The growing complexity of clinical environment continues to exert increasing challenges that demand nurse educators seek innovative pedagogies to equip students with the required confidence, clinical reasoning, critical thinking skills, and competencies.1 As the millennial generation enters the nursing sector, simulation takes on a key role in effective pedagogy. Innovative pedagogies have taken momentum in shaping the nursing curriculum, and simulation has emerged as a significant method in teaching clinical courses. The literature on nursing education shows that simulation is useful in creating a strong learning environment, contributing to knowledge acquisition as well as increased awareness for safety and improved student confidence.2,3 Hence, there is an increasing trend of using simulation as a teaching strategy for imparting knowledge and competency even to novice nursing students.4
Globally, simulation is recognized in several landmark studies as an effective teaching-learning method. Although primarily used in applications in the military, nuclear power, and aviation, simulation has been integrated into the education of nurses for the last 20 years.5 As a practice-based profession, the nursing curriculum must provide opportunities for students to repeatedly practice required competencies in a conducive working environment without fear of harming patients.6 Although traditional teaching methods provide this opportunity in the nursing laboratory, they generally cannot simulate the challenges inherent in a clinical environment. Simulation as a teaching/learning method introduces the dynamism of a clinical environment and prepares students to deal with real situations.7
The emphasis on simulation is often on the application and integration of knowledge, skills, and clinical judgment. Some studies suggest that simulation has a considerable increase in knowledge,8–11 competence, self-efficacy,12 and confidence.11 Students reported increased self-confidence,13,14 self-efficacy, and satisfaction.7
Although simulation is increasingly used for teaching in developed countries, in Middle Eastern countries this has only recently started. Although simulation is increasingly appreciated and applied as a method of teaching, there are no studies evaluating the outcome of simulation in teaching novice nursing students within the context of the region. This research attempts to address that gap, adding to the existing knowledge on simulation as a teaching method in nursing in the Middle East, especially with novice nursing students, in enhancing their knowledge and competency. Some complicated procedures like injection, nasogastric tube (NGT) feeding, and urinary catheterization need concentrated practice by novice nursing students to excel in their competency. Therefore, the researchers were interested in introducing simulation among these novice nursing students taking fundamentals of nursing course. The purpose of this study was to examine the efficacy of simulation as a teaching method and compare it with case scenario for novice nursing students. The study also measured the knowledge and the role of simulation in imparting self-confidence and satisfaction among these nursing students. Hence, the research questions addressed were: what is the effectiveness of simulation in gaining knowledge and improving competency of performing NGT feeding among the novice nursing students and what is the relation between self-confidence and satisfaction among the students who underwent simulation?
Methods
In this quasi-experimental study, we assessed the knowledge and competency of 69 students registered for the Fundamentals of Nursing Laboratory course during the 2016 spring and fall (January to December) semesters at the College of Nursing, Sultan Qaboos University, Oman. The study included undergraduate direct entry students who were willing to participate and consented to the study. Ethical clearance was obtained from the College of Nursing Research and Ethics Committee.
The subjects were divided into intervention and control groups. At Sultan Qaboos University, students are admitted under different class sections: 35 students of section 20 were assigned to the intervention group and attended a simulation, while 34 students of section 10 were assigned to the control group and were given the standard case scenario used in teaching this course.
The researchers used standardized instruments to collect data. (i) Demographic Proforma - Code numbers were assigned to each student representing age, gender, cohort of study, cumulative grade point average (CGPA), and home region. (ii) Cognitive Gain Tool - A researcher-designed test was developed to measure the understanding of NGT feeding, consisting of 10 multiple-choice questions. This test was based on the current National Council Licensure Examination testing as well as the researcher’s goal of evaluating students’ abilities to recall information (as opposed to recognition). Experts reviewed the items for validity, and its reliability was 0.88. Each question had one correct answer. Hence, the minimum score was zero, and maximum score was 10. (iii) The Creighton Competency Evaluation Instrument (CCEI) - A 23-item tool used by clinical instructors to rate students on behaviors that collectively demonstrate clinical competency (assessment, communication, clinical judgment, and patient safety). This tool was used to assess students in the two settings (clinical and simulation) in previous research studies. The detailed validity and reliability statistics as reported by Hayden et al,15 which show that the overall Cronbach’s alpha coefficient ranged from 0.974 to 0.979, which is considered highly acceptable. Furthermore, the percentage of agreement between the faculty raters of the reliability and validity studies and an expert rater was 70% or higher for 20 out of 23 items.15 (iv) Student Satisfaction and Self-Confidence in Learning Scale – Developed by the National League for Nursing and used to determine novice students’ satisfaction with the simulation of the skill NGT feeding. Furthermore, this scale was used to determine students’ self-confidence in applying skills learned from the simulation to future patients. The scale consisted of 13 statements based on a 5-point Likert scale with responses ranging from ‘strongly disagree’ to ‘strongly agree’. The student satisfaction with learning scale consisted of five statements with a Cronbach’s alpha reliability of 0.94.13 The self-confidence in learning using simulations scale consisted of eight statements with Cronbach’s alpha reliability of 0.87.13 As a further measure of quality control, the content validity of both instruments was established by nine experts.13
Table 1: Chi-square values of the variables with the pre-test knowledge category.
|
Age, years |
|
|
|
|
|
|
|
≤ 20 |
33 |
97.1 |
2.862 (0.0910) |
29 |
82.9 |
0.054 (0.817) |
|
> 20 |
1 |
2.9 |
6 |
17.1 |
|
Gender |
|
|
|
|
|
|
|
Male |
7 |
20.6 |
0.200 (0.650) |
13 |
37.1 |
0.551 (0.458) |
|
Female |
27 |
79.4 |
22 |
62.9 |
|
Residence |
|
|
|
|
|
|
|
Rural |
28 |
82.4 |
0.360 (0.540) |
25 |
71.4 |
1.393 (0.238) |
|
Urban |
6 |
17.6 |
10 |
28.6 |
|
CGPA |
|
|
|
|
|
|
|
≤ 2.5 |
13 |
38.2 |
11 |
31.4 |
CGPA: cumulative grade point average.
Table 2: Comparison of mean scores and standard deviation (SD) of pre- and post-test knowledge scores between the intervention and control group.
|
Pre-test |
|
|
|
|
|
|
Intervention |
4.4 |
1.5 1.3 |
2.242 |
67 |
0.028 |
|
Control |
3.7 |
|
|
|
|
|
Post-test |
|
|
|
|
|
|
Intervention |
4.9 |
1.5 |
-0.240 |
67 |
0.810 |
df: degree of freedom.
The intervention was administered over three days. On the first day, the 69 registered students attended a two-hour theory session on the topic of human nutrition and NGT feeding, forming the basis of the intervention. On the second day in the skills laboratory session, the students’ knowledge and demographic characteristics were assessed using standardized questionnaires. This was followed by a demonstration of the NGT feeding procedure by assigned clinical instructors, who are part of the fundamentals of nursing lab course and were involved in this research.
Following the pre-test, the intervention group was given the simulation of NGT feeding procedure, and the control group was given the usual case scenario regarding NGT feeding. After this simulation practice and case scenario discussion, both groups were subjected to post-test measurements using the CCEI National League for Nursing questionnaire on self-confidence and self-satisfaction and the cognitive gain tool. The pre- and post-test data were collected by four trained nursing faculty who were involved in teaching the course, and only two were part of the study.
Table 3: t-test and comparison of mean scores and standard deviation (SD) of post-test competency between the intervention and control group.
|
Post-test |
|
|
|
|
|
|
Intervention |
14.6 |
0.98 |
3.869 |
67 |
< 0.001* |
df: degree of freedom.
Results
Data were analyzed using SPSS Statistics (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). In both the control and intervention group, the majority of students were ≤ 20 years old, females, hailed from rural areas, and had a CGPA of > 2.5 [Table 1]. The data did not show any statistically significant association between the pre-test categories and the selected variables (p > 0.050), implying a homogenous sample in both groups before the study.
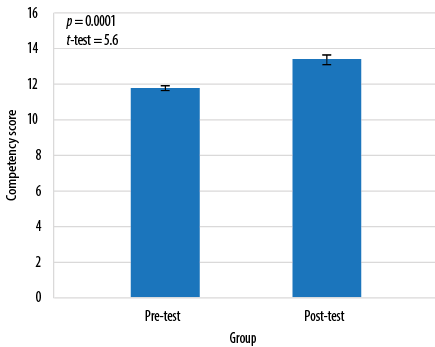
Figure 1: Competency scores of the control group before and after case scenario.
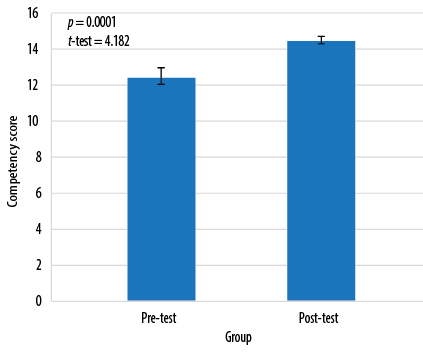
Figure 2: Competency scores of the intervention group before and after simulation.
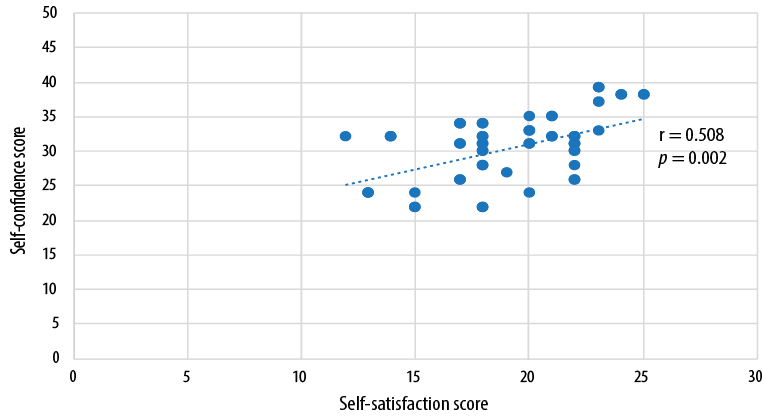
Figure 3: Correlation between self-confidence and self-satisfaction score in the intervention group.
There was no significant difference in the mean scores of knowledge between groups before and after the intervention, or between the groups, showing that the knowledge scores were independent of the intervention [Table 2]. Data showed a significant improvement in the mean competency scores indicating that both simulation and case scenario were effective in improving student competencies (p < 0.001) [Figure 1 and 2]. The t-test computed between the post-test scores of competency between the intervention and the control group showed a statistically significant difference in the mean scores between the two teaching methods (t (67) = 3.869, p < 0.001), suggesting that simulation was better in improving the competency than case scenario [Table 3]. The results shown in Figure 3 indicate a positive statistical significance between satisfaction and self-confidence. Students who were satisfied had better self-confidence in performing the procedure in the intervention group.
Table 2 compares pre- and post-test in terms of participants’ knowledge. The data shows no significant difference in the knowledge mean scores between groups before and after the intervention.
We observed a significant improvement in the mean post-test scores in competency for the control group following the case scenario [Figure 1]. This was also the case for the intervention group [Figure 2].
We found a positive statistical significance between satisfaction and self-confidence [Figure 3]. We found a significant difference in the mean competency scores between the control and intervention group [Table 3]. Hence, it was inferred that simulation was effective in improving the competency of the students compared with case scenario in performing NGT feeding.
Discussion
Advanced technology accessible for the millennial generation of nursing students has created opportunities for nurse educators to use simulation as a teaching strategy. This study was a preliminary investigation into the efficacy of simulation as a best practice among novice nursing students compared to the case scenario method. The current study provides empirical data of simulation-based nursing education with first-year nursing students with respect to knowledge, competency, satisfaction, and self-confidence. The results reveal that both case scenarios and simulation-based learning had a positive impact on improving the knowledge and competency of novice nursing students. However, there was a statistically significant difference in the mean post-test scores of competency, leading to the conclusion that simulation was better than the case scenario. Similarities between the current study and previous findings16,17 are evident. Other studies have reported satisfaction with learning and level of self-confidence,17,18 as well as improved communication and clinical reasoning with simulation and the use of standardized patients as teaching strategies for undergraduate nursing students.7
Students who were satisfied with the simulation learning perceived higher levels of competency to perform the requisite nursing skills. This is similar to the findings of other recent, similar studies, which revealed a positive association between simulation, satisfaction, and self-confidence.3,19,20
Available literature in simulation and nursing education provides evidence on improved learning outcomes of nursing students in various aspects including knowledge, competency, clinical reasoning, communication, teamwork, and patient safety.3,7,21–26 This study is the first to evaluate the effectiveness of simulation-based learning among novice nursing students in the Middle East, a vast region spanning 12 countries with over 218 million people. In evaluating research, the results need to be carefully weighed based on the cost-effectiveness of the two teaching strategies. It can be concluded that simulation as a best practice could be utilized in first level nursing courses because students exposed to this method report a higher perception of satisfaction and self-confidence. However, questions remain as to whether a simulated learning environment would help novice nursing students retain and transfer the learning outcomes in actual clinical settings. Further research is needed to evaluate the knowledge, student performance, satisfaction, and self-confidence in the clinical setting after simulated learning experiences.
Our study was limited by its small sample size, as the estimated sample size of 80 was not available within the study period of spring and fall 2016. Hence, the results are limited to the participants of the study. Another limitation is the inter-observer error/difference in the assessment of competency with four observers. These limitations may affect the generalizability of the findings to other populations and clinical settings.
Based on our findings, we recommend the following:
1. Conducting a comparative cross-sectional study to evaluate simulation effectiveness across different courses. 2. Assessing the follow-up of clinical skills competency. 3. Conducting similar studies with other complex nursing procedures (e.g., wound dressing and medication administration).
Conclusion
This study has various implications for nursing education, practice, and research. Simulation is a very effective tool for teaching practical skills. However, we found a statistically significant difference between the two methods of teaching. This helped us to conclude that competency gained by novice students’ learning a skill through simulation, was better than the competency gained through case scenario. However, simulation can be used for teaching vital skills to the students (especially novices) in a safe environment without the fear of making mistakes. Curriculum planners could dedicate 5–10% of clinical experience to simulation in level one and two courses.
Disclosure
The authors declared no conflicts of interest. The study was supported by the Dean’s Fund for Research, College of Nursing, Sultan Qaboos University, Muscat, Oman.
references
- 1. Kalman M. Teaching students’ practical skills: the clinical project as a culminating experience. Clin Nurse Spec 2008 Mar;22(2):103.
- 2. Kaddoura M, Vandyke O, Smallwood C, Gonzalez KM. Perceived benefits and challenges of repeated exposure to high fidelity simulation experiences of first degree accelerated bachelor nursing students. Nurse Educ Today 2016 Jan;36:298-303.
- 3. Norman J. Systematic review of the literature on simulation in nursing education. ABNF J 2012;23(2):24-28.
- 4. Tuoriniemi P, Schott-Baer D. Implementing a high-fidelity simulation program in a community college setting. Nurs Educ Perspect 2008 Mar-Apr;29(2):105-109.
- 5. Aebersold M, Tschannen D. Simulation in nursing practice: the impact on patient care. Online J Issues Nurs 2013 May;18(2):6.
- 6. Park HR, Park JW, Kim CJ, Song JE. Development and validation of simulation teaching strategies in an integrated nursing practicum. Collegian 2017 Oct;24(5):479-486.
- 7. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect 2009 Mar-Apr;30(2):79-82.
- 8. Gates MG, Parr MB, Hughen JE. Enhancing nursing knowledge using high-fidelity simulation. J Nurs Educ 2012 Jan;51(1):9-15.
- 9. Howard VM, Ross C, Mitchell AM, Nelson GM. Human patient simulators and interactive case studies: A comparative analysis of learning outcomes and student perceptions. CIN: Computers, Informatics. Nursing 2010;28(1):42-48.
- 10. Lapkin S, Fernandez R, Levett-Jones T, Bellchambers H. The effectiveness of using human patient simulation manikins in the teaching of clinical reasoning skills to undergraduate nursing students: a systematic review. JBI Libr Syst Rev 2010;8(16):661-694.
- 11. Tiffen J, Corbridge S, Shen BC, Robinson P. Patient simulator for teaching heart and lung assessment skills to advanced practice nursing students. Clin Simul Nurs 2011 May;7(3):e91-e97.
- 12. Kameg K, Howard VM, Clochesy J, Mitchell AM, Suresky JM. The impact of high fidelity human simulation on self-efficacy of communication skills. Issues Ment Health Nurs 2010 May;31(5):315-323.
- 13. Jeffries PR, Rizzolo MA. Designing and Implementing Models for the Innovative Use of Simulation to Teach Nursing Care of Ill Adults and Children: A National, Multi-Site, Multi-Method Study [Summary Report]. 2016 [cited 2018 September]. Available from: http://www.nln.org/docs/default-source/professional-development-programs/read-the-nln-laerdal-project-summary-report-pdf.pdf?sfvrsn=0.
- 14. Kaddoura MA. New graduate nurses’ perceptions of the effects of clinical simulation on their critical thinking, learning, and confidence. J Contin Educ Nurs 2010 Nov;41(11):506-516.
- 15. Hayden J, Keegan M, Kardong-Edgren S, Smiley RA. Reliability and validity testing of the Creighton Competency Evaluation Instrument for use in the NCSBN National Simulation Study. Nurs Educ Perspect 2014 Jul-Aug;35(4):244-252.
- 16. Mills J, West C, Langtree T, Usher K, Henry R, Chamberlain-Salaun J, et al. ‘Putting it together’: unfolding case studies and high-fidelity simulation in the first-year of an undergraduate nursing curriculum. Nurse Educ Pract 2014 Jan;14(1):12-17.
- 17. Yuan HB, Williams BA, Fang JB. The contribution of high fidelity simulation to nursing students’ confidence and competence: a systematic review. Int Nurs Rev 2012 Mar;59(1):26-33.
- 18. Robinson-Smith G, Bradley PK, Meakim C. Evaluating the use of standardized patients in undergraduate psychiatric nursing experiences. Clin Simul Nurs 2009 Nov;5(6):e203-e211.
- 19. Natarajan J, Al-Khasawneh EA, Bartlett JL. Simulation in nursing education: faculty and prelicensure bsn student perspectives ‒ an integrated review. International Educational Scientific Research Journal 2016 Jun;2(6):89-95.
- 20. Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ 2016 May;16(1):152.
- 21. Gore T, Thomson W. Use of simulation in undergraduate and graduate education. AACN Adv Crit Care 2016 Feb;27(1):86-95.
- 22. O’Connor T. The role of simulation in nursing education. Nurs N Z 2014 Feb;20(1):11-12.
- 23. Richardson KJ, Claman F. High-fidelity simulation in nursing education: a change in clinical practice. Nurs Educ Perspect 2014 Mar-Apr;35(2):125-127.
- 24. Weaver A. High-fidelity patient simulation in nursing education: an integrative review. Nurs Educ Perspect 2011 Jan-Feb;32(1):37-40.
- 25. Al Sabei SD, Lasater K. Simulation debriefing for clinical judgment development: A concept analysis. Nurse Educ Today 2016 Oct;45:42-47.
- 26. Madhavanprabhakaran G, Al-Khasawneh E, Wittmann L. Perceived benefits of pre-clinical simulation-based training on clinical learning outcomes among Omani undergraduate nursing students. Sultan Qaboos Univ Med J 2015 Feb;15(1):e105-e111.