Sarcomas account for 1% of all malignancies, while vulvar sarcomas account for 1–2% of vulvar tumors.1 Leiomyosarcoma is the most common type of sarcoma presenting in the vulva and thought to originate from the smooth muscle within erectile tissue or the blood vessel wall, or in the erectile-pili muscle. Other rare vulvar sarcomas include epithelioid sarcoma, fibrosarcoma, hemangiosarcoma, malignant hemangiopericytoma, neurogenic sarcoma, dermatofibrosarcoma protuberans, and malignant fibrous histiocytoma.2,3
Leiomyosarcomas in the Bartholin’s gland area are frequently mistaken for benign lesions, which lead to delayed diagnosis and worsen the prognosis. It usually presents in women older than 40 years of age as an insidious, slowly growing mass with hard consistency and without any significant symptoms. The identification of leiomyosarcomas in this region is particularly important due to the risk of recurrence. Patients may need radiation and/or chemotherapy in addition to adequate surgical treatment and appropriate follow-up. We report a case of vulvar leiomyosarcoma that clinically mimicked a Bartholin gland cyst.
Case report
A 63-year-old Arab woman, parity 4 (all lower uterine segment cesarean section), presented to our gynecology department with a history of painless swelling in her left labia majora lasting one year. Initially, the size of a peanut, but later she felt that it has increased in size and requested to remove it for cosmetic reasons. She was also known to have chronic renal disease and hypertension. On examination, there was no redness, on palpation at the region of left Bartholin’s gland showed a non-tender, non-fluctuant, and hard swelling measuring 3 × 4 cm. There were no palpable inguinal lymph nodes. The clinical diagnosis was a chronic left Bartholin’s gland cyst. Since the patient was asymptomatic, she was counseled about the need for conservative management only, but she insisted on surgical excision.
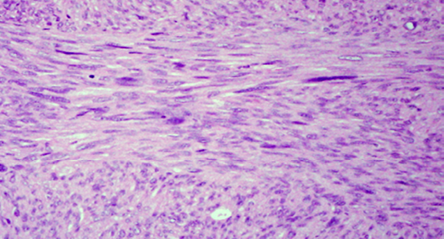
Figure 1: The tumor shows proliferation of interlacing fascicles of malignant spindle cells, magnification = 200 ×.
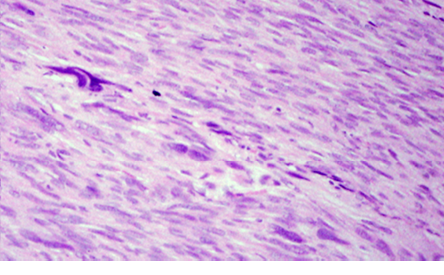
Figure 2: Leiomyosarcoma showing large bizarre hyperchromatic nuclei, magnification = 200 ×.
Complete excision of the Bartholin’s gland was done, and the mass was wholly enucleated from the bed.
On gross examination, the mass appeared as pale brown color, firm, slightly lobulated, and nodular tissue measuring 2.8 × 2.4 × 1.4 cm. Slicing revealed a pale brown colored firm surface.
The microscopic examination revealed a highly cellular tumor arranged as interlacing fascicles and sheets, composed of pleomorphic spindle to fusiform cells with elongated eosinophilic cytoplasm, variable-sized hyperchromatic ovoid to cigar-shaped nuclei and prominent nucleoli [Figure 1]. Many scattered bizarre-shaped atypical and multinucleated tumor cells were seen. Numerous mitotic figures, including atypical ones were seen (22 mitotic figures per 10 high-power field; 22MF/10 HPF); [Figure 2]. Few small foci of coagulative tumor necrosis were seen. Lymphovascular invasion was not identified. Focally the tumor was seen involving the outermost resected margin.
Immunohistochemistry of the tumor cells showed diffuse strong positive staining for smooth muscle actin, caldesmon, and desmin. The Ki-67 (MIB-1) proliferation index was around 30%. Negative staining was observed for CD117, CD4, vimentin, and S100. The histomorphological features and immunoprofile were consistent with leiomyosarcoma grade 2, according to the French Federation of Cancer Centers Sarcoma Group (FNCLCC) grading system.
The patient was referred to the Gyne-oncology department for further management. Magnetic resonance imaging revealed normal anatomy with no lymph node enlargement. She underwent a second surgery and examination under anesthesia with modified left inguinal lymphadenectomy and hemivulvectomy of the left side of the vulva, which was sent for histomor-phological evaluation.
Microscopic examination confirmed that vulvar tissue with resected margins was negative for malignancy. Eight lymph nodes showed features of reactive lymphoid hyperplasia (reactive lymphadenitis). The patient is on follow-up every six months in the oncology department.
Discussion
This is the first case of vulvar leiomyosarcoma reported in the Gulf region. The literature review revealed only nine documented cases of leiomyosarcoma located in the Bartholin’s gland.1 These cases commonly had an insidious course, presenting as enlarging painless solid mass located in the labia majora or minora. Other symptoms included pain, pruritus, and erythema. Our patient presented with a painless, slow-growing swelling in the labia majora for one year, which she wanted to remove only for cosmetic purposes.
A final diagnosis of leiomyosarcomas is usually based on histopathological examination of the excised tissue as clinically it is usually mistaken for Bartholin’s gland cyst or leiomyoma if the mass is of hard consistency. Soft tissue smooth muscle tumors with both atypia and mitotic activity are generally diagnosed as leiomyosarcomas acknowledging its potential for metastasis.4 Diagnostic criteria to differentiate between leiomyomas and leiomyosarcomas of the vulva have been suggested. Tumors exhibiting three or more of the following characteristics should be regarded as sarcoma: (1) > 5 cm in diameter, (2) infiltrative margins, (3) > 5 MF/10 HPF, and (4) moderate to severe cytological atypia. Tumors exhibiting only one of these characteristics should be diagnosed as leiomyoma, and those exhibiting two of these characteristics should be regarded as benign but atypical leiomyoma.5 Leiomyosarcoma must be considered in the differential diagnosis of other soft tissue tumors.
The histological grade represents the most important prognostic factor for all soft tissue sarcomas, and it is strongly associated with the occurence of metastasis and patients’ survival.6 The FNCLCC grading system is the best documented and tested system.6 The presence of smooth muscle actin, caldesmon, and desmin positivity confirmed the diagnosis of vulvar leiomyosarcoma in the Bartholin’s gland area.
Multiple case reports7–10 have been published in which patients with slowly growing painless vulvar masses that were initially thought to be a Bartholin’s duct cyst were found to be cancerous upon biopsy, which may delay the diagnosis and curative treatment. Due to the rarity of these tumors, there are no evidence-based diagnostic algorithms or published recommendations for treatment. However, prior reports have recommended wide local excision, hemivulvectomy, ipsilateral inguinal lymphadenectomy, chemotherapy, and radiotherapy.11,12 Decisions are made based upon the individual case presentation and pathology evaluation. Leiomyosarcomas are generally treated by complete excision with a goal of pathologic confirmation of negative margins. In our patient, based on the clinical diagnosis of chronic Bartholin’s cyst, the mass was excised.
Aartsen and Albus-Lutter13 analyzed the most extensive review of 45 patients with vulvar sarcomas comprising 25 cases of leiomyosarcoma of the vulva. They observed that leiomyosarcoma can behave aggressively with a high rate of local recurrence and can result in distant metastases by the hematogenous route to the liver and lung. However, a review of a few cases of leiomyosarcoma of the Bartholin’s
gland area did not show any distant metastases during the follow-up period, so anatomically; this location has a low risk of metastases. We had also done a bilateral inguinal lymph node biopsy in our patient, which was negative for malignancy. The patient has been under close follow-up with the oncology team for periodic evaluation to detect any local recurrence.
Conclusion
Any vulvar lesion presenting with unusual characteristics or insidious evolution in the labia majora or the Bartholin’s gland area should be carefully evaluated and treated with wide local excision. If the mass is reported as leiomyosarcoma of the Bartholin’s gland with clear resected margins and without negative prognostic factors, there is no need for radical or adjuvant treatment. Since we cannot exclude the possibility of late local recurrence, a close follow-up of these patients is essential to diagnose and treat local recurrences of the disease promptly.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Korkmaz V, Kurdoğlu Z, Karadag B, Arslanca T, Caydere M, Ergun Y. A rare case of leiomyosarcoma localized in the Bartholin’s gland area and review of the literature. J Obstet Gynaecol Res 2016 May;42(5):589-592.
- 2. Behranwala KA, Latifaj B, Blake P, Barton DP, Shepherd JH, Thomas JM. Vulvar soft tissue tumors. Int J Gynecol Cancer 2004 Jan-Feb;14(1):94-99.
- 3. González-Bugatto F, Añón-Requena MJ, López-Guerrero MA, Báez-Perea JM, Bartha JL, Hervías-Vivancos B. Vulvar leiomyosarcoma in Bartholin’s gland area: a case report and literature review. Arch Gynecol Obstet 2009 Feb;279(2):171-174.
- 4. Miettinen M. Smooth muscle tumors of soft tissue and non-uterine viscera: biology and prognosis. Modern Pathology 2014;27(1):S17-S29.
- 5. Nielsen GP, Rosenberg AE, Koerner FC, Young RH, Scully RE. Smooth-muscle tumors of the vulva. A clinicopathological study of 25 cases and review of the literature. Am J Surg Pathol 1996 Jul;20(7):779-793.
- 6. Baig MA. Evaluation of performance of various histological grading systems of soft tissue sarcomas and the prognosis (metastatic risk and survival rate). Int J Res Med Sci. 2015 Sep;3(9):2394-2401.
- 7. Mowers EL, Shank JJ, Frisch N, Reynolds RK. Myxoid leiomyosarcoma of the Bartholin gland. Obstet Gynecol 2014 Aug;124(2 Pt 2)(Suppl 1):433-435.
- 8. Dewdney S, Kennedy CM, Galask RP. Leiomyosarcoma of the vulva: a case report. J Reprod Med 2005 Aug;50(8):630-632.
- 9. Torres Lobaton A, Cruz Ortiz H, Rojo Herrera G, Avila Medrano L. Sarcomas of the vulva. Report of 2 cases. Ginecol Obstet Mex 2000;68:429-434.
- 10. Lösch A, Joura EA, Stani J, Breitenecker G, Lahodny J. Leiomyosarcoma of the vulva. A case report. J Reprod Med 2001 Jun;46(6):609-612.
- 11. Davos I, Abell MR. Soft tissue sarcomas of vulva. Gynecol Oncol 1976 Mar;4(1):70-86.
- 12. Di Gilio AR, Cormio G, Resta L, Carriero C, Loizzi V, Parisi AM, et al; DiGilioAR. Rapid growth of myxoid leiomyosarcoma of the vulva during pregnancy: a case report. Int J Gynecol Cancer 2004 Jan-Feb;14(1):172-175.
- 13. Aartsen EJ, Albus-Lutter CE. Vulvar sarcoma: clinical implications. Eur J Obstet Gynecol Reprod Biol 1994 Sep;56(3):181-189.