Pharyngocele, first described in 1886 by Wheeler et al,1 is an occupational overuse syndrome of the pharynx, and a rare pharyngeal pathology.2 Pharyngocele typically protrudes through the laxity in the thyrohyoid membrane at the site of passage of the internal branch of the superior laryngeal nerve through this membrane. Pharyngoceles are bounded anteriorly by the infrahyoid epiglottis, posteriorly by the thyrohyoid ligament, superiorly by the hyoid bone, and inferiorly by the superior margin of the thyroid cartilage. It usually occurs in the fifth to sixth decade of life.3 True lateral pharyngoceles that penetrate through the thyrohyoid membrane are rare, with less than 60 cases reported in the literature over the last 133 years. Pharyngoceles are usually asymptomatic and symptomatic patients may present with regurgitation of food, dysphagia, halitosis, pain, and nocturnal coughing.4 Pharyngocele and laryngocele are often misdiagnosed or interchangeably diagnosed. Both entities occur in glassblowers and wind instrument players.5 We present a case of bilateral pharyngocele imaged on plain radiography and contrast-enhanced computerized tomography (CECT)

Figure 1: Plain radiograph of the neck (anteroposterior and lateral views) shows a large volume of air filling the pharynx during the Valsalva maneuver, notably more on the left side compared to the right side.
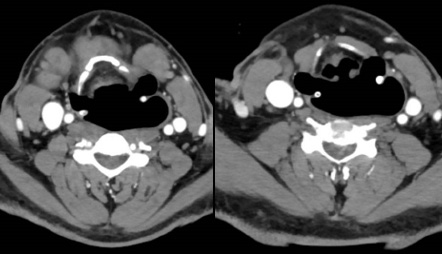
Figure 2: Axial contrast-enhanced computerized tomography section acquired during the Valsalva maneuver shows distended pyriform sinus with air-filled outpouching, extending across the thyrohyoid membrane on both sides (left more than right).
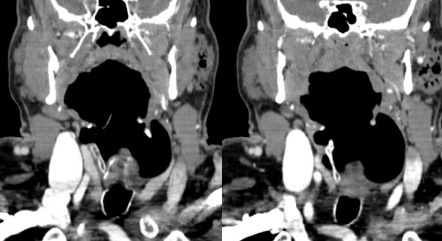
Figure 3: Coronal contrast-enhanced computerized tomography section acquired during the Valsalva maneuver shows significant distended pyriform sinus and hypopharynx with air-filled outpouching, extending across the thyrohyoid membrane on both sides (left more than right).
Case report
A 60-year-old male presented with complaints of bilateral intermittent neck swelling one year. He had associated complaints of intermittent food regurgitation. He had no difficulty in breathing or dysphonia. He has been a trumpet blower for the past 25 years by occupation. There was no relevant family history, no history of trauma, or past surgeries. At rest, head and neck examinations were unremarkable with no visible, palpable neck lumps or swelling. Characteristically, the neck swelling appeared only during the Valsalva maneuver, and it was soft in consistency and reducible. Laboratory investigations were unremarkable. Flexible laryngoscopy did not show any obvious abnormality. Plain radiograph of the neck (anteroposterior and lateral views) showed a large volume of air filling the pharynx during the Valsalva maneuver, notably more on the left side compared to the right [Figure 1]. CECT acquired during the Valsalva maneuver showed significant distended pyriform sinus and hypopharynx with air-filled outpouching, extending across the thyrohyoid membrane on both sides (left more than right) [Figures 2 and 3]. The patient was managed conservatively as his symptoms did not warrant any surgical management.
Discussion
Pharyngocele is characterized by protrusion of pharyngeal mucosa through the musculature of the tonsillar fossa, vallecula, or pyriform fossa. It may be congenital or acquired.5 Congenital pharyngocele is mostly due to the remnant of the branchial cleft. We can differentiate between congenital and acquired pharyngocele based on clinical history, as those with congenital pharyngocele usually do not have any occupational history that would cause increased intrapharyngeal pressure.6 Congenital pharyngoceles arising from the second branchial cleft to fourth branchial cleft remnant open in the lower pole of the tonsillar fossa and the piriform sinus, respectively.7 The acquired type of pharyngocele is due to prolonged increased intrapharyngeal pressure and pharyngeal wall weakness, and it is more common than congenital pharyngocele. The weakness of the pharyngeal wall in acquired pharyngocele may be due to advanced age or prior surgeries in the area. Pharyngoceles are also classified as upper and lower, based on pharyngeal wall weakness through which the hernia sac protrudes. Upper pharyngocele lacks a muscular layer in-between the superior and middle constrictor muscle, and lower pharyngocele lacks a muscular layer in-between the middle and inferior constrictor muscle.4 Increased intrapharyngeal pressure is common in professional glassblowers or wind instrument players and those with chronic cough.8 It may be unilateral or bilateral. In our patient, it was acquired and bilateral.
Close differential diagnoses include Zenker’s diverticulum, laryngocele, and jugular venous phlebectasia. The imaging modalities used to diagnose pharyngocele include plain radiography, barium swallow, ultrasound, and neck CT. A barium swallow can be used to locate the point of pharyngeal herniation. As our patient did not consent to barium swallow study, we proceeded with CT, which showed the large point of communication exquisitely. In Zenker’s diverticulum, the pharyngeal mucosa herniating between thyropharyngeus and cricopharyngeus muscles is not associated with intrapharyngeal pressure. Laryngocele means herniation of the laryngeal mucosa through the laryngeal ventricle. Jugular venous phlebectasia may present with similar complaints, and these can be differentiated by thorough clinical examination and ultrasound with Doppler imaging studies.9 Costa et al,2 found that 100% of acquired lateral pharyngoceles were seen in the wind instrument musicians, prompting their description as an occupational overuse syndrome. Conservative management is a treatment of choice for asymptomatic patients. It consists of maintaining good oral hygiene to avoid bacterial growth and use of a scarf around the neck while playing the trumpet to act as a truss. Surgical treatment is only advised for refractory cases or significant sized swellings and symptomatic cases. The surgical option of external extirpation of the hernia sac may be considered.5,9 Other minimally invasive include percutaneous injection pharyngoplasty and endoscopic suture pharyngoplasty.10,11
Conclusion
Acquired pharyngocele usually occurs in wind-blowing musicians. Pharyngocele and laryngocele are both can present with asymptomatic neck swelling and are close differentials. Thorough clinical examination and properly focused imaging during the Valsalva technique can differentiate pharyngocele from laryngocele, which has potential airway complications.
Disclosure
The authors declared no conflicts of interest. The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed. Permission of institutional ethical committee is also obtained.
references
- 1. Wheeler WI. Pharyngocele and dilatation of pharynx. Dublin J Med Sci 1886;82:349-357.
- 2. Costa MM, Alvite FL. Lateral laryngopharyngeal diverticula: a videofluoroscopic study of laryngopharyngeal wall in wind instrumentalists. Arq Gastroenterol 2012;49(2):99-106.
- 3. Naunheim M, Langerman A. Pharyngoceles: a photo-anatomic study and novel management. Laryngoscope 2013 Jul;123(7):1632-1638.
- 4. Daultrey C, Colley S, Costello D. “Doctor I have a frog in my throat”: Bilateral pharyngoceles in a recreational trumpet player. J Laryngol 2013 Jan;3(1):18.
- 5. Edmiston R, Hariri A, Karagama Y. The trumpet player with a swelling in the neck. BMJ Case Rep 2015 Mar;2015:bcr2015209487.
- 6. Katsinelos P, Chatzimavroudis G, Pilpilidis I, Zavos C, Lazaraki G, Soufleris K, et al. Congenital bilateral pharyngoceles: an unusual case of upper dysphagia. Dysphagia 2008 Mar;23(1):98-100.
- 7. Leuchter I, Becker M, Dulguerov P. Bilateral pharyngocele surgery under local anesthesia: let the patient help the surgeon. Laryngoscope 2013 Jun;123(6):1444-1447.
- 8. Oishi Konari M, Zapater Latorre E, Mosquera Lloreda N, Basterra Alegría J. Pharyngocele. Acta Otorrinolaringol Esp 2013 Sep-Oct;64(5):369-370.
- 9. van de Ven PM, Schutte HK. The pharyngocele: infrequently encountered and easily misdiagnosed. J Laryngol Otol 1995 Mar;109(3):247-249.
- 10. Yılmaz T, Cabbarzade C, Süslü N, Bajin MD, Günaydın RÖ, Özer S, et al. Novel endoscopic treatment of pharyngocele: endoscopic suture pharyngoplasty. Head Neck 2014 Aug;36(8):E78-E80.
- 11. Hu A, Merati AL. Percutaneous injection pharyngoplasty for the treatment of a pharyngocele. Ear Nose Throat J 2012 Feb;91(2):66-68.