| |
Abstract
Lymphangiomas are rare tumors. When they occur at different locations, they are referred to as lymphangiomatosis. Here we describe a case of lymphangiomatosis presenting with chronic diarrhea and failure to thrive. Etiology, clinical presentations and treatment options will be discussed.
Keywords: Lymphangiomatosis; Tumor; Parenchymal; Propranolol.
Introduction
Intra-abdominal lymphangioma is a rare tumor with 90% of cases presenting at the age of less than 3 years.1 They have an equal prevalence between males and females in childhood.2 The common sites for lymphangiomas among the younger individuals are head, neck (these two comprise 50% of cases), axillae, or sometimes the parenchymal organs such as the liver. At times, they can occur at different foci and this is referred to as lymphangiomatosis.3,4 These are benign tumors, but due to their large size and the fact that they can occur in critical locations and become infected, they can cause significant mortality.5 Herein, we describe a case of systemic lymphangiomatosis in a 7-year-old Afghani girl, whose abdominal pain persisted after surgery but responded to treatment with propranolol.
Case Report
A 7-year-old Afghani female was referred to Mofid Children’s Hospital, Iran, with the clinical picture of bowel obstruction, having an abdominal mass with abdominal distension and a history of chronic diarrhea lasting for more than a year, which had discontinued a few days before the patient presented to the hospital. Meanwhile, the child suffered from failure to thrive. Physical examination revealed a mobile 2 × 2 cm abdominal mass, a few centimeters to the left of the umbilicus. (Figs. 1 & 2)
The lesion looked round and had a soft, homogenous-looking appearance. On palpation, it felt like a semi-solid mass, though it was not possible to determine the consistency of the mass solely based on the clinical findings. Coeliac disease work-up was negative and the patient had normal liver function tests. Ultrasonography revealed increased thickness in bowel wall loops and a huge hyper-echoeic heterogenous mass in the abdominal cavity. Barium enema showed colon dilatation; while abdominal X-ray and spiral CT with contrast showed soft tissue opacity in the small bowel mesentery pressuring bowel loops, compatible with a mass lesion. There was no invasion of mesenteric vessels; however, there were several mesenteric lymphadenopathies. Jejunal wall and colon wall were thickened. Multiple cysts were found in the spleen; moreover, a pancreatic pseudocyst and an inguinal canal lesion suggestive of cordal cyst were also observed. (Fig. 3)
The patient was not anemic and her 2 CBC tests were normal; one of them showed the following results; WBC was 4100, composed of neutrophils (76%), hemoglobin (12.3) and platelet count of 473000. All other laboratory tests and imaging studies including blood sugar, BUN and creatinine, electrolytes profile, liver enzymes and bilirubin level, uric acid level, coagulation studies, urinalysis and chest X-ray were all within normal ranges. Coeliac disease work-up was negative and liver function tests were normal; however, marrow biopsy revealed bone marrow involvement with decreased cellularity and proliferation of the lymphatic channels. Flow cytometry immunophenotype analysis was performed and revealed a lymphoid population of approximately 24% of total cells; half of which were mature T-cells with normal CD4/CD8 ratio. Seven to eight percent of cells were CD45 positive (blast cells) and expressed CD19 and CD20 positivity, but were negative for CD10. (Fig. 4)
Histopathological examination showed dilation and proliferation of lymphatics, muscular layer hypertrophy and fibro-adipose inflammation. This confirmed the diagnosis of lymphangiomatosis.
At laparotomy, a very large mass was found in the bowel mesentery and colon causing near complete obstruction close to the jejuno-ileal junction. Due to the fact that the mass was very large, a resection was performed in a way that would be compatible with the patient’s life. Bowel obstruction was partial and was more related to the compression, which was exerted by the mass externally to the lumen. Approximately 50 cm proximal to the tumor and approximately 50 cm distal; it was resected along with the tumor and small bowel mesentery and end-to-end anastomosis was performed. Surgery was uneventful but the patient’s abdominal pain persisted afterwards. After surgery, the patient did not complain of diarrhea and there was no further specific treatment for diarrhea. The patient was then prescribed propranolol (dose: of 1 mg/kg body weight/day). After 1 month, CT showed a significant decrease in tumor size. During this period, the patient’s pain also decreased to a great extent. (Fig. 5)
Discussion
Five to 6% of benign tumors of infancy and childhood are lymphangiomas.6,7 Only 10% of cases occur in internal organs.4 They are looked at as congenital dysplasia of lymphatic tissues resulting from embryological failure of the lymphatic system; this is by itself a consequence of lack of communication between lymphatics of the small bowel and the main lymphatic vessels; thus resulting in the formation of cystic lymphangiomas of the small bowel.8,9 Patients with mesenteric lymphangioma are often asymptomatic until the tumor enlarges. The clinical manifestations may vary; however, the most common symptoms include abdominal pain, incidentally identified mass, and distension. Pressure on the adjacent structures and complications including infection, perforation, torsion and rupture may also occur. If a lesion can be identified using ultrasonography, it will usually be observed as a cystic mass with multiple thin septa. In CT, they appear as uni- or multiloculated masses with septa of variable thickness.10 The definitive and optimal treatment for abdominal cystic lymphangioma is complete surgical excision. Often during surgery, similar to what happened in our case, it is necessary to resect parts of bowel due to the close relation between the cyst and the bowel wall. In asymptomatic patients, there is a 10% chance of spontaneous regression. Another option in cases of emergency would be aspiration and injection of sclerosing agents; however, they might present a high recurrence rate.8,10 Diffuse lymphangiomatosis is very rare and in this disease, there may be diffuse lymphangiomas in bones, spleen, liver, mediastinum and lung.11 When bone is involved, it is called Gorham’s disease, in which osseous matrix undergoes resorption and destruction. The presence of this syndrome makes treatment difficult and controversial.12
According to our patient’s age and clinical presentation, the main differential diagnosis was lymphoma. The other differential diagnosis was diffuse hemangioma, which can mimic the clinical presentation of the current case with abdominal mass and abdominal pain. Also, skin and liver may be involved in hemangioma and it can have a vascular appearance in histopathology. These diagnoses were ruled out using histopathological exam. Also, Gorham’s disease was ruled out after performing a bone survey, which yielded negative results.
Therapeutic options for diffuse lymphangiomatosis and Gorham’s syndrome are controversial. They include surgery, pleural drainage, radiotherapy, and local or systemic pharmacotherapy. Steroid pulse therapy, interferon alpha 2b and bevacizumab have been used effectively for treating this disease in some studies. Also, sirolimus has been found to be effective in certain cases.13-17 Recently, propranolol has been reported to be effective in a patient with intractable diffuse lymphangiomatosis, with a starting dose of 0.5 mg/kg/day and increased to a dose of 4 mg/kg/day. The mechanism though which propranolol exerts its effect is thought to be through vasoconstriction and reduction of vascular endothelial growth factor (VEGF) expression. Reduction in VEGF expression results in apoptosis of capillary endothelial cells.18
Due to the rarity of the disease and considering the fact that the best therapeutic options for this disease have not yet been completely verified; in order to treat this patient, we used an option which was potentially most economically affordable and posed the least risk of complications. It is worth mentioning that currently, the response to treatment with propranolol has been very effective; and the patient did not suffer from diarrhea anymore. We consider that had complete resection of the tumor been performed, the prognosis would have been good. However, in the case of any problems during therapy or insufficient expected response, patient’s treatment will be changed to other options including corticosteroids, Gleevec and/or re-operation.

Figures 1 & 2: Abdominal spiral CT scan with IV and oral contrast media, Infiltrative mass with considerable pressure effect on bowel loops and peripheral displacement of them in the small bowel mesentery

Figure 3: Gross appearance, thickening of abdominal wall.
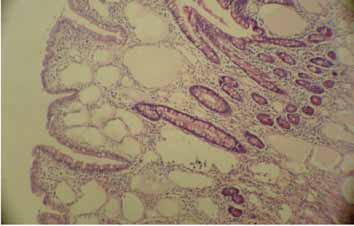
Figure 4: Many dilated vascular spaces in intestinal mucosa (H&E × 100).
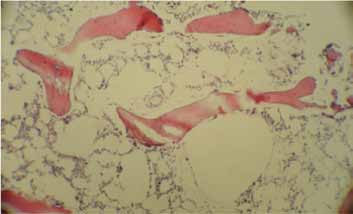
Figure 5: Many dilated vascular spaces in bone marrow (H&E × 100).
Conclusion
In summary, diffuse lymphangiomatosis is a rare disease which can involve soft tissue, bone and other viscera, and present as different clinical manifestations. Proper diagnosis requires a wide range of investigations and a high level of suspicion. Due to the rarity of this disease, different therapeutic options have not undergone comparison in clinical trials, there is not one best management option for such patients which can be easily determined, and the treatment options should be individualized according to disease severity and/or response to treatment. The current treatment plan for the patient is to continue propranolol and if necessary, adding/switching into other medications.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Bill AH Jr, Sumner DS. A unified concept of lymphangioma and cystic hygroma. Surg Gynecol Obstet 1965 Jan;120:79-86.
2. Rieker RJ, Quentmeier A, Weiss C, Kretzschmar U, Amann K, Mechtersheimer G, et al. Cystic lymphangioma of the small-bowel mesentery: case report and a review of the literature. Pathol Oncol Res 2000;6(2):146-148.
3. Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg 1985 Nov;120(11):1266-1269.
4. Konen O, Rathaus V, Dlugy E, Freud E, Kessler A, Shapiro M, et al. Childhood abdominal cystic lymphangioma. Pediatr Radiol 2002 Feb;32(2):88-94.
5. Singh S, Maghrabi M. Small bowel obstruction caused by recurrent cystic lymphangioma. Br J Surg 1993 Aug;80(8):1012.
6. Alqahtani A, Nguyen LT, Flageole H, Shaw K, Laberge JM. 25 years’ experience with lymphangiomas in children. J Pediatr Surg 1999 Jul;34(7):1164-1168.
7. Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg 2003 Apr;196(4):598-603.
8. Méndez-Gallart R, Solar-Boga A, Gómez-Tellado M, Somoza-Argibay I. Giant mesenteric cystic lymphangioma in an infant presenting with acute bowel obstruction. Can J Surg 2009 Jun;52(3):E42-E43.
9. Hwang SS, Choi HJ, Park SY. Cavernous mesenteric lymphangiomatosis mimicking metastasis in a patient with rectal cancer: a case report. World J Gastroenterol 2009 Aug;15(31):3947-3949.
10. Chung JC, Song OP. Cystic lymphangioma of the jejunal mesentery presenting with acute abdomen in an adult. Can J Surg 2009 Dec;52(6):E286-E288.
11. Ozeki M, Funato M, Kanda K, Ito M, Teramoto T, Kaneko H, et al. Clinical improvement of diffuse lymphangiomatosis with pegylated interferon alfa-2b therapy: case report and review of the literature. Pediatr Hematol Oncol 2007 Oct-Nov;24(7):513-524.
12. Barbagallo M, Incorpora G, Magro G, D’Amico S, Pavone V. Splenic lymphangiomatosis associated with skeletal involvement (Gorham’s disease): a new case and review of literature. Minerva Pediatr 2009 Apr;61(2):231-236.
13. Chang SC, Tu SH, Shi MY, Huang SH, Chen KM. Mesenteric lymphangioma causing bowel obstruction: report of one case. Acta Paediatr Taiwan 2002 Jan-Feb;43(1):43-45.
14. Timke C, Krause MF, Oppermann HC, Leuschner I, Claviez A. Interferon alpha 2b treatment in an eleven-year-old boy with disseminated lymphangiomatosis. Pediatr Blood Cancer 2007 Jan;48(1):108-111.
15. Takahashi A, Ogawa C, Kanazawa T, Watanabe H, Suzuki M, Suzuki N, et al. Remission induced by interferon alfa in a patient with massive osteolysis and extension of lymph-hemangiomatosis: a severe case of Gorham-Stout syndrome. J Pediatr Surg 2005 Mar;40(3):E47-E50.
16. Grunewald TG, Damke L, Maschan M, Petrova U, Surianinova O, Esipenko A, et al. First report of effective and feasible treatment of multifocal lymphangiomatosis (Gorham-Stout) with bevacizumab in a child. Ann Oncol 2010 Aug;21(8):1733-1734.
17. Reinglas J, Ramphal R, Bromwich M. The successful management of diffuse lymphangiomatosis using sirolimus: a case report. Laryngoscope 2011 Sep;121(9):1851-1854.
18. Ozeki M, Fukao T, Kondo N. Propranolol for intractable diffuse lymphangiomatosis. N Engl J Med 2011 Apr;364(14):1380-1382.
|
|