|
A 27-year-old female presented with severe dysmenorrhea and primary infertility. She had past history of post-traumatic splenectomy but was otherwise healthy. Her pelvic ultrasound was normal. She had a diagnostic hysteroscopy, laparoscopy, and a tubal patency dye test. On laparoscopy, there were multiple fleshy looking, red with blue hue nodules. In between, there were few scattered dark blue nodules on the anterior surface of the uterus, the visceral peritoneum, uterosacral ligaments, left ovarian fossa, and sigmoid colon. There were no significant adhesions. Some of those nodules were excised. The ones left behind were those in tricky anatomical locations like on the sigmoid colon and the ovarian fossa. The excised nodules were sent for histopathological confirmation. The patient made unremarkable recovery.
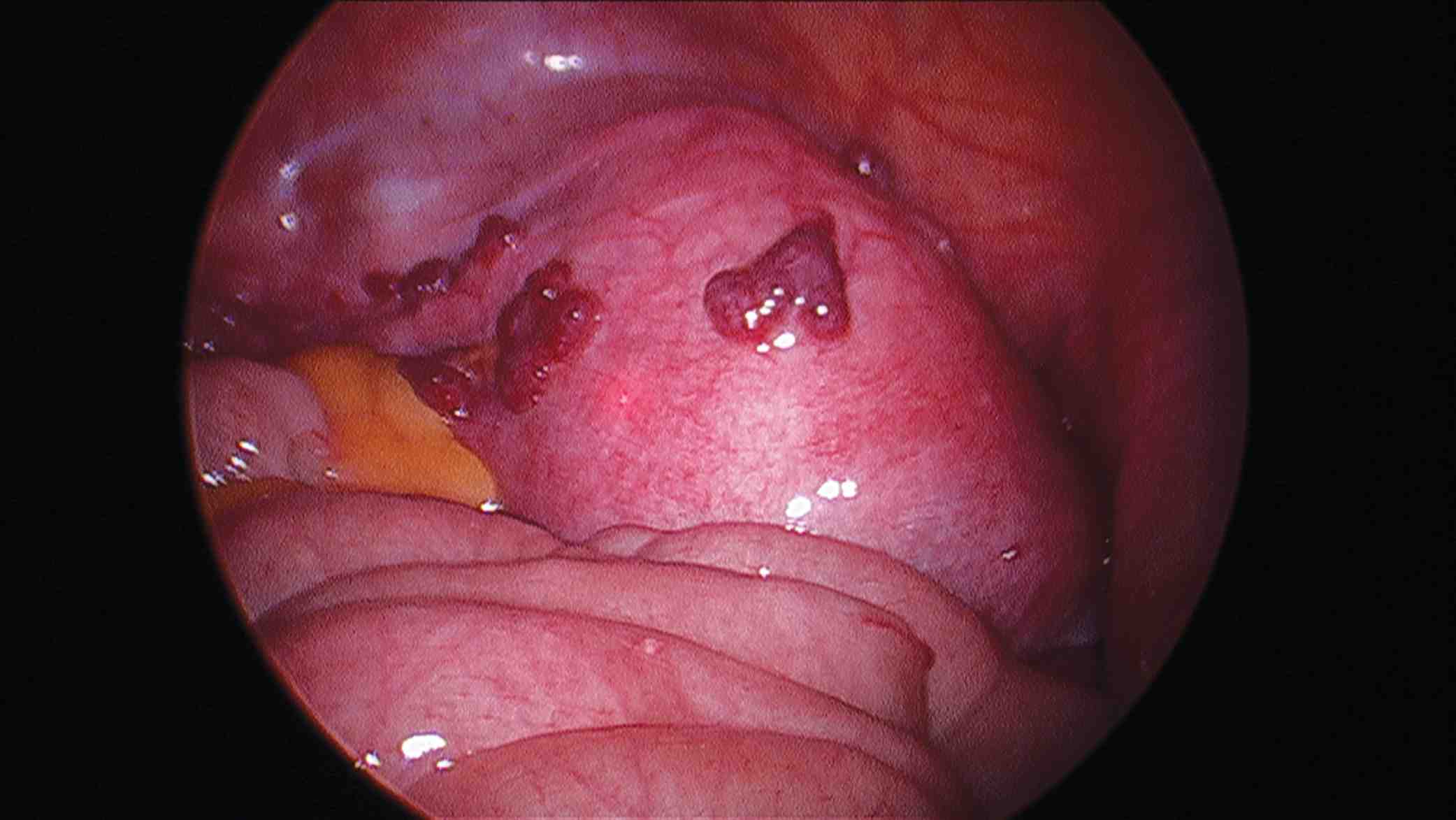
Figure 1: A laparoscopic picture: Distinctive nodules on the uterus.
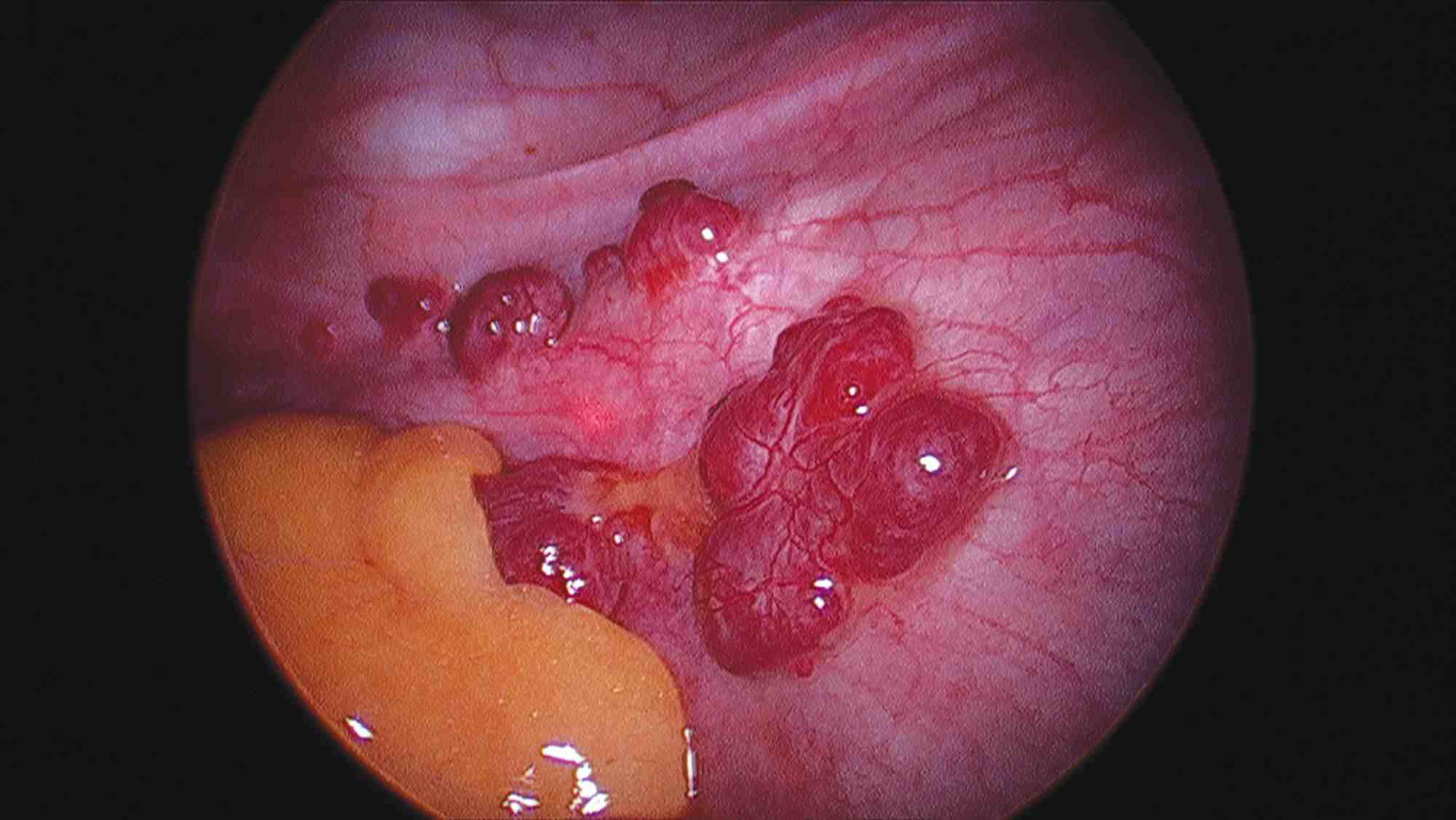
Figure 2: A laparoscopic picture: A close-up look at the nodules on the left side of uterus and broad ligament.
Questions
1. What is your differential diagnosis?
2. How do you differentiate between the possible diagnoses?
Answers
1. Possible diagnoses are; endometriosis and splenosis. The appearance is not consistent with malignant nodules.
Splenosis represents autotransplantation of splenic tissue after splenic trauma or surgery.1 It is presumed that spillage of the damaged splenic pulp into the adjacent thoracic, abdominal and/or pelvic cavities begins the seeding process.2,3 Also, hematogenous spread of the splenic pulps might explain the reported intrahepatic and intracranial splenosis.3,4 A third proposed mechanism is growth of erythrocytic progenitor cells in the liver in response to tissue hypoxia.3,5 Pelvic splenosis is usually asymptomatic.6 Rarely, it may cause pelvic pain, dysmenorrhoea and dyspareunia, or it may present with an adnexal mass mistaken for ovarian cyst, endometrioma or carcinoma.6,7 Its incidence is not accurately known but it is thought to occur in upwards of 65% of splenic rupture cases.3,8
2. History is important to elicit history of splenic trauma.
Details of the presenting gynecologic symptoms and directing the investigations to the known common etiologies make splenosis as an unlikely cause of the symptoms. Splenosis has distinctive intra-operative appearance. The nodules are of a reddish-blue appearance grossly, and can vary in shape and size.3 Endometriosis commonly has different appearances even in the same patient like red, blue, brown or black areas or nodules. It may also appear like white scarred or puckered areas indicating its deep impeded infiltrative nature. Splenosis nodules are sessile or pedunculated; whereas, the endometriotic ones are usually embedded in the serosal surfaces.3,8
Unlike endometriosis splenosis is vascular and thought to be immunologically functional.8 Unlike splenosis, however, endometriosis is usually associated with significant pelvic adhesions. If splenosis is suspected preoperatively, the diagnosis is made by scintigraphy using erythrocytes or platelets that are labeled specifically for splenic uptake.3,4,6 Its excision is not indicated unless thought to be symptomatic.6,8
Acknowledgements
The authors declare no conflict of interest.
References
1. Fleming CR, Dickson ER, Harrison EG Jr. Splenosis: autotransplantation of splenic tissue. Am J Med 1976 Sep;61(3):414-419.
2. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 29-1995. A 65-year-old man with mediastinal Hodgkin’s disease and a pelvic mass. N Engl J Med 1995 Sep;333(12):784-791.
3. Fremont RD, Rice TW. Splenosis: a review. South Med J 2007 Jun;100(6):589-593. Review.
4. Rickert CH, Maasjosthusmann U, Probst-Cousin S, August C, Gullotta F. A unique case of cerebral spleen. Am J Surg Pathol 1998 Jul;22(7):894-896.
5. Kwok CM, Chen YT, Lin HT, Su CH, Liu YS, Chiu YC. Portal vein entrance of splenic erythrocytic progenitor cells and local hypoxia of liver, two events cause intrahepatic splenosis. Med Hypotheses 2006;67(6):1330-1332.
6. Zvi V, Moti P, Mendlovic S, Arie H, Maymon R. Pelvic splenosis–a gynaecological challenge. Reprod Biomed Online 2009 Mar;18(3):421-423.
7. Zitzer P, Pansky M, Maymon R, Langer R, Bukovsky I, Golan A. Pelvic splenosis mimicking endometriosis, causing low abdominal mass and pain. Hum Reprod 1998 Jun;13(6):1683-1685.
8. Zvi V, Moti P, Mendlovic S, Arie H, Maymon R. Pelvic splenosis–a gynaecological challenge. Reprod Biomed Online 2009 Mar;18(3):421-423.
|