Autoimmune progesterone dermatitis (APD) is a rare condition that affects women in their childbearing age. It is characterized by a periodic type I or type IV hypersensitivity reaction to endogenous or exogenous progesterone resulting in a heterogeneous set of non-specific clinical manifestations ranging from urticaria to anaphylaxis.1,2
The diversity of clinical presentations infers that the immune system reacts to progesterone differently in different patients.3 The involvement of the oral cavity is exceedingly rare and has been reported in 1% of all APD cases.2 Manifestations can include lip swelling and non-specific mucosal erosions that can be confused with common conditions, such as erythema multiforme and vesiculobullous diseases.4 In almost all of the cases reported in the literature, the oral involvement of APD was part of a syndrome of dermatological and respiratory manifestations. This report describes a rare case of APD in whom the clinical manifestations were confined to the oral cavity in the absence of dermatological and non-dermatological manifestations.

Figure 1: Labial pigmentation on a 42-year-old woman.
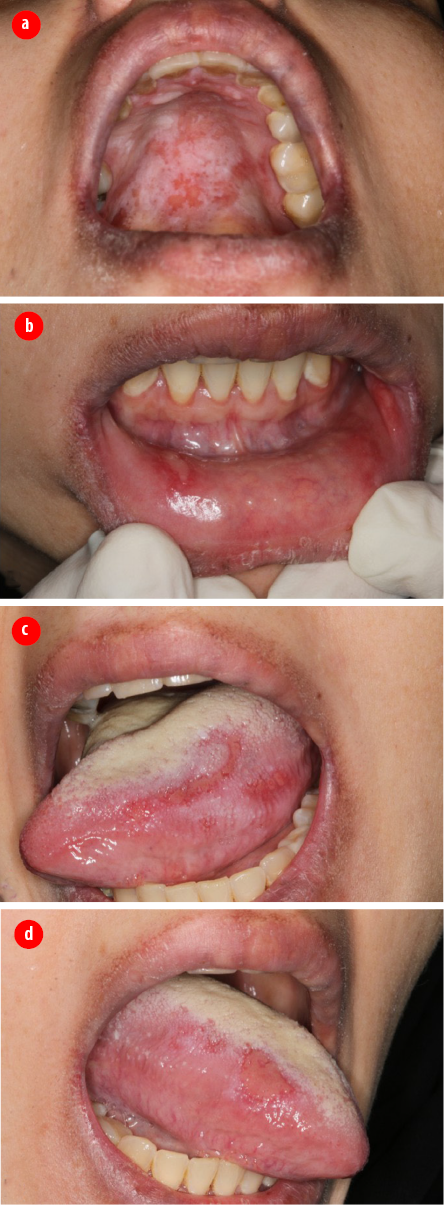
Figure 2: The ulcerative lesions affecting the
(a) hard palate, (b) lower labial mucosa, (c) right, and (d) left ventrolateral tongue.
Case report
A 42-year-old mother of four children presented to the Oral Medicine Clinic, University Dental Hospital Sharjah with recurrent and painful oral erosions. The erosions had started 12 months before her visit, and recurred with every menstrual cycle. The patient’s medical history was unremarkable. The oral erosions were preceded by a feeling of fullness in the lips lasting for 1-2 days before menstruation, followed by formation of painful labial and oral erosions. The pain increased gradually through menstruation, then spontaneously subsided at its completion. The patient had more than 14 medical and dental consultations without reaching a conclusive diagnosis. She had been treated with various systemic and topical medications, including antibiotics and antiseptic mouthwashes, without improvement. Clinical examination revealed mild skin pigmentation around the lips [Figure 1] and widespread oral mucosal erosions [Figure 2]. Blood investigations showed mild anemia, mild leukocytosis, and slightly elevated erythrocyte sedimentation rate [Table 1].
Table 1: Results of blood investigations performed during the ulcerative phase.
|
Red blood cells |
4.22 × 106/µL |
Normal |
|
Platelets |
359.000 × 103/µL |
Normal |
|
Hemoglobin (Hb) |
11.1 g/dL |
Low |
|
Hematocrit |
33.5% |
Low |
|
Mean corpuscular volume |
79.0 fL |
Normal |
|
Mean corpuscular Hb |
26.3 |
Low |
|
Mean corpuscular Hb concentration |
33.1 g/dL |
Normal |
|
Red cell distribution width |
23.5% |
High |
|
Mean platelet volume |
12.1 fL |
Normal |
|
White blood cells |
6.70 cells × 103/µL |
High |
|
Neutrophils |
74.9% |
High |
|
Lymphocytes |
19.3% |
Normal |
|
Monocytes |
5.1% |
Normal |
|
Eosinophils |
0.3% |
Normal |
|
Basophils |
0.4% |
Normal |
|
Erythrocyte sedimentation rate |
16 mm/hr |
High |
|
C-reactive protein |
< 2 mg/L |
Normal |
|
Antinuclear antibody |
Negative |
Normal |
|
Extractable nuclear antigens |
Negative |
Normal |

Figure 3: Compete and spontaneous resolution of the ulcerative lesions two weeks after menstruation.
(a) Hard palate, (b) lower labial mucosa, (c) right, and (d) left ventrolateral tongue.
The diagnosis of ulcerative stomatitis secondary to APD was made based on the clinical presentation and the absence of gross hematological abnormalities. The patient was prescribed dexamethasone elixir 0.5 mg/5 mL as a mouthwash three times daily throughout the menstrual phase. At two-week follow-up, the patient reported partial response to dexamethasone. Her examination showed complete healing of oral erosions [Figure 3].
The patient was referred to her gynecologist with the clinical diagnosis of APD. She was managed with tamoxifen 10 mg twice daily for three months. During subsequent follow-up appointments throughout the 18 months after the tamoxifen course, the patient reported no episodes of oral erosive lesions.
Discussion
APD is a rare condition that results from a hypersensitivity reaction to endogenous or exogenous progesterone.1 The first report of this condition is thought to be by Gerber in 1939.5 However, the term APD was first used by Shelley et al in 1964.6 APD affects women anytime between menarche and menopause; however, the majority of the reported cases are seen in women in their third decade.2 Several case reports have been published over the last few decades describing diversity and non-specific clinical presentations, including urticaria, dermatitis, vesiculobullous eruptions, dyspnea, and anaphylaxis.3 The term progesterone hypersensitivity was suggested as an alternative to APD in order to accommodate the non-dermatologic spectrum of clinical manifestations of this disease.1,2 The heterogeneity of APD is not only confined to clinical manifestations but also to disease severity that ranges from mild skin rash to life-threatening anaphylaxis.3 Despite this diversity, all cases have the pathognomonic feature associated with the cyclical rise in serum progesterone levels.
The etiology of APD is not clear, however, 45% of patients reported exposure to exogenous progesterone before the onset of the diseases, which suggests a sensitization process of the immune system to endogenous progesterone.2 Nguyen and Razzaque Ahmed summarized the predisposing factors associated with the onset and progression of the disease into the menstrual cycle (73%), pregnancy (15%), and hormonal therapy (9%).2
Oral involvement of APD in the form of non-specific erosions has been reported in only 1% of all APD reported cases.2,4 Ulcerative stomatitis as the sole clinical manifestation of progesterone hypersensitivity is exceedingly rare and has only been reported once in 1955.7
The diagnosis of APD is largely based on the unique association of clinical presentation recurring with every menstrual period. The diagnosis can be confirmed by the administration of an intra-dermal progesterone challenge.6 Other diagnostic tests include serological assay of immunoglobulins and complementary factors.2 A tissue biopsy is rarely indicated and is usually non-diagnostic.
Treatment options for APD are decided based on the severity of symptoms and can be categorized into three levels. First, symptomatic management using topical and systemic corticosteroids, with or without antihistamines. Second, the suppression of ovulation using oral contraceptive pills and gonadotropin-releasing hormone agonists1–3 or through a progesterone desensitization protocol.1 Finally, bilateral oophorectomy, which is considered the definitive treatment and is used in severe refractory cases.8,9
Tamoxifen is a selective estrogen receptor modulator that is commonly used to treat patients with breast cancers or to prevent their recurrence. Tamoxifen has been used to treat APD with variable treatment outcomes, ranging from partial8 to full remission.4,9 The mechanism by which tamoxifen works is believed to prevent progesterone secretion by suppressing ovulation. Tamoxifen is also believed to desensitize the body to progesterone, giving the patient permanent relief from APD. However, its use has an adverse effect of hypoestrogenemia.
The patient in this case report was initially treated with dexamethasone elixir 0.5 mg/5 mL as a mouthwash. Although this intervention gave the patient partial relief during the ulcerative phase, full remission was only achieved with tamoxifen. No lesions reappeared during the 18 months follow-up period after completing the tamoxifen course.
Conclusion
This report shows that ulcerative stomatitis can be the only clinical manifestation of an autoimmune reaction to progesterone. Clinicians should be aware of the possibility of APD-related stomatitis when women present with oral ulcerative lesions that appear concurrently with menstruation.
Disclosure
The authors declared no conflicts of interest. The patient of this case report consented on using the clinical images.
references
- 1. Foer D, Buchheit KM, Gargiulo AR, Lynch DM, Castells M, Wickner PG. Progestogen hypersensitivity in 24 cases: diagnosis, management, and proposed renaming and classification. J Allergy Clin Immunol Pract 2016 Jul-Aug;4(4):723-729.
- 2. Nguyen T, Razzaque Ahmed A. Autoimmune progesterone dermatitis: update and insights. Autoimmun Rev 2016 Feb;15(2):191-197.
- 3. Snyder JL, Krishnaswamy G. Autoimmune progesterone dermatitis and its manifestation as anaphylaxis: a case report and literature review. Ann Allergy Asthma Immunol 2003 May;90(5):469-477.
- 4. Moghadam BK, Hersini S, Barker BF. Autoimmune progesterone dermatitis and stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998 May;85(5):537-541.
- 5. Gerber J. Desensitization in the treatment of menstrual intoxication and other allergic symptoms. Br J Dermatol 1939;51(6):265-268.
- 6. Shelley WB, Preucel RW, Spoont SS. Autoimmune progesterone dermatitis: cure by oophorectomy. JAMA 1964 Oct;190(1):35-38.
- 7. Berger H. Ulcerative stomatitis caused by endogenous progesterone. Ann Intern Med 1955 Jan;42(1):205-208.
- 8. Ródenas JM, Herranz MT, Tercedor J. Autoimmune progesterone dermatitis: treatment with oophorectomy. Br J Dermatol 1998 Sep;139(3):508-511.
- 9. Cocuroccia B, Gisondi P, Gubinelli E, Girolomoni G. Autoimmune progesterone dermatitis. Gynecol Endocrinol 2006 Jan;22(1):54-56.