Compared to arterial aneurysms, venous aneurysms are rare clinical entity.1–12 They have been reported in cervical, thoracic, visceral, and extremity regions. Isolated venous aneurysm of the neck is an uncommon clinical anomaly because of the low pressure in the superior vena caval reservoir system.
Venous aneurysms can be seen in several anatomic locations in the neck. External jugular vein aneurysms are less frequent than internal jugular vein aneurysms, but the anterior jugular vein aneurysms are the least frequent.1–9 Although multidetector computed tomography (CT) angiography or selective venography can be helpful in the diagnosis, ultrasound (US) with color Doppler imaging is the gold standard for the diagnosis of such aneurysms.1,3,6,8,9,12,13
In this report, we describe a 45-year-old woman with external jugular vein aneurysm and its clinical and radiological characteristics.

Figure 1: A 45-year-old woman with a lump in the left supraclavicular region, which had been present for a few months.
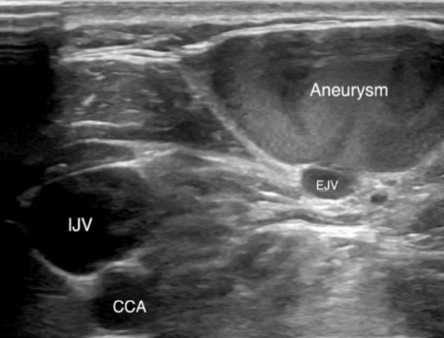
IJV: internal jugular vein; EJV: external jugular vein; CCA: common carotid artery.
Figure 2: Grayscale ultrasound image of an external jugular vein aneurysm. Ultrasound showed the presence of a cystic mass communicating with a short neck with the external jugular vein.
Case report
A 45-year-old woman was referred to our US department with a mass in the left supraclavicular region, which had been increasing gradually in size with time. There was no history of difficulty in swallowing, change in her voice, or any nasal symptoms. The patient denied any history of trauma or medical intervention in this area.
Physical examination revealed a soft, non-tender, non-pulsatile, and fluctuant swelling at the lateral border of the lower part of the left sternocleidomastoid muscle, in the transition of the IV and V level of the left neck [Figure 1]. The skin overlying the mass showed no signs of inflammation, discoloration, or thickening. The mass was slightly enlarging with Valsalva maneuver. The swelling was compressible. No bruit was heard on auscultation over the swelling. No other palpable masses were detected in the rest of the neck. Chest, abdomen examination, and blood tests were unremarkable.
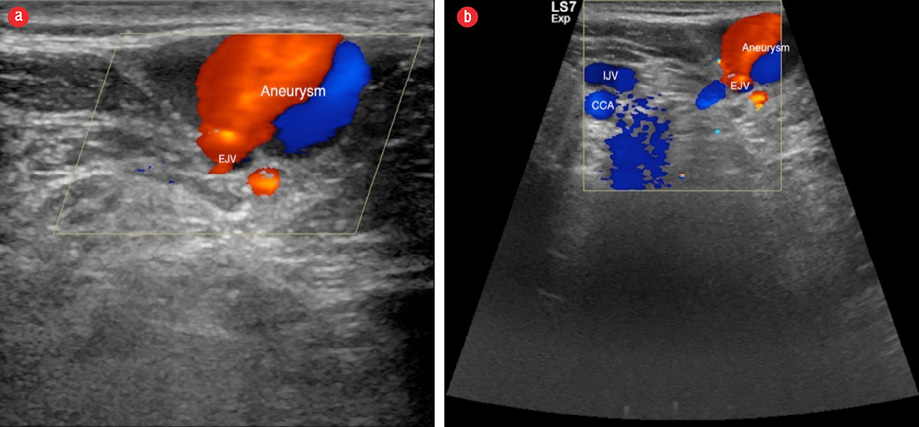
IJV: internal jugular vein; EJV: external jugular vein; CCA: common carotid artery.
Figure 3: (a) Color Doppler ultrasound (US) image of an external jugular vein aneurysm. (b) The lesion presented with venous flow on color Doppler US examination.
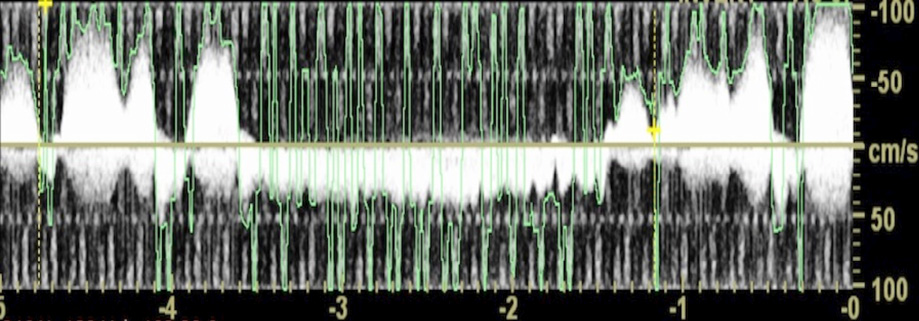
Figure 4: Spectral Doppler examination of an external jugular vein aneurysm. Spectral Doppler analysis of the lesion showed the venous waveform.
US examination revealed a 3 × 2 cm clear cystic compressible mass, which increased in size with Valsalva maneuver [Figure 2]. The lesion showed internal color flow and communicated with a short neck with the adjacent left external jugular vein [Figure 3]. Spectral Doppler analysis of the lesion showed the venous waveform [Figure 4]. These findings were suggestive of saccular venous aneurysm of the left external jugular vein.
Because there were no signs of thrombosis, rupture, thrombophlebitis, or pulmonary embolism, the patient was reassured and asked to attend regular follow-up.
Discussion
Venous aneurysms are rare clinical entity that were first described by Harris in 1928.14 Hischler suggested the term venous aneurysm similar to the arterial aneurysm.15 Venous aneurysms can involve any veins in the body, including cervical, thoracic, visceral, and upper and lower extremity veins. However, aneurysms of the neck are rare due to the low pressure in the superior vena caval system.3–6,12 Jugular vein aneurysms occur in the internal, external, and anterior jugular veins in decreasing order of frequency.1–9 External jugular vein aneurysm is rare, and very few cases have been reported in the English literature to date.
Venous aneurysms can be classified into primary (congenital) and acquired lesions.2–9,12 Primary venous aneurysms are true venous aneurysm because in these lesions the venous wall is intact.2,4,9 These lesions are usually fusiform in shape and frequently diagnosed in childhood.1,2,4,6,8 As for acquired aneurysms of the venous system, these lesions are usually saccular and result from changes in the cardiovascular system.1,2,4,6,8 Causative factors for an acquired venous aneurysm include tumors, inflammation, degeneration, or trauma. Sometimes they can appear spontaneously where no etiologic cause can be identified, as in our case.
Venous aneurysms of the neck can be confused for a variety of neck masses. Differential diagnosis in an adult includes lymph node enlargement, laryngocele, thyroid lesion, thyroglossal/dermoid/branchial cysts, lipoma, cavernous hemangioma, pharyngeal pouch, malignant transformation of a neck cyst, and metastases from squamous cell carcinoma.1–3,5–9,12,16
Clinically, by a careful physical examination, the definite diagnosis can often be accurately established. The clinical presentation of an external jugular vein aneurysm is usually a painless cervical swelling that may gradually increase in size. In the presence of a unilateral, non-tender, soft, and non-pulsatile swelling that enlarges with straining, sneezing, or Valsalva maneuver, one should be suspicious of a venous aneurysm.
The most important complications of venous aneurysms include thrombosis, thrombophlebitis, pulmonary thromboembolism, and rupture.3–5 Although these are rare, these risks should be taken into consideration. A recently documented reported of pulmonary thromboembolism caused by an aneurysm of the external jugular vein shows that these aneurysms may not be as innocent as previously thought.17 The authors of the report recommended mandatory surgical resection of the jugular vein aneurysm to prevent thromboembolic complications.
Surgical resection eliminates the theoretical risk of aneurismal rupture, pulmonary thromboembolism, and can confirm the histopathological diagnosis. However, some authors state that reassurance and regular follow-up can be appropriate for prompt treatment of an asymptomatic venous aneurysm unless there are cosmetic concerns, painful swelling due to intraluminal thrombosis, or phlebitis of the jugular vein. For example, Karapolat et al,18 suggested that surgery should be considered owing to the risk of thrombosis leading to pulmonary embolism and rupture. Other authors have suggested that surgery should be an option only for symptomatic and enlarging jugular aneurysms; otherwise, surgery should be recommended only for aneurysms of the abdomen and lower limb.19 One can conclude that large-scale studies are needed to overcome the limitations of rare case reports. Thus, all cases of venous aneurysm should be reported for further study.
The radiological investigations for diagnosis range from simple ultrasonogram to more sophisticated tools such as venography, CT angiography, and magnetic resonance angiography. US should be the first imaging technique performed, and it is often the only test needed to confirm the diagnosis because it can easily differentiate between cystic and solid masses, and vascular from non-vascular lesions. US can also delineate the borders of these lesions and establish the origin of the lesion from adjacent structures. CT angiography with digital subtraction angiography used to be the gold standard in the diagnosis of venous aneurysm of the neck,3 but US with Doppler imaging has replaced these costly invasive diagnostic tools as the investigation of choice for external jugular vein aneurysm.6,8,9,12,13
Conclusion
An external jugular venous aneurysm is an infrequent clinical entity and can present spontaneously as in our case. The importance of the case lies in the fact that one should remember this entity in the differential diagnosis of a cervical mass. US is the effective method of choice in the diagnosis of venous aneurysm of the neck. Surgical excision is advised for symptomatic aneurysms or esthetic reasons.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Drakonaki EE, Symvoulakis EK, Fachouridi A, Kounalakis D, Tsafantakis E. External jugular vein aneurysm presenting as a cervical mass. Int J Otolaryngol 2011;2011:485293.
- 2. Aiyappan SK, Ranga U, Veeraiyan S. Aneurysm of external jugular vein mimicking hemangioma of neck. Indian J Surg 2013 Dec;75(6):493-495.
- 3. Verma RK, Kaushal D, Panda NK. External jugular vein aneurysm with thrombus presenting as painful neck mass: a case report. Oman Med J 2013 Jul;28(4):278-280.
- 4. Kim SW, Chang JW, Lee S. Unusual presentation of a cervical mass revealed as external jugular venous aneurysm. Vasc Specialist Int 2016 Dec;32(4):205-207.
- 5. Neto T, Balhau R, Coelho L, Pinto I, Correia-Sá I, Silva Á. Thrombosed aneurysm of the external jugular vein: a rare cause of cervical mass. J Craniofac Surg 2016 Jan;27(1):e36-e37.
- 6. Mohanty D, Jain BK, Garg PK, Tandon A. External jugular venous aneurysm: a clinical curiosity. J Nat Sci Biol Med 2013 Jan;4(1):223-225.
- 7. Swaika S, Basu S, Bhadra RC, Maitra S. Multiple venous aneurysms of neck. J Indian Assoc Pediatr Surg 2013 Jan;18(1):25-26.
- 8. Lee HY, Cho SH, Ko TY, Kim HS, Kim JI, Park SD, et al. Saccular aneurysm of the external jugular vein: a case report. Korean J Thorac Cardiovasc Surg 2014 Apr;47(2):171-173.
- 9. Al-Shaikhi A, Kay S, Laberge JM. External jugular venous aneurysm: an unusual cause of a neck mass in a young child. J Pediatr Surg 2003 Oct;38(10):1557-1559.
- 10. Suchý T. [Venous aneurysms]. Rozhl Chir 1995 Sep;74(6):284-286.
- 11. Porcellini M, Selvetella L, Bernardo B, Del Guercio L, Baldassarre M. [Aneurysms of the external jugular vein]. G Chir 1996 May;17(5):238-241.
- 12. Grigorescu I, Dumitraşcu DL, Manole S, Fodor D. Pseudoaneurysma of the external jugular vein communicating with the internal jugular vein. Case report. Med Ultrason 2012 Sep;14(3):257-260.
- 13. Verbeeck N, Hammer F, Goffette P, Mathurin P. Saccular aneurysm of the external jugular vein, an unusual cause of neck swelling. J Belge Radiol 1997 Apr;80(2):63-64.
- 14. Harris RI. Congenital venous cyst of mediastinum. Ann Surg 1928;88:953-956.
- 15. Hilscher WM. Zur frage der venosen aneurysmen. Fortscher Röntgenstr 1955;82:244-247.
- 16. Kirmani S, Rashid M, Ali I, Badar F. External jugular vein aneurysm: a rare cause of neck swelling. J Ultrasound Med 2011 Aug;30(8):1157-1158.
- 17. Ioannou CV, Kostas T, Tsetis D, Georgakarakos E, Gionis M, Katsamouris AN. External jugular vein aneurysm: a source of thrombotic complications. Int Angiol 2010 Jun;29(3):284-285.
- 18. Karapolat S, Erkut B, Unlu Y. Multiple aneurysms of the left external jugular vein. Turk J Med Sci 2005;35(1):43-45.
- 19. Calligaro KD, Ahmad S, Dandora R, Dougherty MJ, Savarese RP, Doerr KJ, et al. Venous aneurysms: surgical indications and review of the literature. Surgery 1995 Jan;117(1):1-6.