Tobacco smoking contributes to major health issues across the globe as well as in the UAE.1 Familiar though much of the evidence seems, it is worth revisiting. Tobacco smoking does not only cause cancer (lung, bladder, tongue, and throat), but it can damage almost every organ in the body and is highly associated with stroke, circulatory diseases, cardiovascular disease (CVD), and other severe respiratory diseases, for example, influenza and pneumonia.2 Globally, tobacco kills more than 7 000 000 individuals every year. More than 6 000 000 of those deaths are a consequence of direct use of tobacco whereas, around 890 000 are the result of non-smokers exposed to second-hand smoke.3 A national agenda by the UAE established for the health system includes 10 specific goals to be achieved by 2021, five of them are related to non-communicable diseases: tackling CVD, cancer, diabetes, obesity, and smoking.4 According to the 2010 Ministry of Health and Prevention report, the prevalence of smoking any tobacco product is 21.6% among men and 1.9% among women.5 Previous literature indicates that roughly about three-quarters of smokers aim to quit. However, smoking is vastly addictive, and the cessation of smoking is hard, with recurrent relapses common among people planning to quit smoking.1 Continuous research on the efficiency of different interventions related to smoking cessation is underway. Cytisine, varenicline, bupropion, and nicotine replacement therapy (NRT) have been demonstrated to progress the possibility of quitting, with varenicline signifying the highest advantage. Nevertheless, such products tend to have considerably low product satisfaction and customer appeal.4 Evidence indicates that smoking cessation and its psychosocial interventions, for example, self-help interventions, telephone support, and behavioral counseling are operative. These interventions are pooled with pharmacotherapy that mainly enriches the degree of success to give up smoking.6,7
Controlling the use of tobacco is a foremost public health concern, particularly in developing nations. Healthcare professionals hold an opportunity and the means to help reduce the prevalence of smoking as well as encourage smokers to quit smoking through cessation and prevention intervention.8 Short-term counseling related to health problems are associated with cigarette and tobacco use while the importance of quitting is one of the most useful behavioral interventions that can be used to help smokers quit. Globally, healthcare professionals lack the training to counsel individuals and do not offer effective treatment and counseling to the people.9 Healthcare providers in the UAE have reinforced smoking as a major health priority, supported anti-tobacco policies, modeled good health, and offered clinical interventions to individuals who smoke.
This review aims to offer a comprehensive understanding of the health risk of tobacco smoking and aims to review previous evidence about the prevalence and interventional/counseling practices offered in the UAE.
Methods
The study used ‘systematic review’ as a research approach. To locate primary studies relevant to the aims and objectives of the study, we performed a systematic search of the PubMed and Scopus electronic databases covering the period between 2007 and 2017 [Box 1]. Search strings for conducting the electronic searches were made to retrieve targeted evidences by combining the following Medical Subject Headings (MeSH) terms, including ‘smoking’, ‘tobacco use’, ‘health risk’, ‘cigarette smoking’, ‘prevention’, ‘prevalence’, ‘interventions’, ‘counseling’ ‘UAE’, ‘Dubai’, ‘Ras Al Khaimah’, ‘Abu Dhabi’, ‘Ajman’, ‘Al Ain’, ‘Sharjah’, ‘Fujairah’, and ‘Umm Al Quwain’. Furthermore, reference lists of the chosen studies were perused to categorize the relevant citations manually.
Box 1: Search strategy.
|
Date: 2007–2017 |
|
1. MeSH descriptor: Cigarette smoking (titles/abstract). |
|
2. MeSH descriptor: Tobacco use (titles/abstract). |
|
3. MeSH descriptor: Smoking (titles/abstract). |
|
4. MeSH descriptor: Prevalence, Smoking, Tobacco, Health risk, Cigarette smoking, Prevention, Intervention, or Counseling. |
|
5. MeSH descriptor: UAE, Dubai, Ras Al Khaimah, Abu Dhabi, Ajman, Sharjah, Al-Ain, Fujairah, or Umm Al Quwain. |
|
#1, #2, or #3, and #4 and #5. |
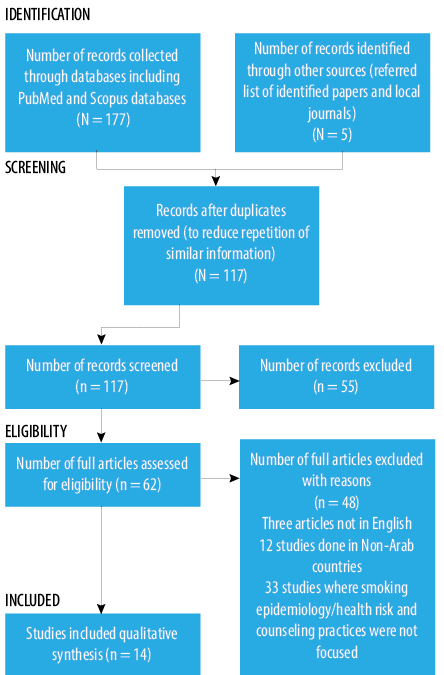
Figure 1: Schematic representation of the studies selected for the integrative review of the literature.
For inclusion in the study, publications had to meet the following criteria: primary research articles published in peer-reviewed journals; studies either estimates the prevalence of smoking in the population or determines its possible health risk or interventions; and published in the English language between 2007 and 2017. Figure 1 specifies the search-related process followed in detail. Articles not available in the English language, including a non-relevant topic, or not conducted in the UAE were excluded from this review. The search was limited to English language articles only because articles mainly in other languages could not be translated feasibly.
Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines, retrieved citations were screened, duplicates were eliminated, and the remaining citations were organized. The investigator then examined the abstracts and titles and only relevant articles were recovered. Further, two researchers independently reviewed as well as screened the titles, abstracts, and full texts for inclusion, reaching a strong agreement (Cohen’s Kappa = 0.83). This confirmed that only articles pertinent to the aims and objectives of this review were included. The selected articles primarily focused on reviewing the prevalence of tobacco smoking, determining its possible health risk, and interventions precisely involving the UAE population. Overall, 182 records were identified, 117 of which remained after duplicates were removed. The two researchers then independently reviewed as well as screened the articles and 48 were further excluded at this stage. In total, 14 articles were then retrieved as full text, synthesized, and evaluated for cautious reading and evaluation.
Results
The results of the literature search yielded 14 published papers that had been conducted in the UAE with regards to smoking intervention, prevalence, or health risk. The study results are discussed below, including epidemiology, counseling practices/interventions, and the health effects of tobacco smoking.
Prevalence of tobacco smoking
Six prevalence studies were conducted in different states of the UAE: two studies were conducted in Dubai,10,11 three in Abu Dhabi,12–14 and one in Ajman.15 Of the six studies reporting on the prevalence of tobacco smoking, five were cross sectional,10–12,14,15 and one was a cohort longitudinal study [Table 1].13
More men smoked tobacco in the included studies than women. A cross-sectional descriptive study conducted in Abu Dhabi demonstrated that Arab expatriates (31.9%) had the highest smoking prevalence, followed by other nationals (21.6%) and expatriates (22.6%). More men (19.2%) were cigarette smokers compared to women (3.5%). Arab expatriate women reported a higher prevalence of cigarette smoking (31.4%) than national women (0.7%).12 A cohort study conducted in Abu Dhabi specified significant factors that were associated with ‘substance use’ such as marital status and smoking.13 A large cross-sectional study conducted in Abu Dhabi reported ‘modes of tobacco consumption’ and its prevalence in the UAE. Overall, smoking prevalence reported in males was 24.3% and 0.8% in females. The highest prevalence was reported in males aged 20–39 years. Smoker’s mean age was 32.8±11.1 years; 35.7±12.1 in females and 32.7±11.1 in males. One of the most common forms of tobacco use included cigarette smoking (77.4%) followed by 15.0% midwakh use (a small pipe used for smoking tobacco), 6.8% waterpipe, and 0.66% cigar use.14 A school-based intervention program conducted among 2457 students aged 10–20 years found that tobacco users made up 14.6% of participants, of which 2.2% used water-pipes and 11.2% smoked cigarettes. The primary reasons leading to smoking included peer influence (21.9%), stress relief (22.5%), and for the experience (29.4%).10 While, dokha smoking (a tobacco product, including dried and finely shredded tobacco flakes mixed with spices and herbs) prevalence among secondary school students (precisely males) in Ajman was reported to be high (39% ever smokers, 36% ever dokha smokers, and 24% current dokha smokers).15 Similarly, high school student residents in Dubai reported a prevalence of 23.4%.11
Interventions/counseling practices
Tobacco addiction is the most important preventable cause of mortality and morbidity. Interventions/counseling practice studies addressed best practices for effective and brief treatment and counseling for tobacco addiction. Most importantly, smoking cessation interventions are a cost-effective way of reducing ill-health and preserving life. Of the five studies reporting tobacco cessation intervention, all were cross-sectional studies16,18–20 except one which included a case-control study conducted in Abu Dhabi.17 The interventional study explored the most readily available and common interventions that take the form of brief interventions/health education on tobacco cessation,18–20 telephone counseling, group behavior therapy programs, and individual behavioral counseling.16,17
A cross-sectional survey conducted in Sharjah, Dubai, and Abu Dhabi indicated that the young age population is of specific interest because these are the most effective groups for targeting smoking prevention programs. The study, therefore, assessed the delivery of smoking related preventive counseling in young Arab population (age 9–24 years) and examined counseling behaviors and barriers to counseling.16 Barriers to counseling involved lack of patient educational materials, lack of time, and lack of community resources. Another cross-sectional mail survey was undertaken in a random sample of general practitioners (GPs) in Sharjah, Dubai, and Abu Dhabi to document cessation-counseling practices.19 Despite favorable attitudes and beliefs regarding cessation counseling, only 47% of GPs stated that they hold adequate skills to benefit and support patients to quit smoking.
Health risks of tobacco smoking
Of the three studies reported for health risks of tobacco smoking, two were cross-sectional and one was a quasi-experimental study conducted in different regions of the UAE [Table 1]. The findings of these studies demonstrated that tobacco smoking causes high blood pressure,23 influence the epithelial dysplasia status,22 and is a significant predictor of dry cough and wheeze.21
Table 1: Characteristics of the included research studies.
|
Summary of study features —Prevalence |
|
|
Aden et al, 201310 |
To examine the
self-reported prevalence of tobacco use (including Medwakh, cigarette, and waterpipe) among applicants who were registered to Abu Dhabi’s Premarital Screening program in 2011 |
Cross-sectional descriptive study |
Abu Dhabi |
9337 adult applicants;
2309 self-reported adult’s smokers registered in the screening program /
Adults (18 years and above) population of nationals and expatriates |
Smokers: 19.2% of men; 3.5% of women
Medwakh (hand-held pipe) smokers: men (11.5%) and women (0.1%) [Women less likely to smoke medwakh]
Highest medwakh smoking prevalence: 16.1% UAE Nationals
Current smokers: 24.7%;
2.5% smoked a combination of cigarettes
5.9% smoked medwakh
11.5% smoked cigarettes
4.8% smoked waterpipe
Waterpipe smoking: 6.8% men; 2.8% women; Arab expatriate men (10.2%) |
To reduce the consumption of tobacco and tobacco-related mortality and morbidity: tobacco control laws should be reinforced including increase in tobacco taxes, and implementing clean indoor air laws. Moreover, targeted health education programs are needed. |
|
Alblooshi et al,
201611 |
To address the substance use disorder |
Cohort study/
one-to-one questionnaire interview session |
National Rehabilitation Centre in Abu Dhabi |
251 UAE nationals-male patients |
95.6% were current smokers;
4.4% had quit smoking
Substance use disorder was correlated with smoking and marital status
However, most commonly used substances included alcohol and opioid |
Additional focus is required on the educational and prevention programs from the use of drugs.
Increased utilization of mass media is needed to promote awareness of the preventions programs as well as to highlight the risks posed by both newly emerging and illicit substances. |
|
Al-Houqani
201212 |
Prevalence and modes of tobacco consumption |
Large cross-sectional survey |
Abu Dhabi residents |
170 430 UAE nationals aged ≥ 18 years (44% males and 56% females) |
Smoking prevalence: 24.3% males; 0.8% females
Highest prevalence reported in males (age group: 20–39 years old)
Commonest form of tobacco use:
77.4% cigarette smokers followed by
15.0% midwakh, 6.8% waterpipe, and 0.66% cigar |
Among young men –mainly UAE nationals –smoking is the most common form.
Comprehensive tobacco control laws are required in future to target young population of UAE. |
|
Al Shemmari et al, 201514 |
To examine prevalence of dokha (Arabian pipe) smoking |
Cross-sectional survey using self-administered questionnaire |
Ajman |
560 participants;
male secondary school students |
High prevalence was reported among current dokha smokers, ever dokha smokers and ever smoker
Prevalence of ever smokers: 39%
Current smokers: 24%
Ever dokha smokers: 36%
Dokha smokers: 40%
Cigarettes and shisha smokers: 30%
Students smoking dokha:
30% |
Health promotion programs are urgently needed in future, which are tailored to preventing dokha smoking as well as policies are required to further restrict the dokha availability for this age group. |
|
Crookes et al, 201415 |
Prevalence of dokha use |
Cross-sectional survey |
Five English curriculum school/ Dubai |
416 high school students |
Regular users of tobacco: daily or weekly Prevalence: 23.4% |
Timely research is further required on the emerging tobacco products. |
|
Summary of study features — Interventions/Counseling practices |
|
Awad et al,
200716 |
Addressed the delivery of smoking preventive counseling to young Arab population (9–24 years) and examined counseling behaviors and barriers to counseling |
Cross-sectional mail survey |
Emirates of Sharjah, Dubai, and Abu Dhabi |
391 eligible general practitioners (GPs) |
Percentage of GPs offering smoking preventive advices:
29% GPs provided preventive advice to pre-adolescents (9–12 years)
50% GPs provided preventive advice to adolescents (13–19 years)
65% GPs provided preventive advices to young adults (20–24 years)
Barriers to counseling included:
lack of patient educational materials;
lack of community resources;
lack of time |
Need for training and support to encourage and improve GP’s adherence to contemporary smoking prevention guidelines for counseling. |
|
Asfour et al, 201517 |
To explore
up to date information on the use of tobacco, physical activity, effectiveness of anti-tobacco media/legislation, nutrition behaviors, and gaps in health education |
Case-control study adopting Global Youth Tobacco Survey |
Abu Dhabi |
439 teenagers (Ninth grade expatriates in the UAE) |
The most concerning issues highlighted in the study were the use of dokha among expatriates |
Further intervention mainly targeting at the UAE expatriates (age group: 12–14 years old) are needed.
"Legislative efforts have not reached the younger age groups, which are most vulnerable to addiction." |
|
Khansaheb et al,
201618 |
Examined the adolescents’ self-reports regarding the health education services acquired between 2008 and 2010 |
Cross-sectional survey adapted from the Young Adult Health Care Survey |
Public high schools in Dubai |
Public high school students 730
Age group: 15–19
357 (48.9%) were males and 373 (51.1%) were females |
The results show that no health education or only little education was received by the healthcare providers. 88.2% indicated that no information was received about drug use; 94.2% indicated that no information was received about using helmet for motorbike or bicycle; 81.9% reported that they received no information about smoking
While, 79.2% reported hearing and/or seeing information with respect to substance abuse and risks of smoking |
Policy makers and health authorities in the UAE- Dubai needs to consider the national programs and guidelines related to the preventive health services targeted for adolescents. Health providers and clinicians training to deal with younger population on skills required for optimal delivery of preventive health services are needed. |
|
Awad et al,
201019 |
To address cessation counseling practices |
Cross-sectional mail survey |
Sharjah, Dubai, and Abu Dhabi |
391 eligible general practitioners |
47% of general practitioners stated that they possess adequate skills to help patients regarding tobacco cessation
24% knew about the community resources for referring patients |
Lack of knowledge and awareness can be overcome by training, support, and intervention programs. |
|
Rahman et al, 201620 |
To determine the perceptions of dental students about offering interventions pertaining to tobacco cessation |
Cross-sectional survey |
UAE |
350 students |
83.4% of students agreed that dentists should be trained to enhance their respective skills and knowledge in the adequate delivery of tobacco cessation and 56% of students disagreed that they are adequately trained to assist the patient in discontinuing the use of tobacco |
An inclusive training program and tobacco cessation education shall be included in the curriculum of dental schools across the UAE to additionally improve the confidence of students in offering services related to the tobacco cessation for smokers. |
|
Health risks from smoking |
|
Barakat-Haddad et al, 201521 |
To study the role of air quality in association with dry cough, wheeze, asthma, emphysema and chronic bronchitis among young population of UAE |
Cross-sectional survey |
Nine regions of UAE |
6363 adolescents
(Age 13–20 years) |
The significant predictors of dry cough and wheeze included ‘tobacco smoking and purposely smelling gasoline fumes, glue, correctors, car exhaust, and burning black ants’ |
The study highlighted the significance of developing educational campaigns to inform young population about the health-related threats. |
|
Jaber,
201022 |
To examine the influence of tobacco and alcohol role as possible risk factors upon the site of development of oral epithelial dysplasia |
Cross-sectional study |
Ajman |
630 oral epithelial dysplasia
patients |
Tobacco smoking plays a critical role in defining the ‘oral epithelial dysplasia subsites’ |
- |
Discussion
The studies reviewed earlier reported prevalence of smoking in the UAE. This study adds to the growing body of knowledge in the developing world, showing evidence of the hazards of tobacco use, with a focus on the association of cigarette smoking with hospitalization. Current prevalence rates of smoking in UAE from this study were estimated to range from 23.4%–24.7% in men and 0.8% in women. In Arab regions, the prevalence of smoking varies from as low as 20% in Bahrain and Egypt to high rates in Tunisia (31%) and Kuwait (34.4%).3,24,25 The prevalence in the UAE is reported to be lower than many other Middle East countries.26
Cross-sectional surveys found an alarming prevalence of the smoking among young population (mainly UAE nationals) in the UAE.12 By nationality, UAE nationals had a prevalence of 16% for midwakh use, followed by 4% for Arab expatriates and 3% for other expatriates. Among adults, the point prevalence of active cigarette smoking was < 1% in women and 24% in men, as stated by one of the largest cross-sectional surveys on adult tobacco use in the UAE.14 The smoking prevalence was consistently higher in men compared to women in other evaluated studies.12,14 Furthermore, the studies also suggested the use of dokha tobacco being the second most common type of tobacco smoked (after cigarettes) among the male UAE population specifically in Abu Dhabi.14,15 Limited published literature exists regarding midwakh use prevalence in any population with only one previously reported small cross-sectional survey of high school students in Dubai that showed 23.4% of students reported regular use of tobacco.11 This increase in the rate of tobacco use reported in a similar age group in one of the current US national data27 is similar to the prevalence in UK.28 The study also reported similar outcomes of the high acceptance of dokha among young age groups despite the different demographics of the existing sample.29 Hence, the reviewed studies demonstrate that relatively young population smoke midwakh on top of smoking at an earlier age compared to other tobacco types. Most of the young smokers favor midwakh as it can be used with different pipe styles in addition to flavored tobacco.
Although most GPs in the UAE have favorable attitudes regarding their role in counseling on smoking cessation, the actual practices fall below current recommendations.30 Consistent with the findings in other countries that showed GPs do not adhere to the counseling recommendations,31,32 a cross-sectional study reviewed suggests that half of the physicians in the UAE provide smoking assistance or preventive advice to pre-adolescents (9–12 years), 50% GPs provided preventive advice to adolescents (13–19 years), and 65% of GPs provided preventive advice to young adults (20–24 years).16 Another survey indicated that 47% of GPs had skills to help patients quit smoking, and 24% knew about the community resources to refer their patients to.19 More than half of the physicians in the study reported community resources, lack of patient educational material, and lack of time as barriers to offering smoking prevention.16 Positive results were found for warning individuals regarding the dangers of tobacco through mass media campaigns.17 Furthermore, additional efforts have to reach the younger age group, which is the most vulnerable to addiction.33–35 No research was identified highlighting the monitoring of tobacco use and prevention policies; thus, suggesting a need for research syntheses on its effectiveness. Self-help materials are considerably recommended to upsurge the motivation of the patients to quit smoking and teach them smoking cessation skills.18
Smoking and potential harms that might result from it were also reviewed. A small pre-post study with no control was led to examine the acute effects of dokha smoking. Ninety-seven volunteers, male university students (Arabs, Emiratis, and other nationalities) were consecutively sampled. The findings were comparable to those found with other smoking forms with a mean increase in the respiratory rate (4±1 breaths/min), heart rate (20±2 bpm), and systolic blood pressures (12±1 mmHg).23 Another study provided the well-known evidence linking tobacco smoking to the development of oral epithelial dysplasia.22 A cross-sectional survey conducted in nine regions of UAE also reported the impact of different risk factors on respiratory health.21 This is consistent with other international studies, where chronic bronchitis was associated with passive smoking, cigarette smoking, air pollution, and exposure to dust or gas.36,37 Regardless of the triumphs and endeavors in the tobacco control by the UAE, there remain many obstacles to achieve the goal. Such barriers may include pressure imposed by the tobacco companies and a dearth of defiance to campaigning as well as partially executing the tobacco controlling endeavors plus limited supervision concerning tobacco-related legislation.38 Keeping in mind the current regulatory frameworks39 and advancements in controlling the tobacco use by implemented taxes, it is evident that supplementary efforts can explicitly work towards the management of the current, well-organized strategies. This may include raising the minimum age to purchase tobacco to 21. Additionally, telephone-based services can help to design a stop smoking program that meets an individual need. Setting up support networks for quitting helps to decide which smoking aids should be used for cessation. Choices may include support programs, NRT, and medicines.
Conclusion
Current smoking prevalence from the studies reviewed varied widely. Even though the tobacco smoking prevalence in the UAE is less than many other Middle Eastern countries, it is a prevalent habit among young individuals and can inevitably lead to the rise in smoking-associated comorbidities. Concerted efforts and excellent accomplishment at the country level in the areas of funding, prevention and control, health education programs, and surveillance have been made to curb this increasing problem. The general population are also provided with education about the harmful effects of smoking. The previous evidence also suggest that mass media campaigns can have a significant impact on reducing the smoking initiation in the young population and adults. Increasing the price of tobacco in UAE is also well supported by the literature. Future research should be focused on evaluating the outcome and impact of current anti-smoking campaigns initiated in the UAE and to assess its integration in the comprehensive tobacco control program.
Disclosure
The authors declared no conflict of interests. No funding was received for this study.
references
- 1. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev 2013 May;(5):CD009329.
- 2. Saha SP, Bhalla DK, Whayne TF Jr, Gairola C. Cigarette smoke and adverse health effects: An overview of research trends and future needs. Int J Angiol 2007;16(3):77-83.
- 3. WHO. Tobacco; fact sheet. World Health Organization. 2018 [cited 2018 November]. Available from: http://www.who.int/mediacentre/factsheets/fs339/en/.
- 4. Apelberg BJ, Onicescu G, Avila-Tang E, Samet JM. Estimating the risks and benefits of nicotine replacement therapy for smoking cessation in the United States. Am J Public Health 2010 Feb;100(2):341-348.
- 5. Vision 2021. National key performance indicators. [Cited 2018 January 7]. Available from: https://www.vision2021.ae/en/nkpi/prevalence-smoking-any-tobacco-product.
- 6. Barth J, Critchley J, Bengel J. Psychosocial interventions for smoking cessation in patients with coronary heart disease. Cochrane Database Syst Rev 2008 Jan;(1):CD006886.
- 7. Stead LF, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev 2012 Oct;10(10):CD008286.
- 8. Snider J. Influence of health practitioners. Youth Smoking Survey. Tobacco Control Programme: Canada; 2002.
- 9. Grable JC, Ternullo S. Smoking cessation from office to bedside: an evidence-based, practical approach. 2003;114(2):45-54.
- 10. Obaid HA, Hassan MA, Mahdy NH, ElDisouky MI, Alzarba FE, Alnayeemi SR, et al. Tobacco use and associated factors among school students in Dubai, 2010: intervention study. East Mediterr Health J 2015 Feb;20(12):765-773.
- 11. Crookes A, Wolff K. Prevalence of the tobacco product dokha among high school students in Dubai. Subst Use Misuse 2014 Aug;49(10):1349-1352.
- 12. Aden B, Karrar S, Shafey O, Al Hosni F. Cigarette, water-pipe, and medwakh smoking prevalence among applicants to Abu Dhabi’s Pre-Marital Screening Program, 2011. Int J Prev Med 2013 Nov;4(11):1290-1295.
- 13. Alblooshi H, Hulse GK, El Kashef A, Al Hashmi H, Shawky M, Al Ghaferi H, et al. The pattern of substance use disorder in the United Arab Emirates in 2015: results of a National Rehabilitation Centre cohort study. Subst Abuse Treat Prev Policy 2016 May;11(1):19.
- 14. Al-Houqani M, Ali R, Hajat C. Tobacco smoking using Midwakh is an emerging health problem–evidence from a large cross-sectional survey in the United Arab Emirates. PLoS One 2012;7(6):e39189.
- 15. Al Shemmari N, Shaikh RB, Sreedharan J. Prevalence of dokha use among secondary school students in Ajman, United Arab Emirates. Asian Pac J Cancer Prev 2015;16(2):427-430.
- 16. Awad MA, O’Loughlin J. Physician delivery of smoking prevention counseling to young patients in the United Arab Emirates. Patient Educ Couns 2007 Jul;67(1-2):151-156.
- 17. Asfour LW, Stanley ZD, Weitzman M, Sherman SE. Uncovering risky behaviors of expatriate teenagers in the United Arab Emirates: A survey of tobacco use, nutrition and physical activity habits. BMC Public Health 2015 Sep;15(1):944.
- 18. Khansaheb H, Hussein A, Hamidi S, Brown D, Younis MZ. Quantitative assessment of some preventive health services provided for adolescent individuals in Dubai. J Health Hum Serv Adm 2016;39(1):95-121.
- 19. Awad MA, El Kouatly M, Fakhry R. Smoking counseling practices of physicians in the United Arab Emirates. Glob Health Promot 2010 Dec;17(4):5-14.
- 20. Rahman B, Hawas N, Rahman MM. Opinions of dental students toward tobacco cessation intervention in the United Arab Emirates. Int Dent J 2016 Oct;66(5):304-310.
- 21. Barakat-Haddad C, Zhang S, Siddiqua A, Dghaim R. Air quality and respiratory health among adolescents from the United Arab Emirates. J Environ Public Health 2015;2015:284595.
- 22. Jaber MA. Tobacco smoking and alcohol consumption as risk factors for site-specific intraoral epithelial dysplasia. J Investig Clin Dent 2010 Nov;1(2):101-107.
- 23. Shaikh RB, Abdul Haque NM, Abdul Hadi Khalil Al Mohsen H, Abdul Hadi Khalil Al Mohsen A, Haitham Khalaf Humadi M, Zaki Al Mubarak Z, et al. Acute effects of dokha smoking on the cardiovascular and respiratory systems among UAE male university students. Asian Pac J Cancer Prev 2012;13(5):1819-1822.
- 24. Sibai AM, Iskandarani M, Darzi A, Nakkash R, Saleh S, Fares S, et al. Cigarette smoking in a Middle Eastern country and its association with hospitalisation use: a nationwide cross-sectional study. BMJ Open 2016 Apr;6(4):e009881.
- 25. Memon A, Moody PM, Sugathan TN, el-Gerges N, al-Bustan M, al-Shatti A, et al. Epidemiology of smoking among Kuwaiti adults: prevalence, characteristics, and attitudes. Bull World Health Organ 2000;78(11):1306-1315.
- 26. Shafey O, Eriksen M, Ross H, Mackay J. The Tobacco Atlas. 3rd ed. American Cancer Society; 2009. p. 128.
- 27. Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the future national survey results on drug use, 1975-2017: overview, key findings on adolescent drug use. Ann Arbor Institute for Social Research, the University of Michigan; 2013.
- 28. Robinson S, Harris H. Smoking and drinking among adults, 2009: a report on the general lifestyle survey. Office for National Statistics: London. 2011 [cited 2018 August 18]. Available from: http://doc.ukdataservice.ac.uk/doc/6716/mrdoc/pdf/2009_report.pdf.
- 29. Jayakumary M, Jayadevan S, Ranade AV, Mathew E. Prevalence and pattern of dokha use among medical and allied health students in Ajman, United Arab Emirates. Asian Pac J Cancer Prev 2010;11(6):1547-1549.
- 30. Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA. 1997;278(21):1759-1766.
- 31. von Garnier C, Kochuparackal S, Miedinger D, Leuppi JD, Tamm M, Battegay E, et al. Smoking cessation advice: Swiss physicians lack training. Cancer Detect Prev 2008;32(3):209-214.
- 32. Makni H, O’Loughlin JL, Tremblay M, Gervais A, Lacroix C, Déry V, et al. Smoking prevention counseling practices of Montreal general practitioners. Arch Pediatr Adolesc Med 2002 Dec;156(12):1263-1267.
- 33. Baheiraei A, Hamzehgardeshi Z, Mohammadi MR, Nedjat S, Mohammadi E. Personal and family factors affecting life time cigarette smoking among adolescents in Tehran (Iran): a community based study. Oman Med J 2013 May;28(3):184-190.
- 34. Maruf MM, Khan MZ, Jahan N. Pattern of substance use: study in a de-addiction clinic. Oman Med J 2016 Sep;31(5):327-331.
- 35. Al-Lawati J, Mabry RM, Al-Busaidi ZQ. Tobacco control in Oman: it’s time to get serious! Oman Med J 2017 Jan;32(1):3-14.
- 36. Radon K, Büsching K, Heinrich J, Wichmann HE, Jörres RA, Magnussen H, et al. Passive smoking exposure: a risk factor for chronic bronchitis and asthma in adults? Chest 2002 Sep;122(3):1086-1090.
- 37. Sunyer J, Jarvis D, Gotschi T, Garcia-Esteban R, Jacquemin B, Aguilera I, et al. Chronic bronchitis and urban air pollution in an international study. Occup Environ Med 2006 Dec;63(12):836-843.
- 38. WHO report on the global tobacco epidemic. Enforcing bans on tobacco advertising, promotion and sponsorship. Geneva: World Health Organizaåtion. 2013 [cited 2015 June 8]. Available from: http://apps.who.int/iris/bitstream/10665/85380/1/9789241505871_eng.pdf.
- 39. Salloum RG, Abu-Rmeileh N, Hamadeh R, Thomas J, Mostafa A, Yusufali A, et al. Policy-relevant context of waterpipe tobacco smoking among university students in six countries across the Eastern Mediterranean Region: a qualitative study. Asian Pacific journal of cancer prevention. Asian Pac J Cancer Prev 2017 Sep;18(9):2533-2540.