Interventional radiology (IR) is a minimally invasive procedure that involves use of various radiological techniques, including X-ray fluoroscopy, ultrasonography, computed tomography (CT), and magnetic resonance imaging, as specifically targeted therapy.1 Diagnostic radiology includes a variety of subspecialties, including neuroradiology, pediatric radiology, nuclear radiology, hospice and palliative medicine, pain medicine, and vascular and IR.2 In 2012, IR was recognized as a specialty by the American Board of Medical Specialties, and a residency program was started.3 The practice of IR includes embolization, angioplasty, stent insertion, drainage, ablation, and treatment of thrombus, among many other therapeutic interventions.2 The role of IR in the management of a number of conditions has expanded in the last few years to include a variety of organ systems.4,5 However, these expanded indications for IR have been accompanied by an increase in demand, complexity, and lack of manpower.6,7 Despite some medical schools in the US exposing students to IR, only 5.5% participated in elective rotations, and among those students, only 12.5% were interested in IR as a specialty.8 The degree of awareness and knowledge of IR is still relatively low in general, especially among students in their preclinical years because radiology rotations do not start until the clinical years.9–12 Moreover, we were only able to identify one study in Saudi Arabia that assessed medical students’ awareness and knowledge of IR.12 That study was performed at King Khalid University and concluded that medical students and interns have poor education about this specialty.12
We believe that there is a need for ongoing research on this issue, particularly in Saudi Arabia, where relevant data are extremely scarce. Our study sought to assess the awareness of IR as a specialty among medical students and determine if there is a difference between the clerkship and pre-clerkship years.
Methods
Our institutional review board approved this cross-sectional, questionnaire-based study, and informed consent was obtained from the participants. A self-administered questionnaire was distributed to male and female undergraduate medical students in their second to sixth year during February 2018. The radiology curriculum is integrated into each module that students complete during their years in college; in addition, fourth-year medical students complete a focused two-week radiology course credited as three hours to the students’ grade point average. Medical students at our institution can obtain clinical and observational training during their clinical years. The survey was sent to 1127 students, 542 (48.1%) of whom returned a completed questionnaire answering all questions. The same questionnaire has been used in previous studies.10
The questionnaire consisted of 17 items in several categories, including awareness of IR procedures, training route, and hospital duties. The respondents were asked to compare their level of knowledge about IR with that on other specialties, their level of interest in IR, and their desire for future education on this subject. The study participants were asked to recall how they gained information about IR and to rank their favored methods for learning about IR in the future. They were also asked whether they would be interested in taking part in obligatory rotations in the field of radiology along with a two-week elective in IR during the clerkship curriculum.
Table 1: Response rate and respondents’ knowledge and interest in diagnostic and interventional radiology (IR).
|
Self-reported knowledge of IR as compared with other subjects |
Excellent |
18 |
3.3 |
|
Good |
73 |
13.5 |
|
Adequate |
167 |
30.8 |
|
Poor |
199 |
36.7 |
|
No knowledge |
85 |
15.7 |
|
Completed or plan to complete an elective in radiology |
Yes |
136 |
25.1 |
|
No |
406 |
74.9 |
|
Respondents who would consider a career in radiology |
Yes |
87 |
16.1 |
|
No |
247 |
45.6 |
|
Not sure |
208 |
38.4 |
|
Respondents who would consider a career in IR |
Yes |
78 |
14.4 |
|
No |
218 |
40.2 |
|
Not sure |
246 |
45.4 |
|
Reasons respondents would not consider a career in IR or are not sure |
Lack of knowledge |
199/464 |
42.9 |
|
Lack of interest |
169/464 |
36.4 |
|
Lifestyle |
53/464 |
11.4 |
|
Radiation exposure |
43/464 |
9.3 |
|
Yes |
128 |
23.6 |
|
No |
342 |
63.1 |
Categorical variables, including primary variables, were summarized in a frequency table. Continuous variables that were normally distributed are given as the mean, standard deviation, and range. The data were compared for statistical significance using the chi-square test. The statistical analysis was performed using SPSS Statistics (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.). A p-value < 0.050 was considered statistically significant.
Results
The survey was sent to 1127 students, 542 (48.1%) of whom returned a completed questionnaire. Of 542 participants enrolled in the study, 123 (22.7%) were in their second year, 143 (26.4%) were in their third year, 64 (11.8%) were in their fourth year, 103 (19.0%) were in their fifth year, and 109 (20.1%) were in their sixth (final) year. Two hundred and seventy-six (50.9%) of the respondents were in the clerkship years, and 266 (49.1%) were in the pre-clerkship years.
Only 136 (25.1%) students had completed or were planning to take an elective in radiology, 87 (16.1%) said they would consider a career in diagnostic radiology, and 78 (14.4%) said they would consider a career in IR [Table 1]. One hundred and ninety-nine respondents (36.7%) rated their knowledge of IR as ‘poor,’ and 85 (15.7%) reported that they had ‘no knowledge’ of IR. One hundred and twenty-eight (23.6%) of the students reported having seen patients who were treated by an interventional radiologist.
Table 2: Association between demographic characteristics of the sample and knowledge of interventional radiology (IR) and year of undergraduate study.
|
Interest in diagnostic radiology |
57 (65.5) |
30 (34.5) |
0.004 |
30 (34.5) |
57 (65.5) |
< 0.001 |
87 |
|
Interest in IR |
57 (73.1) |
21 (26.9) |
< 0.001 |
30 (38.5) |
48 (61.5) |
0.010 |
78 |
|
Did an elective in radiology |
73 (53.7) |
63 (46.3) |
0.520 |
55 (40.4) |
81 (59.6) |
0.002 |
136 |
|
Exposure to IR |
151 (55.7) |
120 (44.3) |
0.030 |
103 (38.0) |
168 (62.0) |
< 0.001 |
271 |
|
Residency of IR doctors* |
132 (58.9) |
92 (41.1) |
0.002 |
120 (53.6) |
104 (46.4) |
0.710 |
224 |
|
Academic level |
|
|
|
|
|
0.080 |
|
|
Pre-clerkship |
- |
- |
|
150 (56.4) |
116 (43.6) |
|
266 |
Values are presented as n (%). *Students who correctly identified that interventional radiologists must finish a residency training program in radiology only.
The most common reasons given for not wanting to choose or being uncertain about a career in IR were lack of knowledge (n = 199, 42.8%) and lack of interest (n = 169, 36.4%; Table 1).
When asked to “list three IR procedures that you know of”, the most commonly mentioned procedures were image-guided biopsies (n = 103, 19.0%) and embolization (n = 72, 13.3%). Forty-nine (9.0%) of the students could not name one IR procedure and 58.7% mentioned non-IR procedures.
Two hundred and twenty-four (41.3%) of the 542 students correctly identified that interventional radiologists must finish a residency training program in radiology [Figure 1].
Table 3: Gender differences among the demographic characteristics of the sample.
|
Knowledge of IR |
|
|
0.912 |
|
|
Poor/No knowledge |
140 (49.3) |
144 (50.7) |
|
284 |
|
Excellent/Good/Adequate knowledge |
125 (48.4) |
133 (51.6) |
|
258 |
|
Interest in diagnostic radiology |
47 (54.0) |
40 (46.0) |
0.354 |
87 |
|
Interest in IR |
39 (50.0) |
39 (50.0) |
0.929 |
78 |
|
Did an elective in radiology |
64 (47.1) |
72 (52.9) |
0.693 |
136 |
IR: interventional radiology.
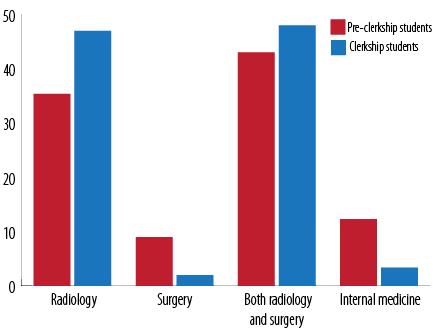
Figure 1: Answers related to the suggestion of a residency program for interventional radiology.
The proportions of clerkship students who were interested in diagnostic radiology and IR were greater than those of pre-clerkship students (65.5%, p = 0.004 and 73.1%, p < 0.001, respectively). Furthermore, an interest in diagnostic radiology and IR was significantly more common among those who rated their knowledge as excellent/good/adequate (65.5%, p < 0.001 and 61.5%, p = 0.010, respectively). Details of the association between demographic characteristics, year of study, and knowledge about IR are presented in Table 2.
Gender differences among the demographic characteristics of the sample are shown in Table 3.
When the respondents were asked about the clinical duties of an interventional radiologist, only 233 (43.0%) thought that they hold outpatient clinics, 266 (49.1%) thought that they attended ward rounds, and 308 (56.8%) thought that they have admitting privileges.
When asked about their source of information on IR, the most common answer was lectures from interventional radiologists (n = 83, 15.3%). Other sources are shown in Table 4. Half the respondents (n = 271, 50.0%) had no exposure to IR.
Ward rounds, electives in the radiology department, and lectures about IR were reported to be the preferred methods for learning about IR (97, 73, and 48 students, respectively). Two hundred and five respondents (37.8%) ranked a medical research project as the worst method for learning about IR [Table 5].
Table 4: Sources that provided participants with the most information about interventional radiology (IR).
|
Radiology elective |
53 |
9.8 |
|
Lectures from IR doctors |
83 |
15.3 |
|
Ward rounds in hospital |
27 |
5.0 |
|
Self-directed research |
54 |
10.0 |
|
Problem-based learning tutorials |
35 |
6.5 |
|
Multidisciplinary meetings |
19 |
3.5 |
Table 5: Favored methods for learning about interventional radiology (IR).
|
Ward rounds |
167 |
86 |
73 |
57 |
47 |
55 |
57 |
|
Radiology department electives |
123 |
164 |
85 |
55 |
46 |
41 |
28 |
|
Lectures from IR doctors |
108 |
94 |
136 |
72 |
65 |
26 |
41 |
|
Multidisciplinary meetings |
32 |
52 |
87 |
166 |
82 |
62 |
61 |
|
Self-directed learning websites |
47 |
49 |
63 |
64 |
145 |
89 |
85 |
|
PBL tutorials |
31 |
58 |
62 |
76 |
79 |
171 |
65 |
Data given as numbers: 1 = best to 7 = worst. PBL: problem-based learning.
Three hundred and sixteen respondents (58.3%) thought that a two-week mandatory radiology rotation during medical school would be beneficial, and 333 (61.4%) stated that they would be interested in doing a two-week IR elective during the surgery curriculum at medical school.
Discussion
IR is an emerging and expanding specialty that has a role in many health care disciplines and services, particularly oncology, cardiovascular medicine, trauma, and urology.13 IR also has many clinical applications and better outcomes, and the procedures performed are minimally invasive and less complicated than routine surgery. Interestingly, it has been reported that new IR procedures are being developed at a rate of 3.5% annually and that an estimated US$108.3 million could be saved each year if just eight surgical procedures were replaced by IR procedures.14 However, the harsh reality is that IR is suffering from an increasing shortage in manpower that is impeding the expansion and use of IR procedures, and very small numbers of qualified interventional radiologists are presently serving very large populations. According to the 2016 Clinical Radiology UK Workforce consensus report, growth in the radiology workforce is not keeping up with the demands made on radiology services.15 The low recruitment rate can be explained by a lack of knowledge and understanding of IR on the part of undergraduate medical students, who are our future doctors.16
To the best of our knowledge, there is very limited literature on medical students’ knowledge about IR as a specialty in our region. This lack of knowledge may be preventing their attention becoming focused on IR and may also be promoting a perception of IR as a minor specialty. The most common misconceptions about radiology as a specialty are that the radiologist’s only task is to read films and that there is no interaction with patients. These misconceptions would severely impact the choice of radiology or IR as a career option. Our findings are consistent with those of a study conducted in the US that identified the important reasons for not entering a radiological specialty were lack of patient contact, the work environment, and the degree of impact on patient care.17
The level of interest in radiology and IR could be improved significantly by increasing students’ knowledge about this specialty. In our study, the awareness rate was higher in those who were interested in radiology (p < 0.001) and IR specifically (p = 0.010) than in those who were not interested in the specialty, which is not surprising because knowledge leads to a better understanding of the specialty and in turn to an informed career decision. Even students who had not considered IR as a career could refer patients to IR clinics in the future. Similarly, students who carried out an elective in radiology had more knowledge of IR (p = 0.002).
Over one third (36.7%) of students in this study rated their knowledge of IR as poor or non-existent, which indicates an insufficient awareness of this specialty. Another study conducted in Saudi Arabia similarly found that 52% of students had a poor knowledge of IR.12 These local findings are consistent with those of a study performed in Ireland in which 62% of medical students had a poor knowledge of IR,18 as did those in studies conducted in England9 and Canada,10 in which 55.5% and 52% of students, respectively, knew little about IR as a specialty. Furthermore, 67.7% of the respondents in our study could not name a single IR procedure or incorrectly named non-IR procedures, which is attributed to both lack of knowledge and a wrong impression of IR as a specialty. The finding that cardiologists and vascular surgeons were the main sources of information about IR procedures for medical students is disappointing, particularly so given that only 1.3% of the respondents correctly identified embolization as an IR procedure. Cardiology and vascular surgery are well covered in the medical education curriculum, and students are well exposed to these two specialties during lectures and their clerkship years.19,20 Moreover, most students were unaware of the privileges enjoyed by interventional radiologists such as doing ward rounds, having an outpatient clinic, and admission privileges. Other studies have also addressed the issue of lack of knowledge and exposure as causes for poor awareness of IR as a specialty.10,11,21 Undergraduate medical students are the main reservoir for the recruitment of new interventional radiologists. However, most of these students have poor knowledge of IR; in our opinion, this is the main cause of increasingly poor recruitment rates.9,18 Therefore, reinforcing awareness and knowledge of IR among medical students is essential.
We found that students who had already undertaken or were planning to undertake an elective in IR tended to be more informed about this specialty (59.6%, p = 0.002) than those who had never had an elective in IR and had no plans to take one. This finding underscores the importance of electives as tools for improving medical students’ understanding and recognition of IR as an emerging and essential specialty area, not only to increase the number of new IR physicians in the field, but also to make them better physicians regardless of the specialty that they are planning to pursue and aware they can refer patients to IR clinics.
Therefore, increasing medical students’ knowledge of IR is mandatory. In our study, we found that students in the clerkship years were significantly more interested in diagnostic radiology (p = 0.004). Similarly, students in the clerkship years were more likely to be interested in IR than their counterparts in the pre-clerkship years (73.1% vs. 26.9%, p < 0.001). Including more compulsory radiology rotations in the curriculum rather than just a short rotation or an optional elective could have an impact on students’ knowledge and interest in IR, especially for pre-clerkship students, given our finding that the exposure to IR was significant only for clerkship students (p = 0.030). This result is consistent with a US report showing that preclinical students were more likely to have poor knowledge of IR than clinical students (49% vs. 16.7%).11 Similarly, a study in Ireland found that students’ knowledge about IR increased from 4% to 42% after 10 hours of lectures on the subject.21 Exposing pre-clerkship students to radiology increases their interest in IR as a career and appreciation of the specialty.22 This could be achieved in several ways, including dedicated lectures on IR, an integrated system of learning for pre-clerkship students, mandatory rotations, electives, attending procedures, IR physicians serving as mentors, and interventional radiologists themselves being a source of information about IR rather than vascular surgeons or cardiologists.
There is insufficient involvement of interventional radiologists in our undergraduate medical curriculum. In this study, 61.4% of respondents agreed that it would be beneficial to include a mandatory two-week IR rotation as part of the surgery curriculum at medical school, even though not all of them were considering radiology as a career after graduation. This finding is similar to that of a Canadian study in which nearly 71% of students agreed with the suggestion of a mandatory two-week IR rotation.10 Medical students who have a mandatory radiological rotation would be better informed about IR as a specialty than those who do not.11
There is now a pressing need to close the gap between supply and demand in radiological services (especially IR) by attracting more students to explore the future of this specialty and the rewards of entering it or at least increase their awareness of it for future collaboration with other specialties, especially the surgical ones.
This study has some unavoidable limitations that should be taken into account when interpreting its results. First, the study participants were enrolled from one Saudi university and may not be representative of all students in the country. A study that addresses the issue of undergraduate awareness of IR at a national level is needed in the future. It is noteworthy that the sample size in this study (542 students) is larger than that in the previous studies reported in the literature;9,10,12,18 the largest of these was a UK study, which contained 220 students.9 Second, the study had a survey-based design, which may have introduced a degree response bias, given that subjects who are interested in the topic may be more likely to complete a questionnaire. However, our response rate of 48.1% is higher than similar studies performed in Canada (19%), Saudi Arabia (35.3%), and Europe (34.5%).10,12,18 Nevertheless, it is possible that there are some hitherto unidentified factors that caused the relatively low response rates in both our study and the studies performed by other researchers, such as a basic lack of interest in the topic. Even though this research was limited to one medical school, we were able to identify that there is no well-defined IR curriculum in any of the medical schools in Saudi Arabia.
Conclusion
Medical students’ awareness and exposure to IR in the undergraduate curriculum is inadequate. This could influence a student’s decision regarding IR as a career. This issue can only be resolved by a direct contribution from interventional radiologists to an undergraduate radiology curriculum. There are several methods that might be used to introduce medical students to IR, including dedicated lectures, an integrated learning system for pre-clerkship students, IR physicians serving as mentors, mandatory rotations, and electives. The lack of a unified radiology curriculum in medical schools across the country should be addressed by the Council of Deans of Saudi Medical Schools. Involvement of the Saudi Interventional Radiology Society and the Radiological Society of Saudi Arabia will be essential when addressing this issue.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Kessel D. What is Interventional Radiology? British Society of Interventional Radiology (BSIR). 2013 [cited 2017 Nov 5]. Available from: https://www.bsir.org/patients/what-is-interventional-radiology/.
- 2. American Board of Radiology. American Board of Medical Specialties [cited 2017 Nov 10]. Available from: http://www.abms.org/member-boards/contact-an-abms-member-board/american-board-of-radiology/.
- 3. Kattapuram TM, Sheth RA, Ganguli S, Mueller PR, Walker TG. Interventional radiology symposium for medical students: saising awareness, understanding, and interest. J Am Coll Radiol 2015 Sep;12(9):968-971.
- 4. Baker TA, Aaron JM, Borge M, Pierce K, Shoup M, Aranha GV. Role of interventional radiology in the management of complications after pancreaticoduodenectomy. Am J Surg 2008 Mar;195(3):386-390, discussion 390.
- 5. Belli AM, Markose G, Morgan R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Intervent Radiol 2012 Apr;35(2):234-243.
- 6. Sunshine JH, Cypel YS, Schepps B. Diagnostic radiologists in 2000: basic characteristics, practices, and issues related to the radiologist shortage. AJR Am J Roentgenol 2002 Feb;178(2):291-301.
- 7. Adam A. The 2006 Charles T. Dotter lecture: interventional radiology–veni, vidi, vanished? J Vasc Interv Radiol 2006 Sep;17(9):1399-1403.
- 8. Nissim L, Krupinski E, Hunter T, Taljanovic M. Exposure to, understanding of, and interest in interventional radiology in American medical students. Acad Radiol 2013 Apr;20(4):493-499.
- 9. Atiiga PA, Drozd M, Veettil R. Awareness, knowledge, and interest in interventional radiology among final year medical students in England. Clin Radiol 2017 Sep;72(9):795.e7-795.e12.
- 10. O’Malley L, Athreya S. Awareness and level of knowledge of interventional radiology among medical students at a Canadian institution. Acad Radiol 2012 Jul;19(7):894-901.
- 11. Commander CW, Pabon-Ramos WM, Isaacson AJ, Yu H, Burke CT, Dixon RG. Assessing medical students’ knowledge of IR at two American Medical schools. J Vasc Interv Radiol. 2014;25(11):1801-1806, 1807.e1-e5.
- 12. Alshumrani GA. Awareness of interventional radiology among final-year medical students and medical interns at a university in Southwestern Saudi Arabia. Saudi Med J 2013 Aug;34(8):841-847.
- 13. Investing in the clinical radiology workforce – the quality and efficiency case. The Royal College of Radiologists. 2012 [cited 2018 Sept 8]. Available from: https://www.rcr.ac.uk/publication/investing-interventional-radiology-workforce-quality-and-efficiency-case.
- 14. Baerlocher MO. Canada’s slow adoption of new technologies adds burden to health care system. CMAJ 2007 Feb;176(5):616.
- 15. Clinical radiology UK workforce census 2016 report. The Royal College of Radiologists. 2017 [cited 2018 Sept 28]. Available from: https://www.rcr.ac.uk/publication/clinical-radiology-uk-workforce-census-2016-report.
- 16. Sunshine JH, Cypel YS, Schepps B. Diagnostic radiologists in 2000: basic characteristics, practices, and issues related to the radiologist shortage. AJR Am J Roentgenol 2002 Feb;178(2):291-301.
- 17. Arleo EK, Bluth E, Francavilla M, Straus CM, Reddy S, Recht M. Surveying fourth-year medical students regarding the choice of diagnostic radiology as a specialty. J Am Coll Radiol 2016 Feb;13(2):188-195.
- 18. Leong S, Keeling AN, Lee MJ. A survey of interventional radiology awareness among final-year medical students in a European country. Cardiovasc Intervent Radiol 2009 Jul;32(4):623-629.
- 19. Levin DC, Abrams HL, Castaneda-Zuñiga WR, Fellows KE, Grollman J Jr, Mitchell WA, et al. Lessons from history. Why radiologists lost coronary angiography and what can be done to prevent future similar losses. Invest Radiol 1994 Apr;29(4):480-484.
- 20. Veith FJ, Gargiulo NJ. Endovascular aortic repair should be the gold standard for ruptured AAAs, and all vascular surgeons should be prepared to perform them. Perspect Vasc Surg Endovasc Ther 2007 Sep;19(3):275-282.
- 21. Shaikh M, Shaygi B, Asadi H, Thanaratnam P, Pennycooke K, Mirza M, et al. The introduction of an undergraduate interventional radiology (IR) curriculum: impact on medical student knowledge and interest in IR. Cardiovasc Intervent Radiol 2016 Apr;39(4):514-521.
- 22. Branstetter BF IV, Faix LE, Humphrey AL, Schumann JB. Preclinical medical student training in radiology: the effect of early exposure. AJR Am J Roentgenol 2007 Jan;188(1):W9-W14.