|
Abstract
Coronary artery fistula is an uncommon finding during angiographic exams. We report a case series of five patients with congenital coronary fistulas. The first patient was 56 years old and had a coronary fistula associated with a partial atrio ventricular defect, the second patient was 54 years old and had two fistulas originating from the right coronary artery with a severe atherosclerotic coronary disease, the third patient was 57 years old with a fistula originating from the circumflex artery associated with a rheumatic mitral stenosis, the fourth patient was 50 years old and had a fistulous communication between the right coronary artery and the right bronchial artery, and the last patient was 12 years old who had bilateral coronary fistulas draining into the right ventricle with an aneurismal dilatation of the coronary arteries. Angiographic aspects of coronary fistulas are various; management is controversial and depends on the presence of symptoms.
Keywords: Coronary fistula; Coronary anomaly.
Introduction
Coronary artery fistula is an anomalous connection between a coronary artery and a major vessel or cardiac chamber bypassing the myocardial capillary system. Coronary fistula can be congenital or acquired. Acquired coronary fistulas may result from trauma, infection or iatrogenic injuries. Congenital coronary fistulas are more frequent and are classified by Greenberg et al. as termination anomalies.1 Coronary fistulas are mostly asymptomatic and represent an incidental finding during angiographic evaluation for coronary disease. This report describes a series of five patients with coronary fistulas and discusses the morphological variances, the associated anomalies and the management strategies.
Case 1
A 56-year-old man with a history of hypertension and smoking was admitted to the emergency room with recurrent episodes of chest pain and was referred to the Cardiology department for coronary angiography. Physical examination found a systolic murmur in the left sternal border. Electrocardiography showed a sinus rhythm with no pathological Q waves, ST segment, or T wave changes. The laboratory data showed an elevated level of troponin (7.29 ng/mL). Echocardiography revealed a partial atrioventricular canal defect with moderate pulmonary hypertension. The segmental wall motion was normal. The coronary angiography showed the coexistence of a coronary fistula and a coronary atherosclerotic disease. An arterial collector was draining blood from the left coronary system to the right atrium and the first diagonal artery presented a significant proximal stenosis (Fig. 1). We first decided to perform a percutaneous angioplasty. Coronary fistula closure would be considered if symptoms persist after treatment of the diagonal stenosis.
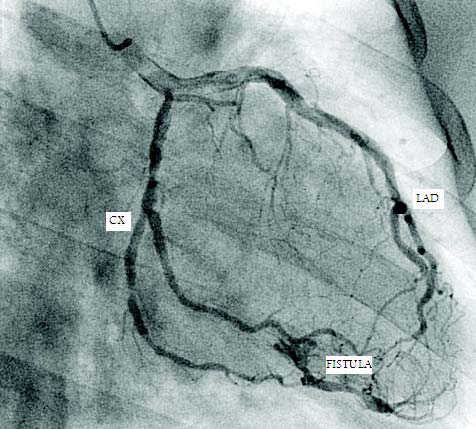
Figure 1: Right anterior oblique caudal view showing the fistulous communication between the left coronary system and the right atrium. LAD: left anterior descending artery; CX: circumflex artery
Case 2
A 54-year-old man with a history of heavy consumption of cannabis was admitted to the emergency room with severe chest pain of 20-hour onset. Physical examination was normal. Electrocardiography showed a sinus rhythm with Q wave in inferior leads and peaked T wave in anterior leads. The cardiac biomarkers were elevated (12 ng/mL for troponin and 123 IU/L for creatine kinase-MB), and echocardiography found an inferior akinesis with an ejection fraction of 45%. Coronary angiography showed a total distal occlusion of the right coronary artery coexisting with double coronary fistulas. Both fistulas originated from the occluded artery; the first draining into the right atrium, the second draining into the coronary sinus through a long collector, the feeding artery occlusion reduced remarkably the shunt of the distal fistula while the shunt of the proximal fistula was insignificant (Fig. 2). Investigations were completed by a dobutamine stress echocardiography. There was no viability in the inferior wall and medical treatment was conducted.
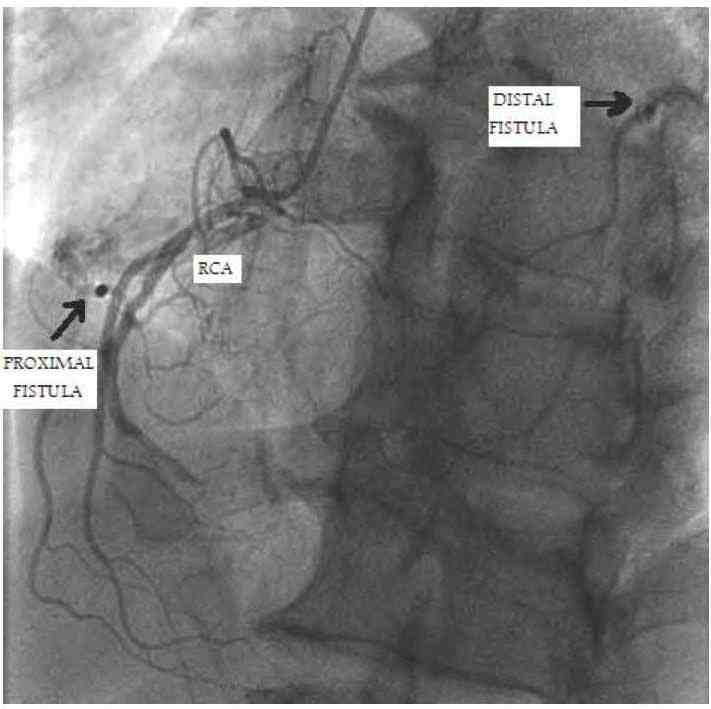
Figure 2: Left anterior oblique cranial view showing the two coronary fistulas originating from the right coronary artery and draining into the right atrium and the coronary sinus. RCA: right coronary artery
Case 3
A 57-year-old woman with a history of closed mitral commissurotomy was admitted to the Cardiology department for preoperative evaluation before a mitral valve replacement. The patient had marked exercise intolerance. Physical examination found an irregular pulse with a diastolic rumbling murmur. Electrocardiography showed an atrial fibrillation with a right bundle branch bloc, while echocardiography revealed a mitral stenosis with a mitral area of 0.7 cm2, the ejection fraction was 75%, the segmental wall motion was normal. The biological exams were unremarkable. Coronary angiography revealed a small fistulous communication between the proximal circumflex artery and the pulmonary artery (Fig. 3). The fistula was hemodynamically insignificant. Closure was not indicated and the patient only underwent mitral valve replacement.
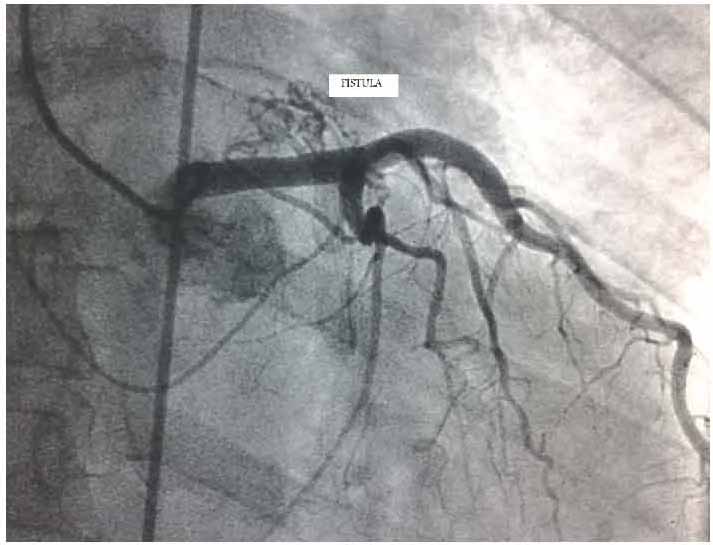
Figure 3: Straight posteroanterior view showing a coronary fistula originating from the circumflex artery.
Case 4
A 50-year-old woman with a history of complicated diabetes and hypertension was admitted to the Cardiology department for a silent myocardial ischemia screening. Physical examination was unremarkable. Electrocardiography showed a sinus rhythm with no pathological Q waves, ST segment, or T wave changes. The laboratory data showed normal levels of cardiac biomarkers. Echocardiography found a normal wall motion with an ejection fraction of 70%. The exercise test was inconclusive. The coronary angiography revealed a fistulous communication between the right coronary artery and the right bronchial artery with no evidence of atherosclerotic disease (Fig. 4). Regular follow-up was decided.
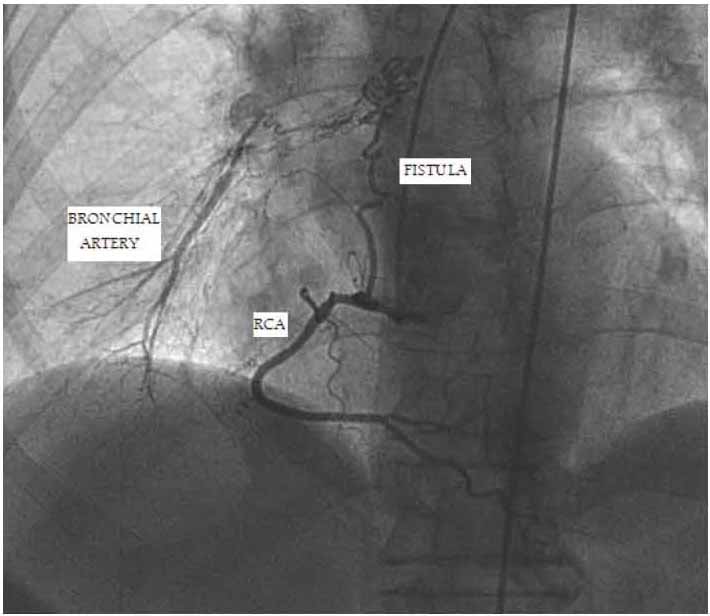
Figure 4: Left anterior oblique cranial view showing the coronary fistula between the right coronary artery and the right bronchial artery. RCA: right coronary artery
Case 5
A 12-year-old girl was admitted to the emergency room for febrile bronchitis. The patient had worsening shortness of breath with recurrent episodes of chest pain. Physical examination found continuous murmur in the left sternal border. Electrocardiography showed a sinus tachycardia. Echocardiography revealed dilated coronary arteries (13 mm for the right coronary artery and 9 mm for the left coronary artery). Coronary angiography showed an unusual aneurysmal dilatation of the left main trunk and the proximal left anterior descending artery. The proximal left anterior descending artery gives rise to an important vessel draining blood into the right ventricle (Fig. 5). The right coronary artery was also aneurysmal with fistula to the right ventricle. The patient underwent successful catheter closure for the fistulas using a vascular plug of 6 mm for the left coronary fistula and 8 mm for the right coronary fistula.
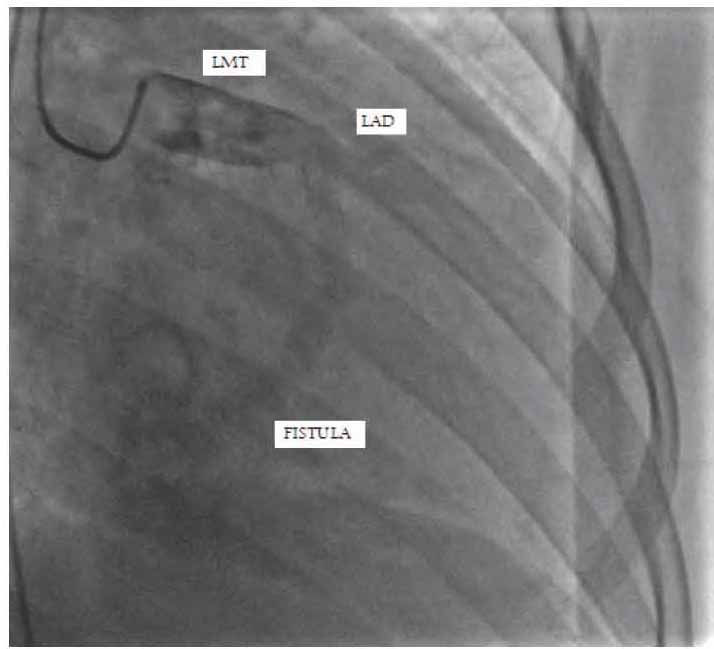
Figure 5: View of the coronary fistula between the proximal left anterior descending artery and the right ventricle. LMT: left main trunk; LAD: left anterior descending artery.
Discussion
Congenital coronary fistula is a rare malformation and accounts for only 14% of all coronary anomalies. The incidence is 0.002% among the general population, around 0.08% to 0.4% among congenital cardiac anomalies and 0.3% to 0.8% among angiographic series.2 Coronary fistula has been recognized since 1865.3 This abnormal communication seems to be consecutive to an embryologic persistence of primitive intratrabecular spaces.4,5 Congenital coronary fistulas are subdivided into two distinct types: solitary fistulas and coronary ventricular multiple microfistulas. Solitary fistulas are most common and represent 74% to 90% of all cases.6,7 The feeding artery is the right coronary artery in about 50% to 60% of cases, the left anterior descending artery in about 25% to 42% and the circumflex artery in 18.3%. The fistula may also originate from the left main coronary artery or from a diagonal or a marginal branch.8,9 Over 90% drain into the right side of the heart.6,10,11 All the presented fistulas drained into the right side.
Congenital coronary fistulas are associated with other congenital heart diseases in 20% to 45% of fistula cases. Associated anomalies include tetralogy of Fallot, atrial septal defect, patent ductus arteriosus, ventricular septal defect and pulmonary atresia with intact ventricular septum.12 In our series, only 1 of 5 patients had an associated congenital heart disease. The patient had a partial atrioventricular septal defect. To the author’s knowledge, the association with a partial atrioventricular septal defect has never been described, thus we are reporting it in the current series.
Clinical presentations vary depending on the type of fistula, shunt volume and site of the shunt. Patients are mostly asymptomatic especially during childhood. Some complications like myocardial ischemia, bacterial endocarditis, heart failure and arrhythmias may occur with increasing age.4,11,13,14 Myocardial ischemia may result from a decrease in coronary blood flow (coronary steal phenomenon) when the shunt is important, or may be due to a premature atherosclerosis. In our series, 2 of the 5 presented patients had an associated atherosclerotic coronary artery disease that explains the ischemic manifestations.
Management is controversial. Coronary fistula closure is indicated in symptomatic patients especially with heart failure or myocardial ischemia, and in asymptomatic patients with large or increasing left-to-right shunt.4,11 In our series, two patients were asymptomatic, two had ischemic manifestations explained by an associated atherosclerotic coronary disease and only one patient had symptomatic large fistulas that require closure. Closure options include surgery and percutaneous interventions. In 1945, Bjork and Crafoord reported the first surgical ligation of a coronary fistula.15 Surgery is safe and effective with good results. Surgical repair can be performed with or without cardiopulmonary bypass. Multiple surgical techniques have been used including epicardial ligation with or without division of the fistulous vessel, arteriotomy and suture closure of the fistula and intracardiac closure of the fistulous ostium by direct suture or with autologous pericardial patch.12 An associated coronary aneurysm can be resected, and the distal coronary flow can be maintained with either an interposition graft or a concomitant coronary artery bypass graft.16
Catheter closure is actually the procedure of choice; a number of devices have been used including occlusion coils, vascular plugs, umbrella devices, covered stents and Histoacryl resin.17 The choice of device depends on the anatomic characteristics of the fistula. Catheter closure can be applied to most cases. Features that may render coronary fistula unsuitable for this technique include those with extreme vessel tortuosity, multiple drainage sites and coronary branches at the site of optimal device positioning.18 In our series, 1 patient had a catheter procedure with successful closure of the two fistulas. The choice of modality was motivated by a suitable anatomy.
Conclusion
Coronary fistulas are uncommon anomalies, coincidentally detected during coronary angiography. Management depends on the anatomic characteristics and the presence of symptoms. Small or asymptomatic fistulous communications do not require closure and conservative medical management with long term follow-up is recommended; however, large and symptomatic fistulas must be treated. Percutaneous closure is emerging as a successful therapeutic strategy in patients with suitable anatomy.
Acknowledgements
The authors reported no conflict of interests and no funding was received for this work.
References
1. Greenberg MA, Fish BG, Spindola-Franco H. Congenital anomalies of the coronary arteries. Classification and significance. Radiol Clin North Am 1989 Nov;27(6):1127-1146.
2. Canga Y, Ozcan KS, Emre A, Kul S, Guvenc TS, Durmus G, et al. Coronary artery fistula: review of 54 cases from single center experience. Cardiol J 2012;19(3):278-286.
3. Krause W. Uber den ursprung einer accessorischen a coronaria aus der a pulmonalis. Z Ratl Med 1865;24:225-227.
4. Gowda RM, Vasavada BC, Khan IA. Coronary artery fistulas: clinical and therapeutic considerations. Int J Cardiol 2006 Feb;107(1):7-10.
5. Al-Maskari S, Panduranga P, Al-Farqani A. Coronary Artery Fistula with Heart Failure in Early Infancy. Oman Med J 2010 Jul;25(3) .
6. Fernandes ED, Kadivar H, Hallman GL, Reul GJ, Ott DA, Cooley DA. Congenital malformations of the coronary arteries: the Texas Heart Institute experience. Ann Thorac Surg 1992 Oct;54(4):732-740.
7. Tkebuchava T, Von Segesser LK, Vogt PR, Jenni R, Arbenz U, Turina M. Congenital coronary fistulas in children and adults: diagnosis, surgical technique and results. J Cardiovasc Surg (Torino) 1996 Feb;37(1):29-34.
8. Dodge-Khatami A, Mavroudis C, Backer CL. Congenital heart surgery nomenclature and database project: anomalies of the coronary arteries. Ann Thorac Surg 2000 Apr;69(4)(Suppl):S270-S297.
9. Huang YK, Lei MH, Lu MS, Tseng CN, Chang JP, Chu JJ. Bilateral coronary-to-pulmonary artery fistulas. Ann Thorac Surg 2006 Nov;82(5):1886-1888.
10. Said SA. Congenital solitary coronary artery fistulas characterized by their drainage sites. World J Cardiol 2010 Jan;2(1):6-12.
11. Qureshi SA. Coronary arterial fistulas. Orphanet J Rare Dis 2006;1(1):51.
12. Mangukia CV. Coronary artery fistula. Ann Thorac Surg 2012 Jun;93(6):2084-2092.
13. Raju MG, Goyal SK, Punnam SR, Shah DO, Smith GF, Abela GS. Coronary artery fistula: a case series with review of the literature. J Cardiol 2009 Jun;53(3):467-472.
14. Abusaid GH, Hughes D, Khalife WI, Parto P, Gilani SA, Fujise K. Congenital coronary artery fistula presenting later in life. J Cardiol Cases 2011;4:e43-e46 .
15. Biörck G, Crafoord C. Arteriovenous aneurysm on the pulmonary artery simulating patent ductus arteriosus botalli. Thorax 1947 Jun;2(2):65-74.
16. Said SM, Burkhart HM, Schaff HV, Connolly HM, Phillips SD, Suri RM, et al. Late outcome of repair of congenital coronary artery fistulas–a word of caution. J Thorac Cardiovasc Surg 2013 Feb;145(2):455-460.
17. Xu L, Xu ZY, Jiang SL, Zheng H, Zhao SH, Ling J, et al. Transcatheter closure of coronary artery fistula in children. Chin Med J (Engl) 2010 Apr;123(7):822-826.
18. Armsby LR, Keane JF, Sherwood MC, Forbess JM, Perry SB, Lock JE. Management of coronary artery fistulae. Patient selection and results of transcatheter closure. J Am Coll Cardiol 2002 Mar;39(6):1026-1032.
|