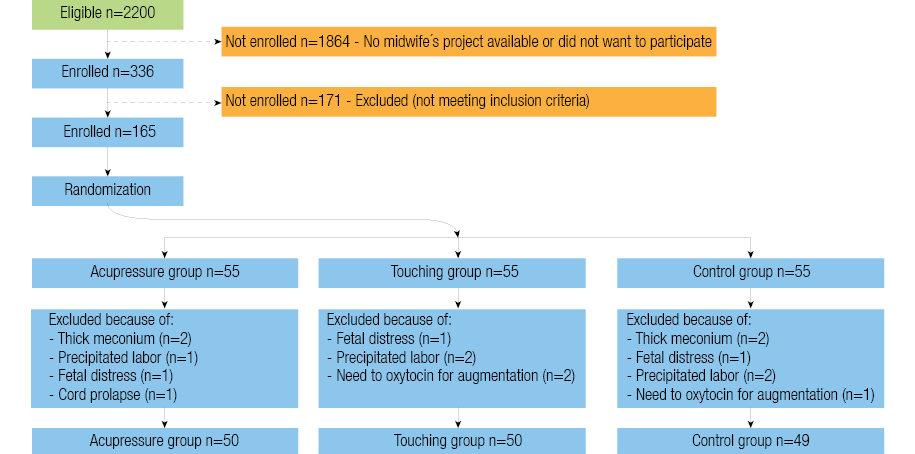
Figure 1: Flow chart of participant allocation.
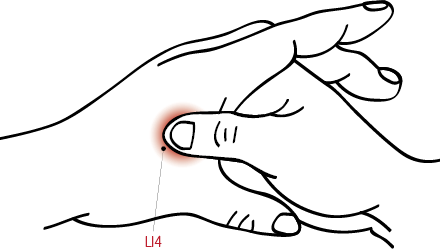
Figure 2: Accupressure was applied using fingers to hugo point LI4 located on the medial midpoint of the first metacarpal.
Pain intensity was measured using the visual analog scale (VAS). Researchers have previously approved the validity and reliability of the VAS as a standard tool for the assessment of pain intensity.12 Pain intensity was measured before and several times after the intervention at 30 minutes, one hour and every hour after intervention until the end of first stage of labor. In the acupressure group, a trained and registered midwife, certificated in the acupressure method, performed the treatment. Pressure was applied bilaterally within the contraction on Hugo point (LI4), which is located on the medial midpoint of the first metacarpal within the skin of the thumb and the index finger [Figure 2]. Prior to applying pressure the patient was asked to take a deep breath then a rotational and vibration pressure was applied for 60 seconds, she then received a 60 second rest, and pressure was repeated. This cycle continued for 30 minutes. Accurate location of the acupoint was confirmed when the subjects felt heaviness, pressure, tingling, or numbness in the area or a pleasant feeling. If the participant reported feeling severe pain at the site of pressure, the pressure was stopped temporarily and commenced after a few minutes. The sign of the intensity of the pressure was partial discoloration of the nail bed to white. In the touching group, the same point was touched but with no pressure applied. The 30-minute intervention time used is based on acupressure theory, which says the time needed to turn the energy in the body’s energy circuits is about 24 minutes.
VAS was used to estimate the pain intensity. Based on an 11-point scale where 0 indicated no pain and 10 indicated extreme and intolerable pain. At every stage of the trial, the participant ticked her pain level on a VAS. For each group the average pain intensity was calculated before and after the intervention, and then comparisons made between the groups.
The duration of the first stage of labor calculated the period from cervical dilatation 4–5 cm up to 10 cm cervical dilatation.
Data was analyzed using Statistical Package for the Social Sciences (SPSS) version 16.0. The chi-squared test was used for qualitative variables and for calculating the pain intensity changes in groups, and sphericity assumed test of analysis variance with repeated measurement and ANOVA to compare the duration of the first stage of labor.
Results
A total of 149 participants were enrolled across three groups, 50 in the acupressure group and touching groups, and 49 in the control group. There were no significant differences in demographic characteristics [Table 1] between the three groups (p=0.933). All three groups were similar in terms of gestational age, gravidity, parity, and cervical dilatation before intervention [Table 2].
Change in pain intensity was assessed for each group separately before intervention, at 30 minutes, and at one hour after intervention using analysis variance test with repeated measurement. The difference between the changes was calculated using Mauchly’s sphericity test. The result showed no significant changes in pain intensity in the acupressure group, but there were significant changes in the touch and control groups. In the acupressure group, pain intensity decreased and then remained constant after the application of pressure, but pain intensity was increased in the other groups, this means that acupressure had been more effective in controlling and reducing pain intensity than the other two groups
[Table 3]. In all three groups cervical dilatation showed a significant increase after intervention. However, those differences were not significant among all three groups. No statistically significant difference was observed in duration of first stage of labor (p=0.942), type of delivery (p=0.840) and Apgar scores at one and five minutes (p=0.621) between three groups.
Table 1: Comparison of demographic characteristics among the three groups.
|
Age (years)* |
25.46+4.48 |
25+6.35 |
25.48+5.7 |
0.990 |
|
Education n(%) |
|
|
|
|
|
Elementary |
3(6%) |
4(8%) |
3(6.1%) |
0.930 |
|
Junior high |
22(44%) |
27(54%) |
28(57.2%) |
|
Senior high |
21(42%) |
16(32%) |
14(28.3%) |
|
College or above |
4(8%) |
3(6%) |
4(8.2 %) |
|
Occupation n(%) |
|
|
|
|
|
Housewife |
47(94%) |
48(96%) |
48(97.9%) |
|
Employed |
2(4%) |
1(2%) |
- |
*mean ± SD
Table 2: Comparison of obstetric characteristics among the three groups (n=149).
|
Gestational age (weeks)* |
39.22+1.01 |
39.98+1.55 |
38.76+0.91 |
0.620 |
|
Parity Primiparous (n) |
24 |
23 |
25 |
0.460 |
|
Multiparous (n) |
26 |
27 |
24 |
|
*mean ± SD
Table 3: Comparison of mean visual analog scores
|
Before intervention* |
6.48+2.23 |
6.23+2.24 |
6.55+1.92 |
|
30 minutes after intervention* |
5.65+1.87 |
6.85+1.89 |
8.18+1.59 |
|
One hour after intervention* |
6.51+2.21 |
7.64+2.22 |
8.68+1.54 |
*mean ± SD
Discussion
In this study, we sought to determine the effect of acupressure on labor pain and the duration of labor.
Use of the acupressure technique on Hugo (L14) point was significantly effective in reducing pain intensity, while in the touching and control groups the intensity of pain significantly increased after the intervention. Acupressure through the gate control theory of pain and the secretion of endorphins reduces the severity of labor pain.7,11
The results of this study were consistent with other studies done in this field. Chung and colleagues14 studied the effect of L14 and BL67 acupressure on labor pain and uterine contractions and found a significant difference in pain intensity after the intervention . However, in the transitional labor phase no pain reduction was observed.
Studies by Enjezab et al,7 and Waters et al.13 showed that using ice massage on the Hugo point decreased pain intensity 30 minutes after intervention., In addition, Fan Qu studied the effect of electro-acupuncture on points L14 and SP6 on the intensity of labor and concluded that the technique could cause reduction in pain during the active phase.15 Another study showed that applying acupuncture on specific points such as LI4 compared to ineffective points could reduce labor pain in 30 minutes, one to two hours after the intervention.6
The common ground of all these studies was that using acupressure or acupuncture on specific points during the active phase of labor reduced labor pain, but during the transitional phase when pain intensity reaches its highest, those techniques had no significant effect. Chung et al.14 concluded that acupressure was not effective in reducing labor pain intensity at the latent phase of labor as well as the transition phase.
What distinguishes this study from other studies is the inclusion of two control groups where both placebo effects, indoctrination and physical presence, are completely removed. We used the pressure technique alone while other studies also used ice massage on the same point or in combination with other points to relieve pain.
Duration of labor did not differ between the three groups, suggesting that applying pressure on the L14 point reduces labor pain but does not disrupt the delivery process. This finding was consistent with the Enjezab’s7 study but Chung et al14 found that the duration of the first stage of delivery in the acupressure group was shorter than their other groups. Other variables examined in their study, were the delivery type and Apgar scores after the first and fifth minutes of birth, to determine how well the baby tolerated the birthing process and how well the baby is doing outside the mother’s womb, respectively. No differences were found between the groups.
A limitation of our study is that we did not assess maternal anxiety and fear, which are additional factors that can affect the severity of labor pain during labor.
Conclusion
Our study suggests that L14 acupressure is a suitable non-pharmacological technique that is easy to perform and effective in elevating pain, without causing adverse side effects for the mother or baby. It can be used to reduce pain during the active phase of labor rather than using pharmacological methods. According to the World Health Organization’s policies to reduce the rate of cesarean deliveries and promotion of safe childbirth, it is necessary to make childbearing pleasant and reduce maternal fear of natural childbirth using safe methods to reduce labor pain and increase the rate of vaginal delivery. In order to make this possible, midwives need training in using non-pharmacological techniques and the attitudes and policies of the hospitals need to be altered. Due to the simplicity and safety of the acupressure technique, additional research using a larger sample size and in combination with other techniques to apply pressure on different points of body is suggested.
Disclosure
The authors declared no conflict of interest. This research project was supported financially by Hormozgan Fertility and Infertility Research Center of Hormozgan University of Medical Sciences (HUMS).
Acknowledgements
We thank the midwives and participating women in the delivery ward at the Dr. Shriati University Hospital, for their cooperation.
references
- Lowe NK. The nature of labor pain. Am J Obstet Gynecol 2002 May;186(5)(Suppl Nature):S16-S24.
- Caton D, Corry MP, Frigoletto FD, Hopkins DP, Lieberman E, Mayberry L, et al. The nature and management of labor pain: executive summary. Am J Obstet Gynecol 2002 May;186(5)(Suppl Nature):S1-S15.
- Tournaire M, Theau-Yonneau A. Complementary and alternative approaches to pain relief during labor. eCAM 2007; 4 (4)409-417.
- Abbasi Z, Abedian Z, Fadaei A. The Effect of Back Massage on Pain Intensity during First stage of labor in primiparous women. Iranian Journal of Obstetrics, Gynecology and Infertility .2009 ;(4):39-47. (Persian)
- Shoorab NJ, Zagami SE, Mirzakhani K, Mazlom SR. The effect of intravenous fentanyl on pain and duration of the active phase of first stage labor. Oman Med J 2013 Sep;28(5):306-310.
- Lee MK, Chang SB, Kang DH. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med 2004 Dec;10(6):959-965.
- Enjezab B, khoushbin A, Bokaei M, Naghshin N. Effect of ice massage on Hugo point for reduction of labor pain. Journal of Shahid Sadoughi University of Medical Science and Health services 2008; 15(4):69-74. (Persian)
- Simkin P, Bolding A. Update on nonpharmacologic approaches to relieve labor pain and prevent suffering. J Midwifery Womens Health 2004 Nov-Dec;49(6):489-504.
- Mc Coffoery M, Beebe A. Pain Clinical manual for nursing practice. 1994; 1st edition. Mosby. London.
- Heydari P, Mozhdeh F, Mazloum SR, Tanbakouei K, Joudaki K. Effect of acupressure on labor pain intensity. Hakim 2008;11(2):39-46. (Persian)
- Borup L, Wurlitzer W, Hedegaard M, Kesmodel US, Hvidman L. Acupuncture as pain relief during delivery: a randomized controlled trial. Birth 2009 Mar;36(1):5-12.
- Heydari P, Mozhdeh F, Masloum SR, Tanbakouei K, Joudaki K. Effect of SP6 acupressure on length of labor. Iranian Journal of Obstetrics and Gynecology 2008;11(2):15-22. (Persian)
- Waters BL, Raisler J. Ice massage for the reduction of labor pain. J Midwifery Womens Health 2003 Sep-Oct;48(5):317-321.
- Chung UL, Hung LC, Kuo SC, Huang CL. Effects of LI4 and BL 67 acupressure on labor pain and uterine contractions in the first stage of labor. J Nurs Res 2003 Dec;11(4):251-260.
- Qu F, Zhou J. Electro-Acupuncture in Relieving labor pain. eCAM 2007;4(1)125-130.